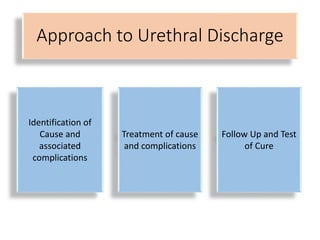
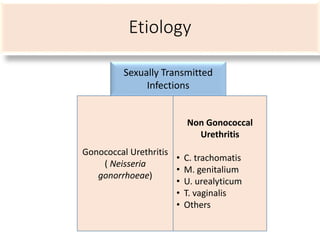
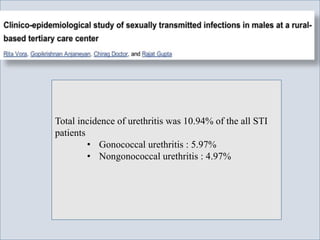
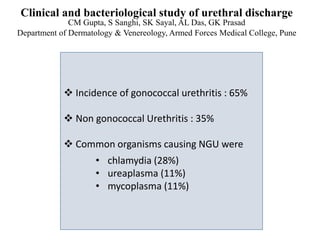
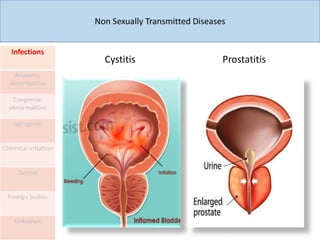
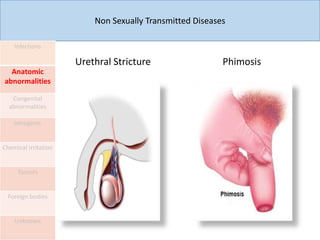
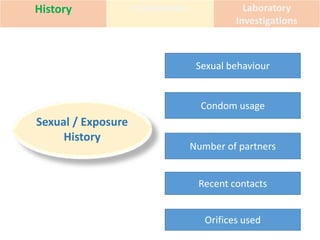
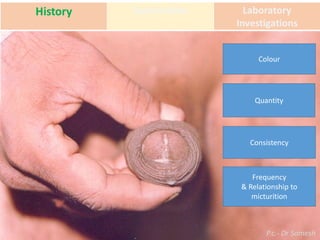
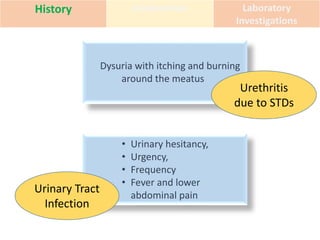
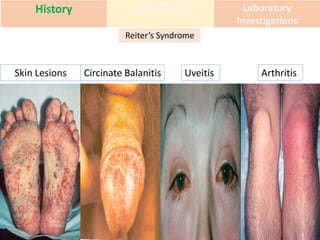
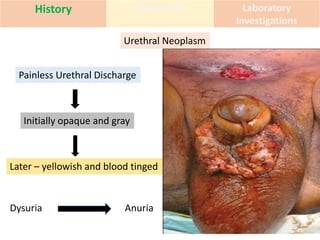
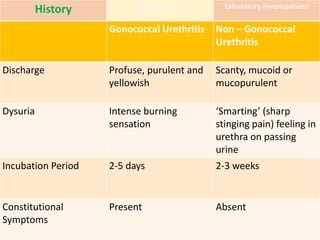
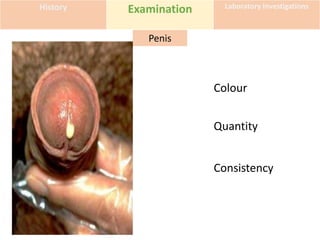
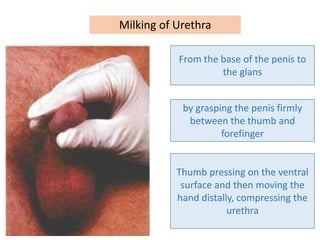
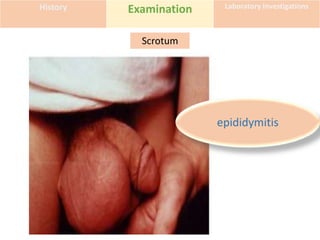
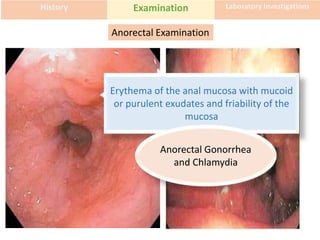
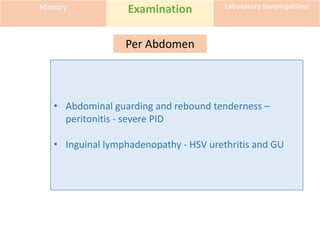
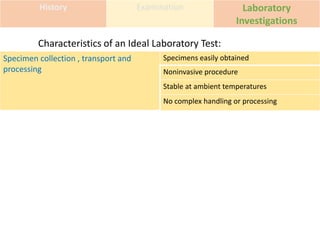
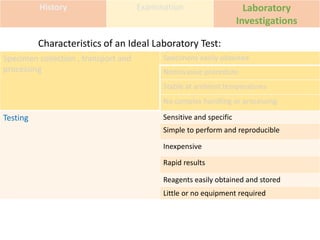
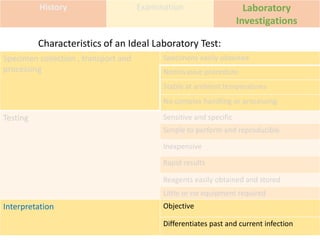
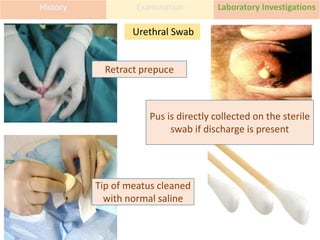
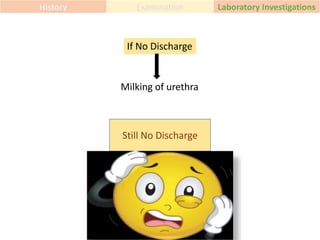
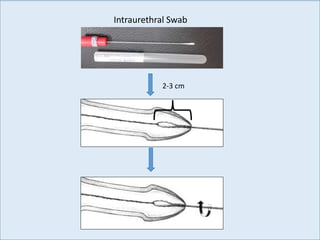
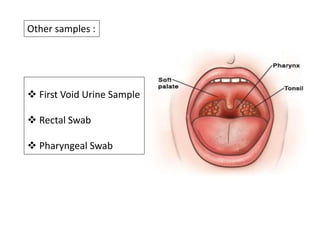
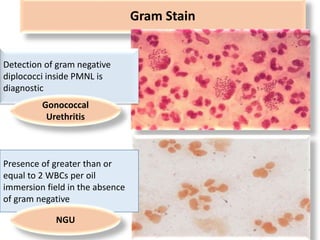
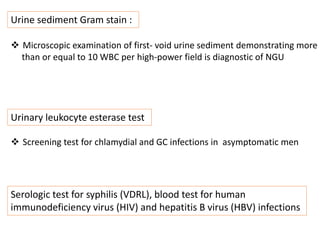
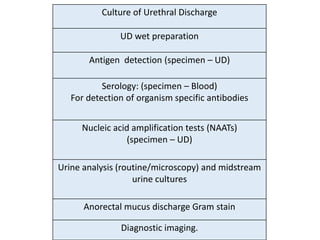
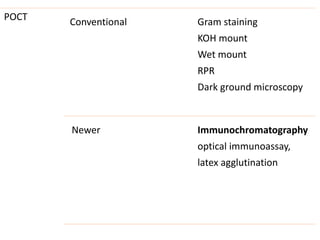
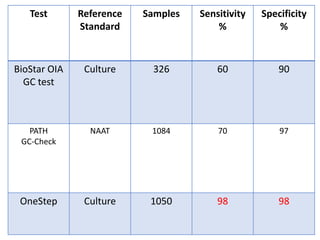
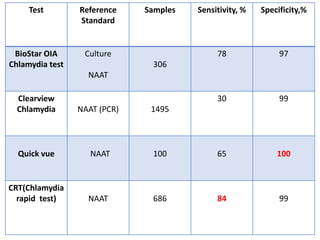
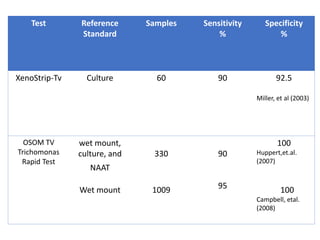
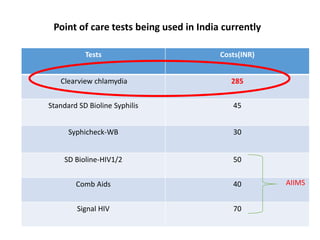
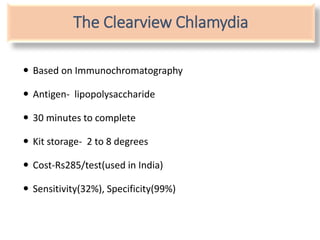
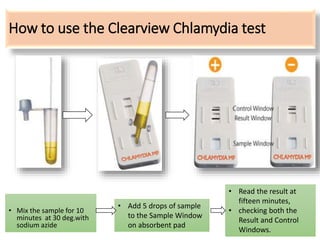
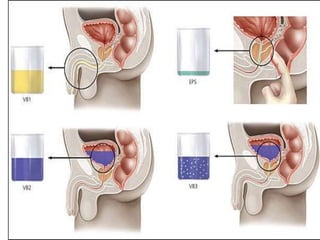
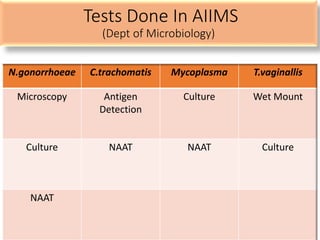
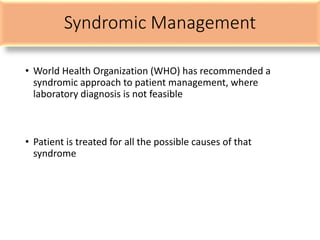
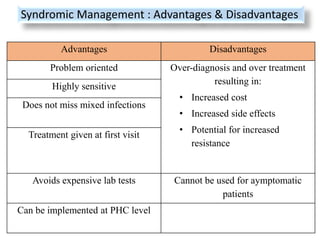
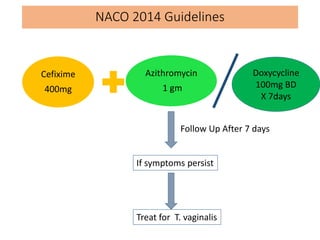
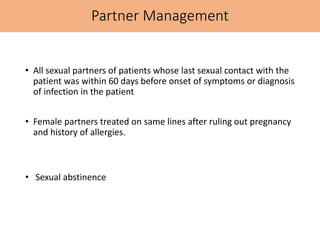
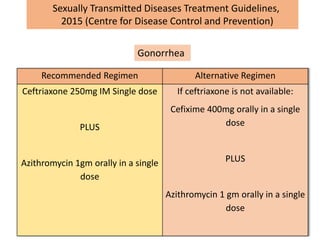
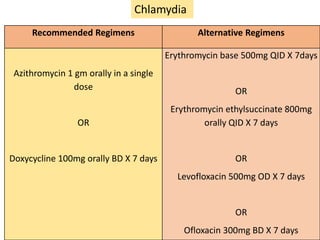
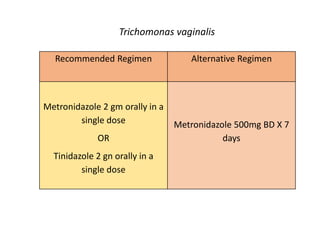
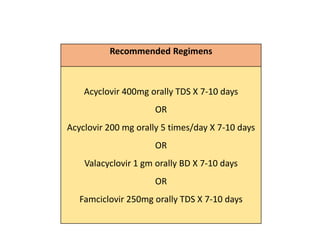
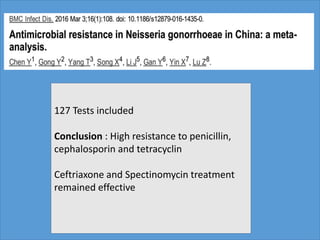
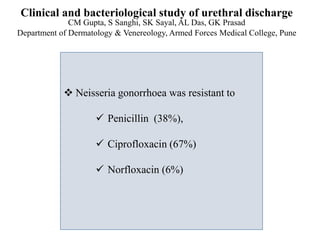
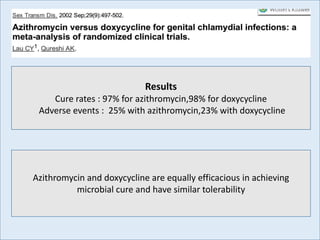
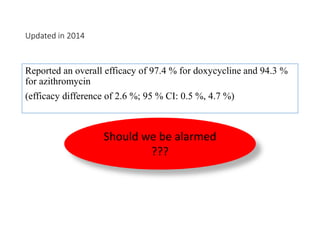
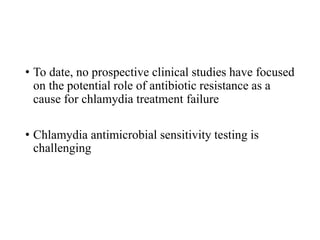
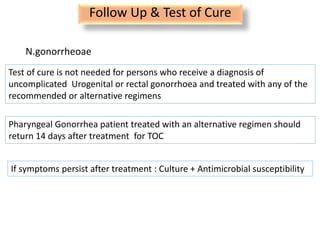
This document discusses the approach to evaluating and treating urethral discharge. It begins by outlining the common causes of urethral discharge including sexually transmitted infections like gonorrhea and chlamydia as well as non-sexually transmitted infections. It then describes the evaluation process including history, examination, laboratory investigations, and treatment guidelines. Evaluation involves identifying the cause through history, examination, testing urethral or urine samples, and treating based on identified causes. Common tests discussed include gram stain, culture, and point of care tests while recommended treatments follow guidelines. Drug resistance and follow up are also addressed.