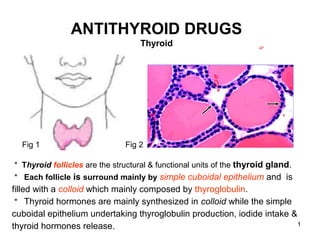
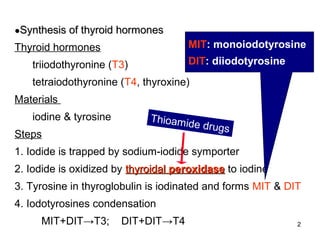
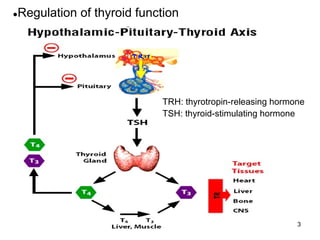
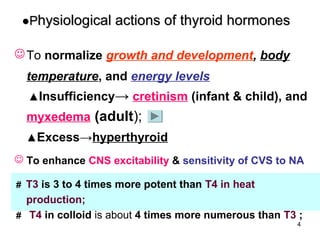
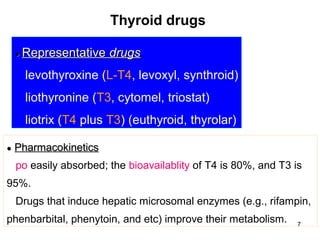
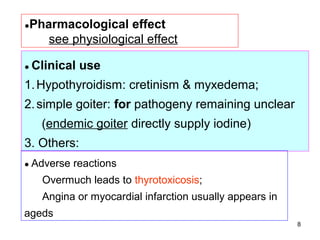
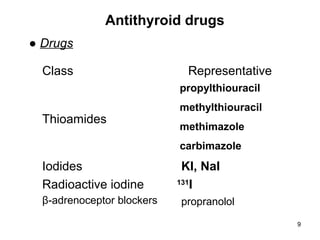
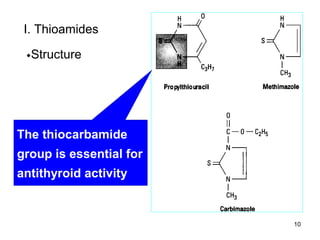
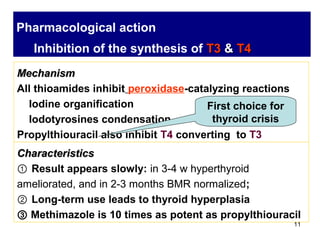
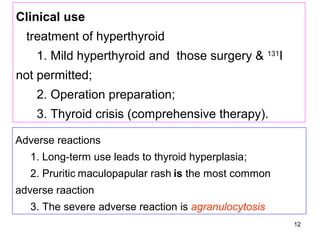
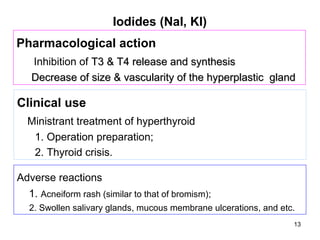
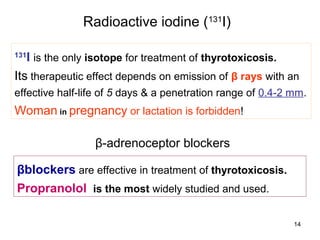
The document discusses antithyroid drugs used to treat hyperthyroidism. It describes the thyroid gland's structure and hormone synthesis process. The main antithyroid drug classes discussed are thioamides like methimazole and propylthiouracil, which inhibit thyroid hormone synthesis. Iodides like potassium iodide decrease thyroid hormone release and synthesis. Radioactive iodine-131 treatment depends on beta ray emission to destroy thyroid tissue. Beta-blockers like propranolol are also used to treat hyperthyroidism symptoms.