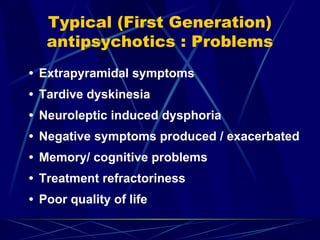
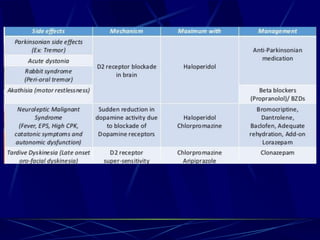
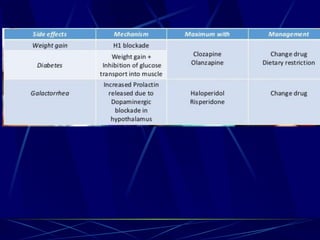
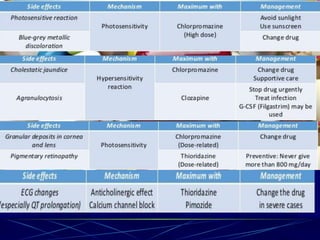
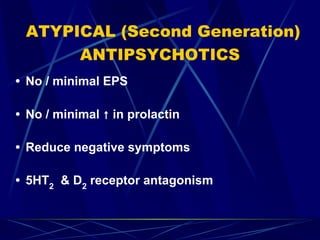
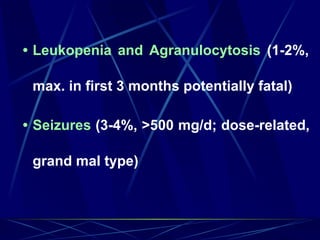
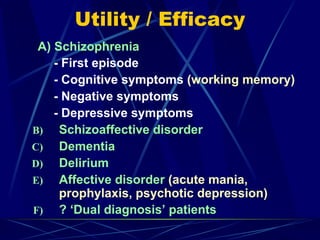
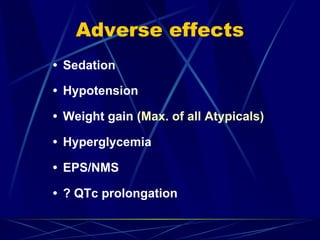
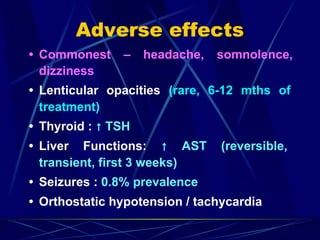
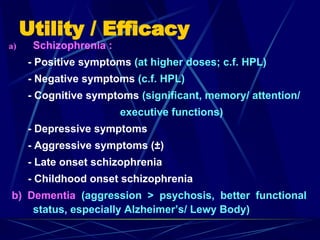
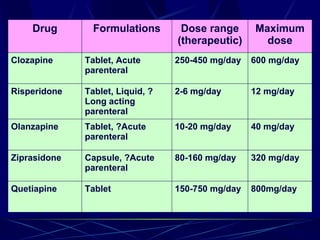
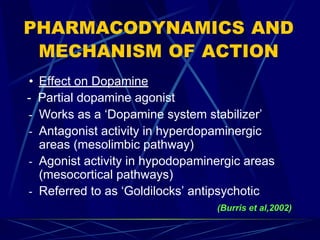
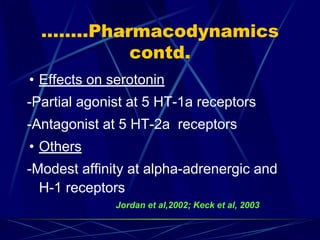
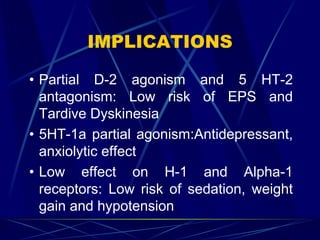
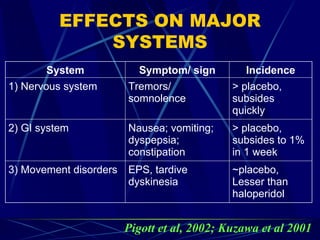
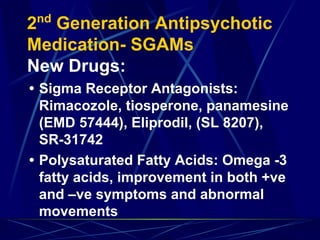
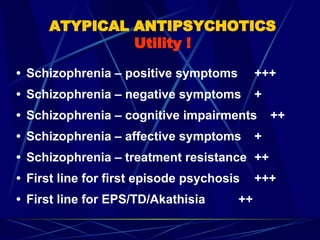
Typical antipsychotics are associated with extrapyramidal side effects and tardive dyskinesia. Atypical antipsychotics have fewer of these motor side effects due to their serotonin receptor antagonism. Clozapine is effective for treatment-resistant schizophrenia but carries risks of agranulocytosis and seizures. Newer atypicals like risperidone, olanzapine, and quetiapine have fewer motor side effects than typicals but can cause weight gain, hyperglycemia, and metabolic side effects. Aripiprazole is a partial dopamine agonist that has low risks of motor and metabolic side effects.