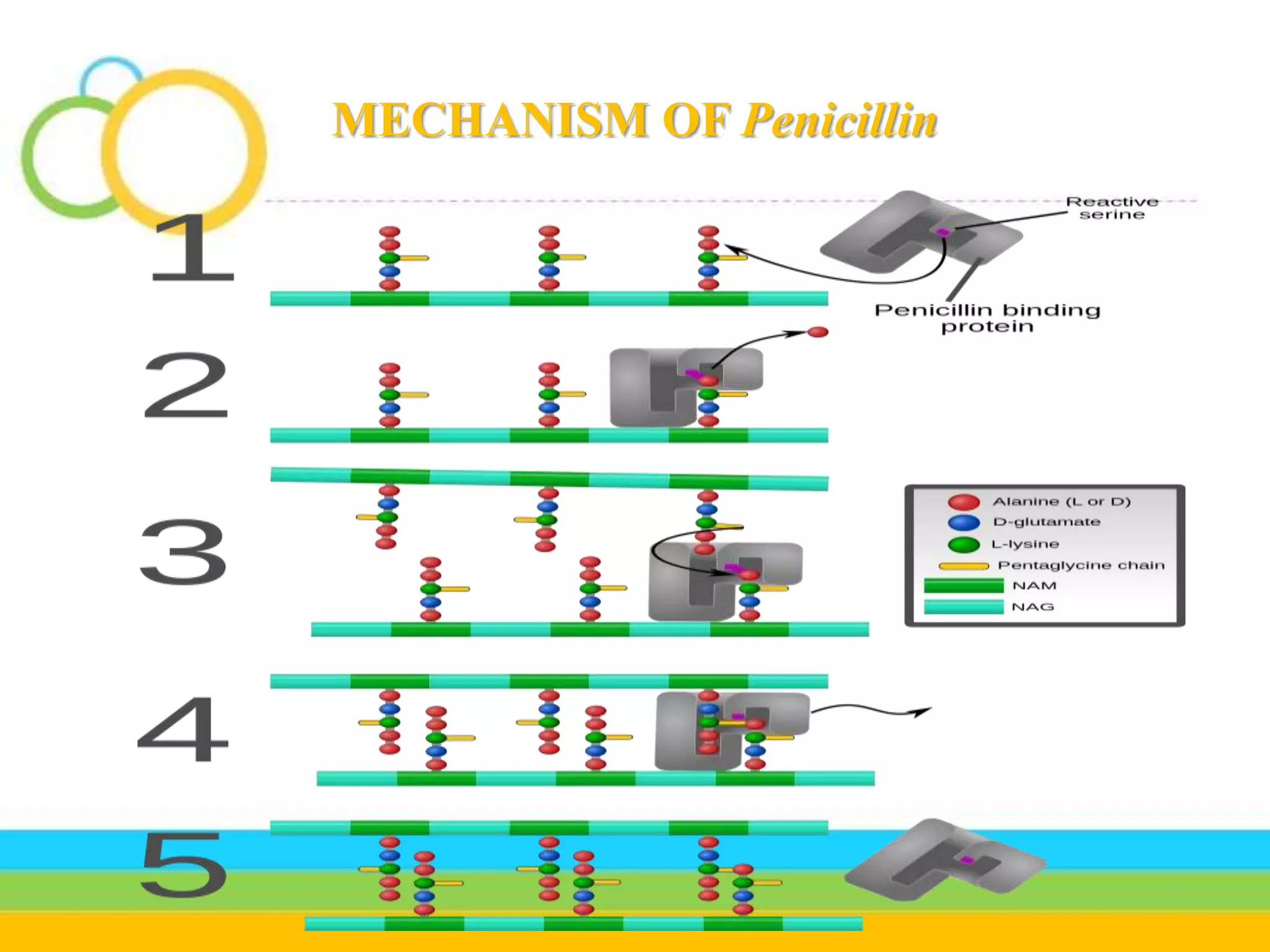
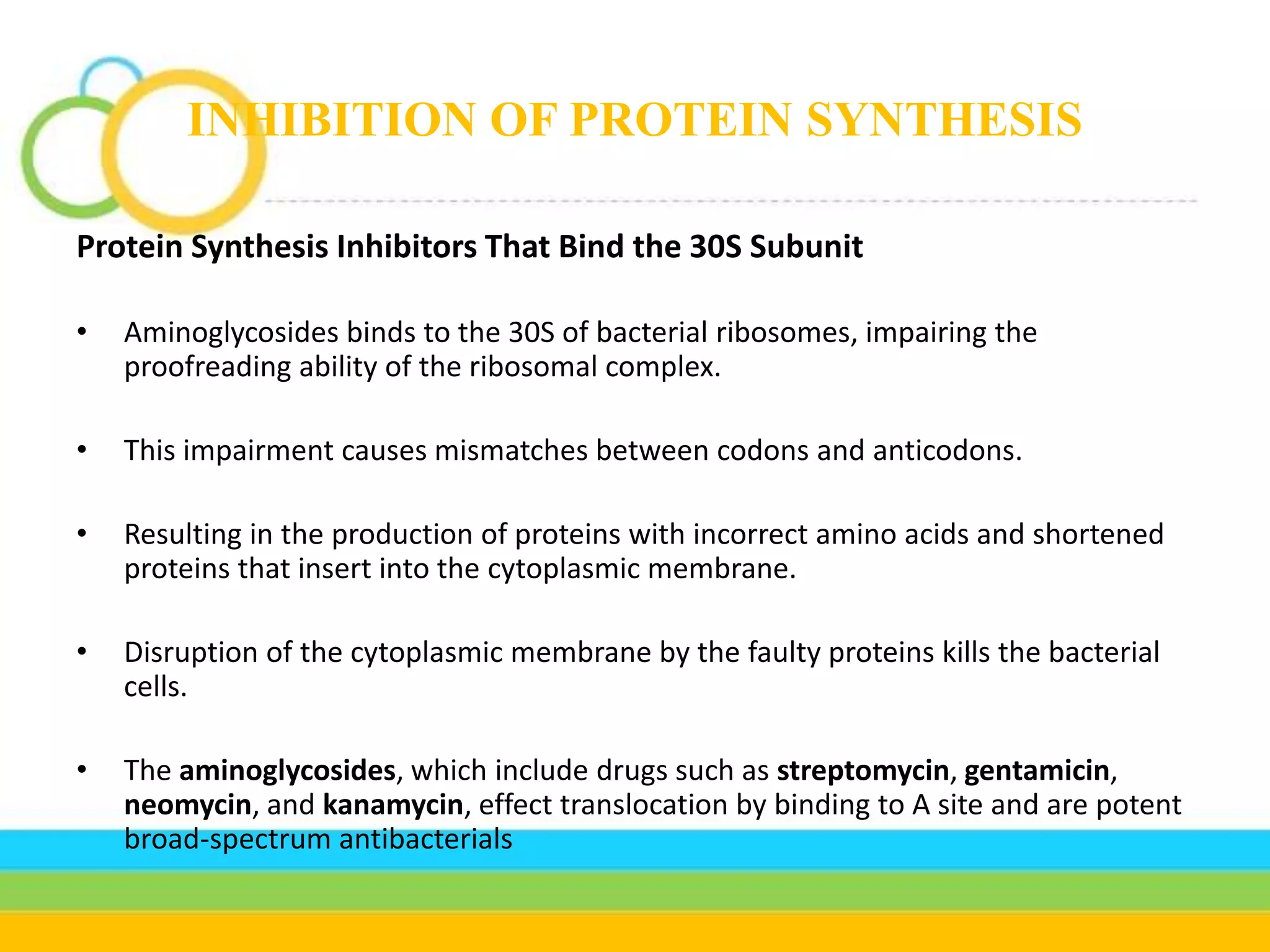
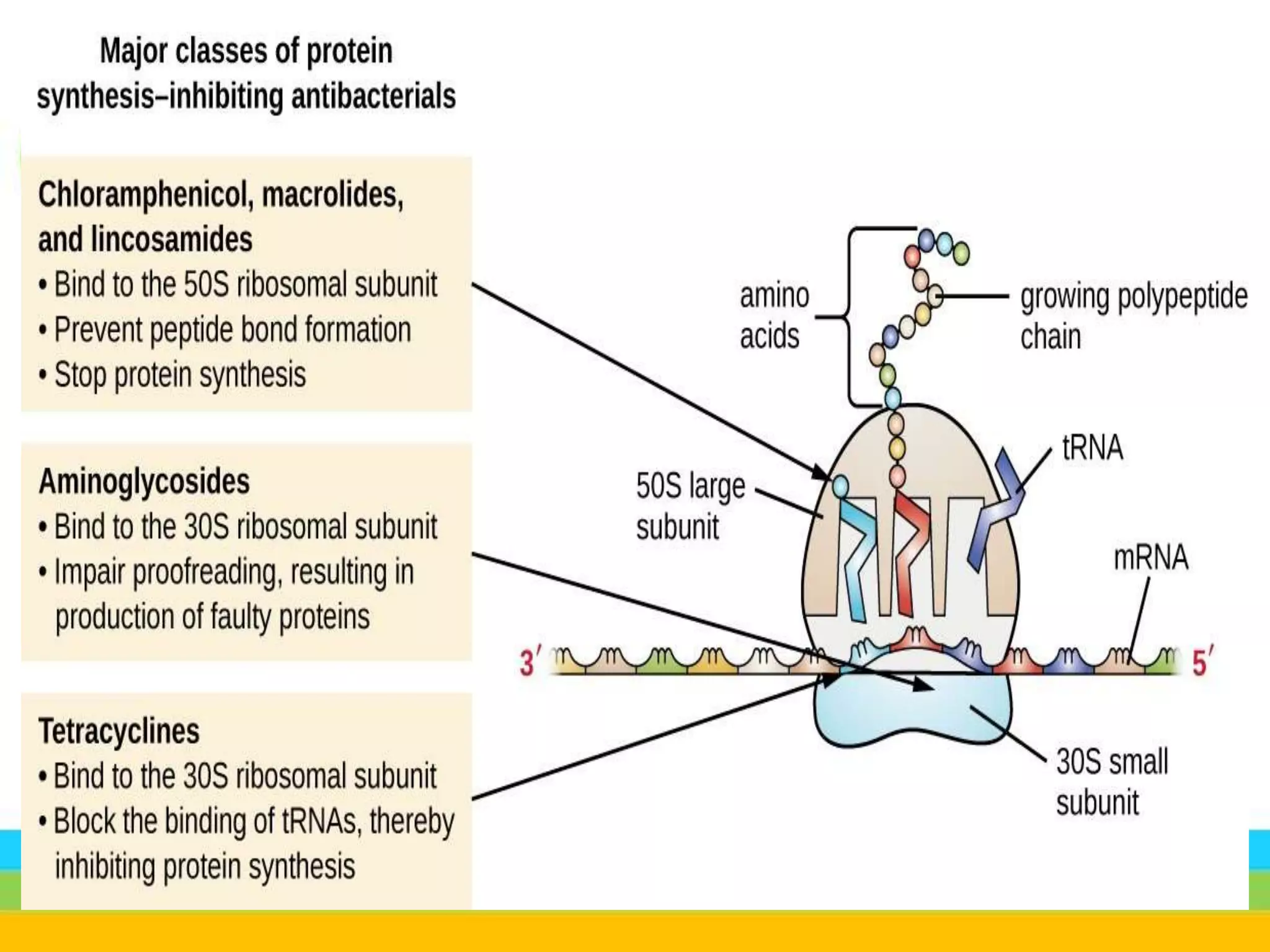
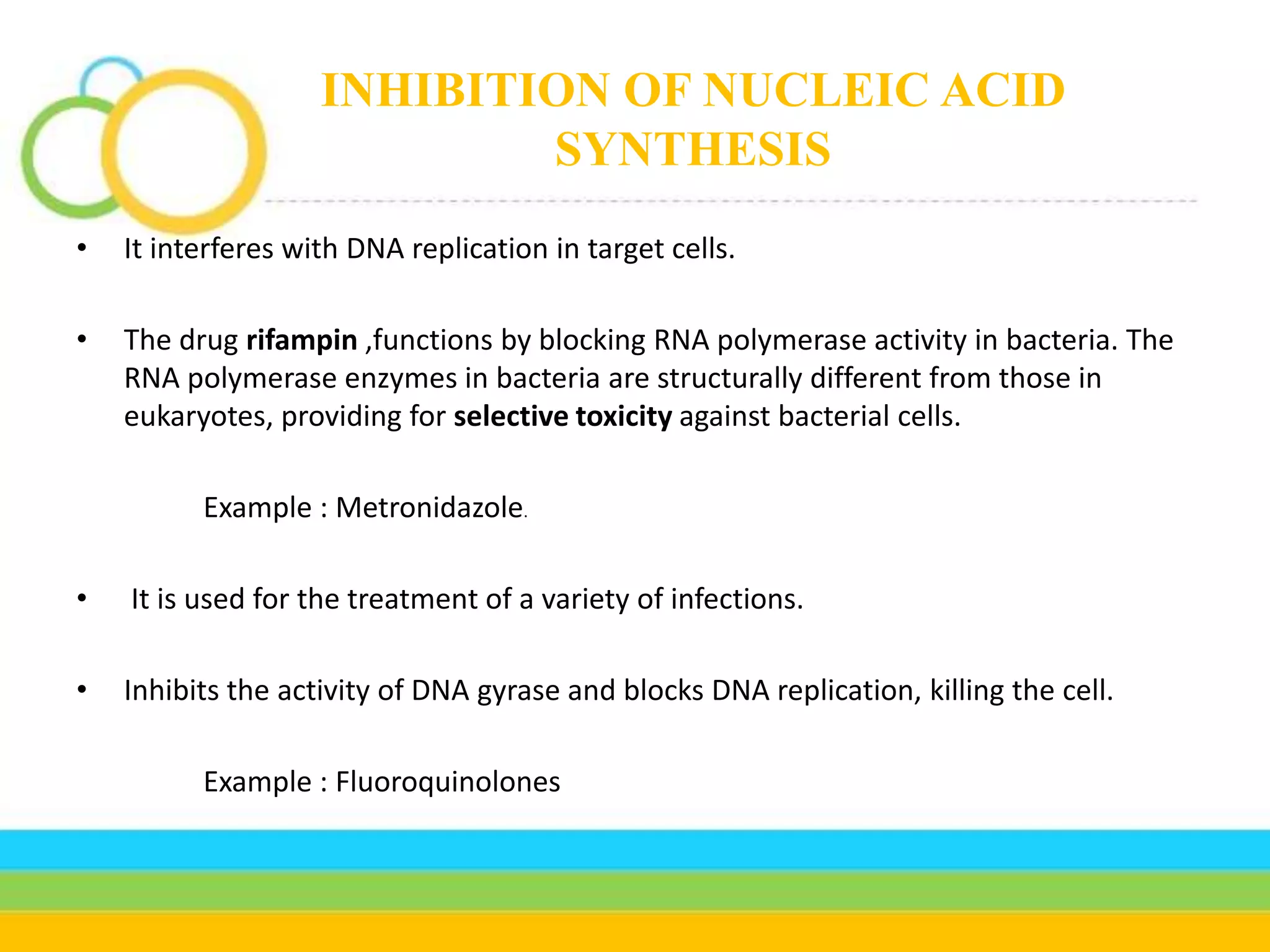
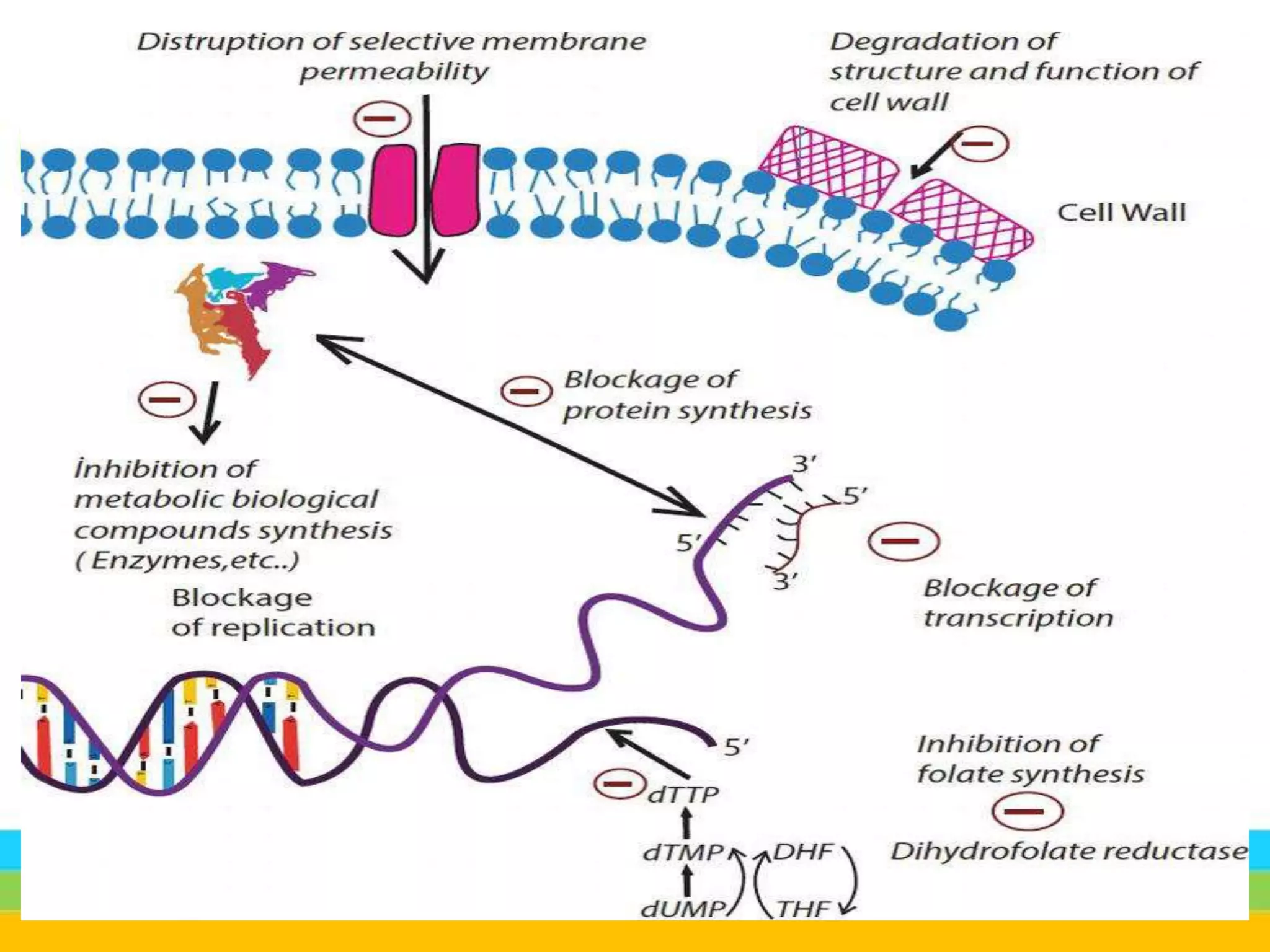
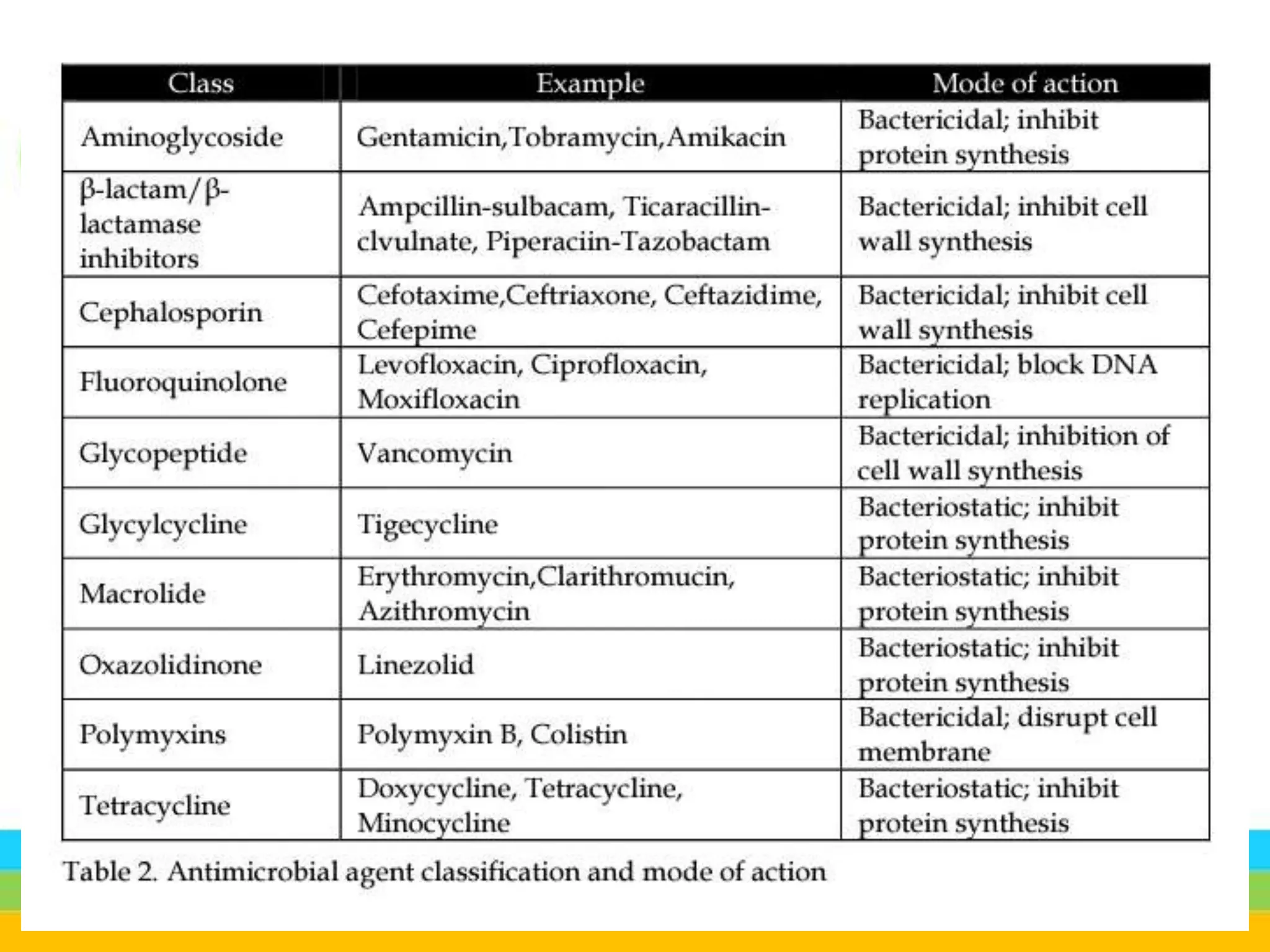
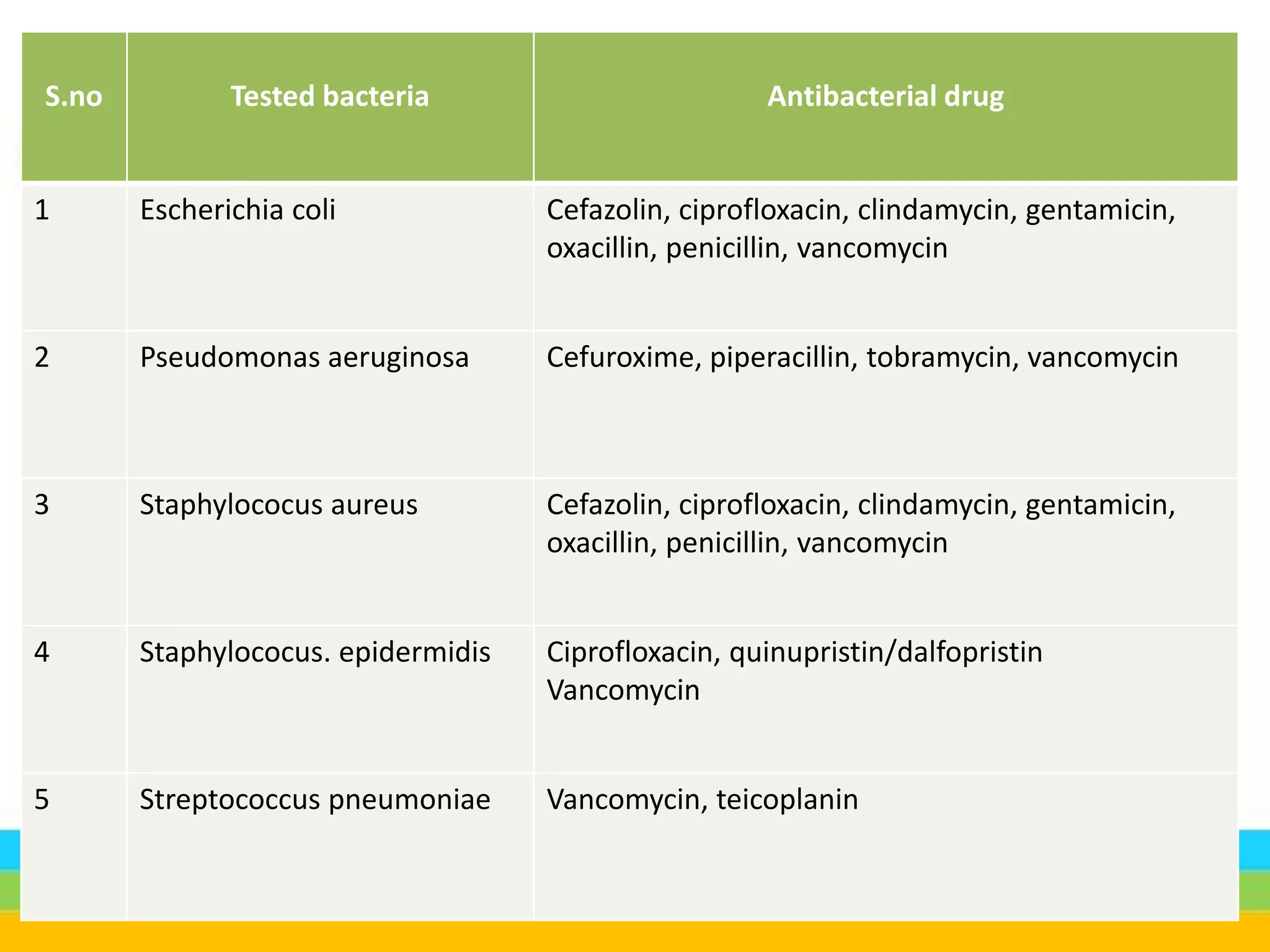
The document describes antibacterial agents, which interfere with bacterial growth and reproduction, and can be classified into bactericidal and bacteriostatic categories based on their action. It outlines the mechanisms of action for various antibiotics, detailing how they target bacterial cell walls, protein synthesis, nucleic acids, and metabolic pathways. Additionally, it discusses the advantages and disadvantages of antibiotics, highlighting issues like side effects and antibiotic resistance.