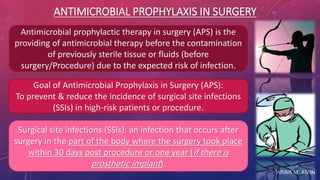
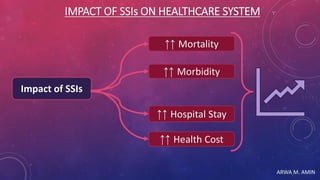
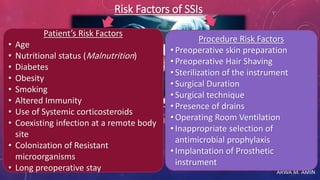
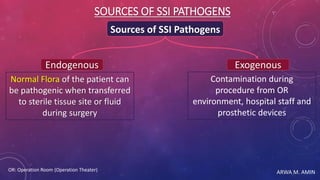
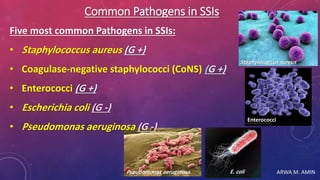
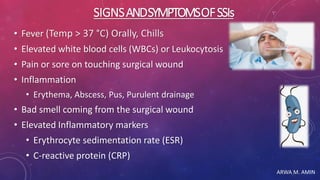
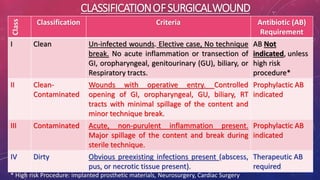
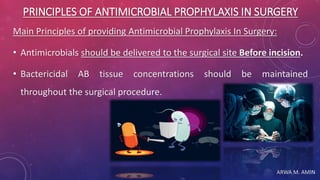
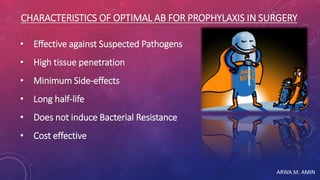
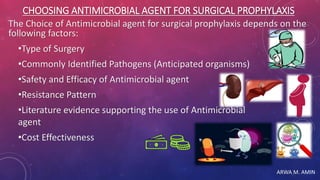
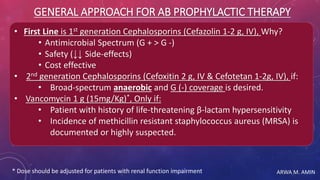
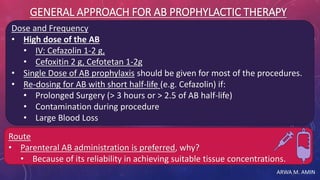
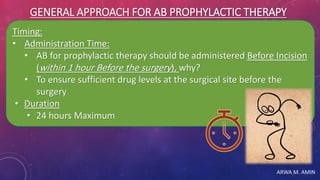
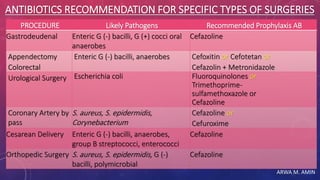
The document discusses antimicrobial prophylaxis in surgery (APS), which aims to prevent surgical site infections (SSIs) by administering antimicrobial therapy before surgery. It outlines the impact of SSIs on healthcare, their classification, risk factors, common pathogens, and principles for effective APS, including the choice of antimicrobial agents based on specific surgical procedures. Additionally, it provides strategies for implementing appropriate APS practices in healthcare institutions.