1. The document outlines preoperative investigations and assessments that should be performed for patients undergoing surgery based on their age, medical history, type of surgery, and other risk factors.
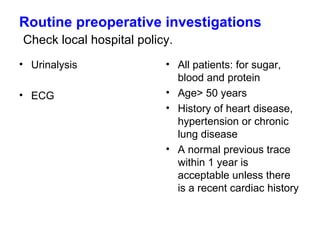
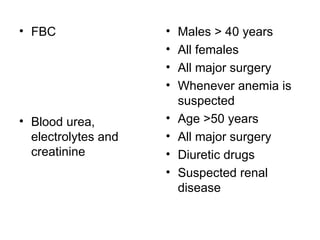
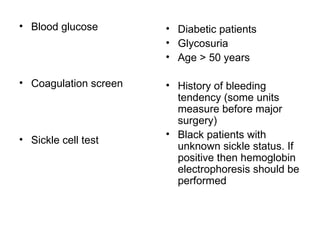
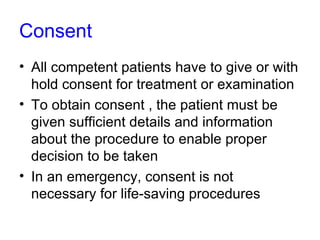
2. Key details include routine tests like urinalysis, ECG, and blood tests, as well as ensuring patient consent is obtained by explaining the procedure, risks, and alternatives.
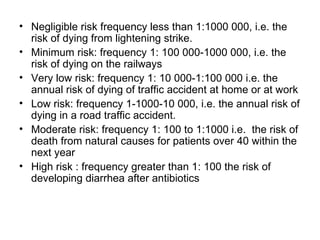
3. Risks are defined on a scale from negligible to high based on their frequency and severity, and patient competence and physical status are also assessed.