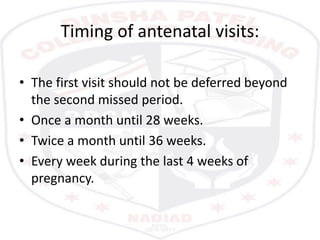
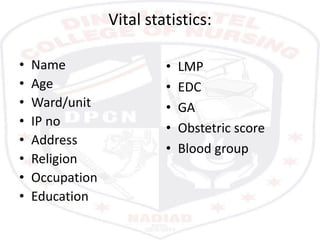
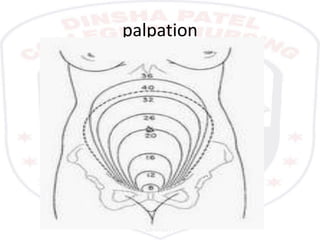
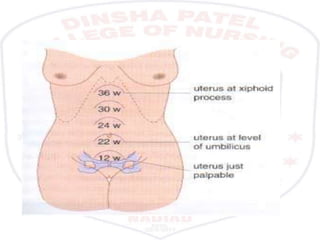
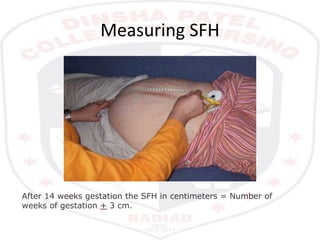
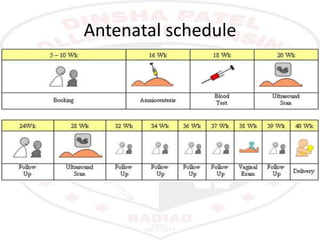
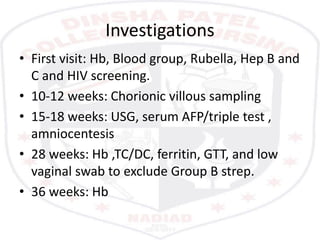
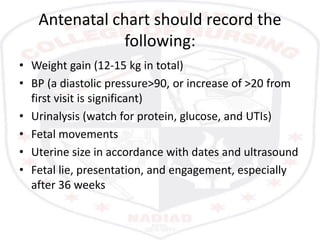
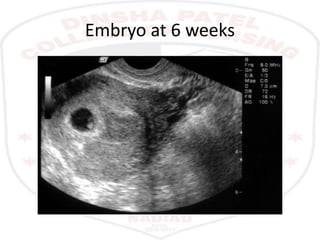
Antenatal assessment involves a systematic evaluation of a pregnant woman to monitor her health and the health of the fetus. It includes a comprehensive history, physical and pelvic examinations, lab tests, and procedures like ultrasound and amniocentesis. The assessment identifies risk factors, monitors fetal growth and well-being, and educates the woman. Regular antenatal visits provide ongoing monitoring throughout the stages of pregnancy.