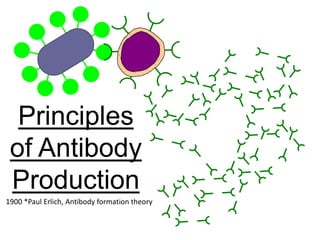
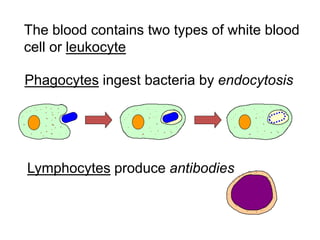
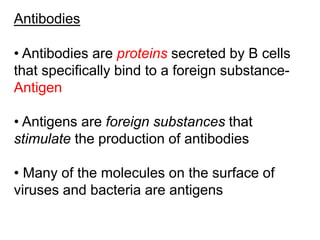
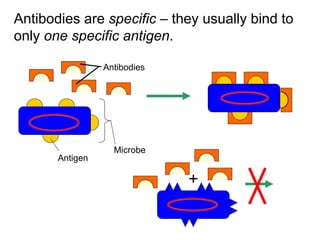
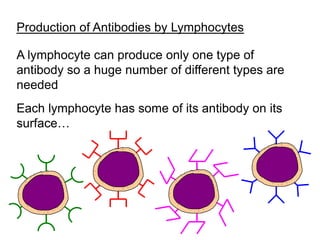
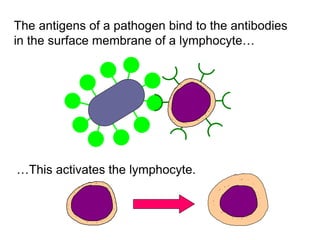
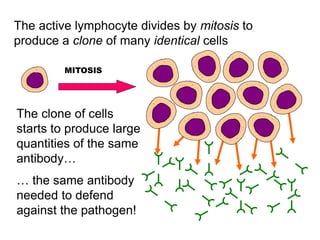
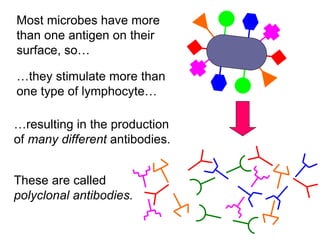
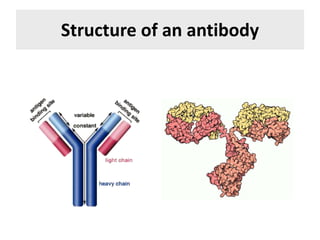
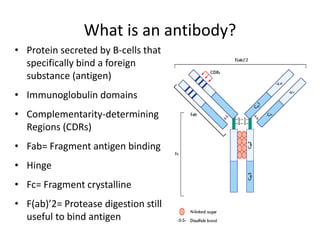
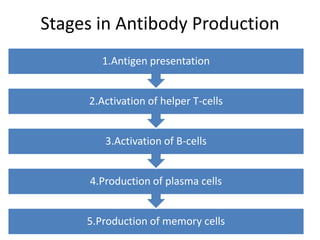
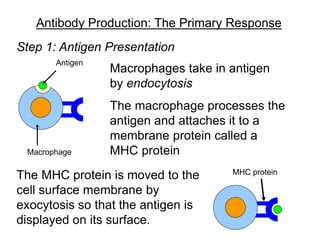
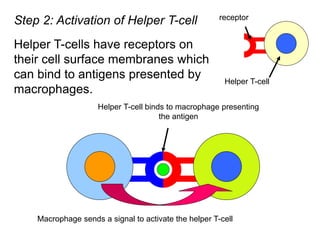
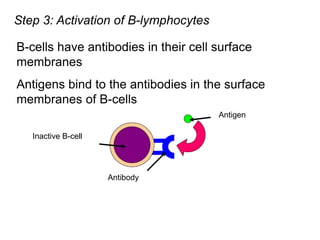
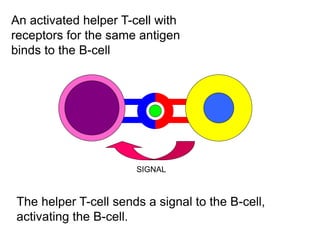
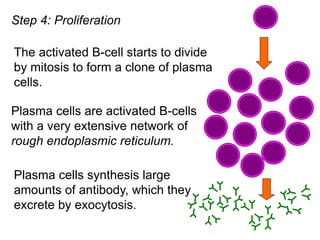
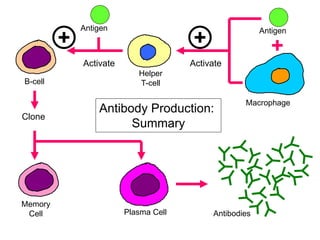
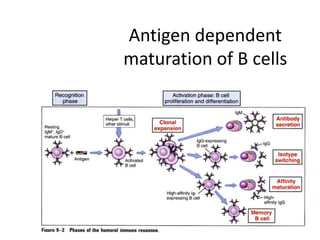
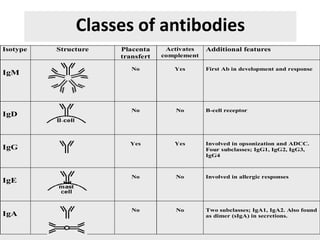
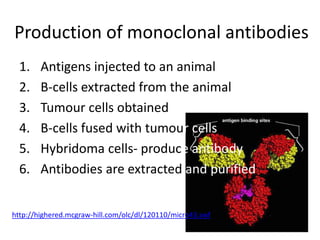
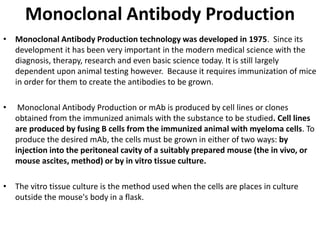
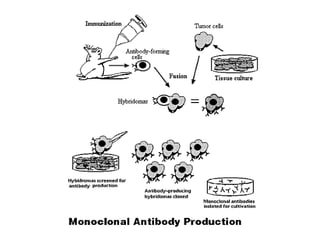
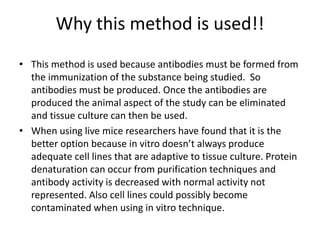
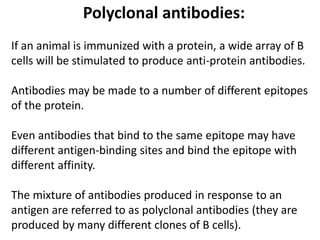
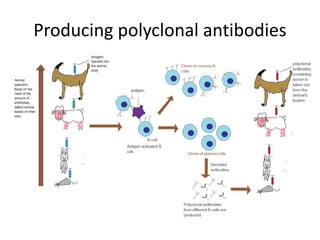
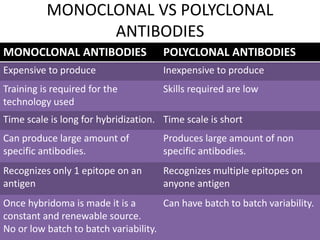
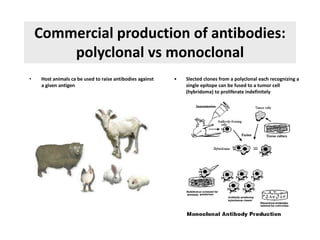
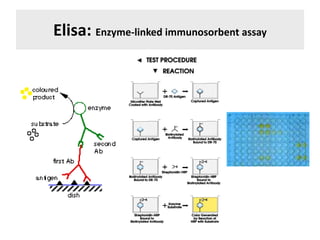
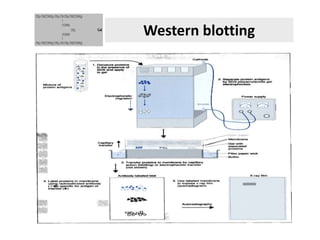
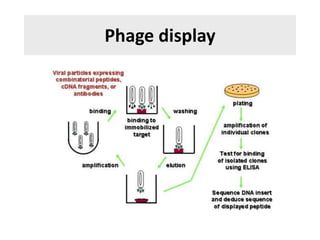
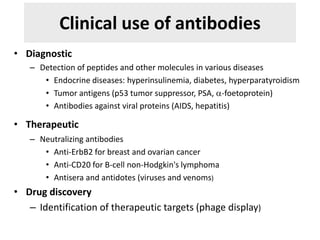
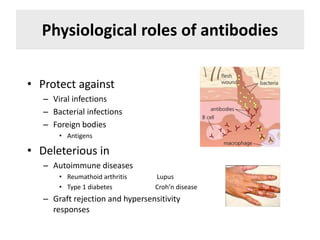
The document discusses the principles of antibody production, including how antibodies are produced by B cells in response to antigens, the process of antibody production including antigen presentation, activation of helper T cells and B cells, proliferation of plasma cells, and the role of memory cells in the secondary response. It also covers the structure and classes of antibodies, as well as the production and uses of monoclonal and polyclonal antibodies in research, diagnosis and therapy.