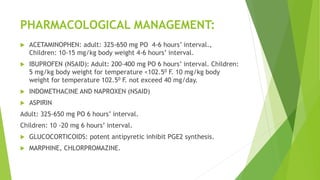
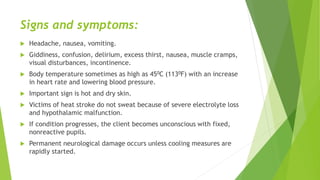
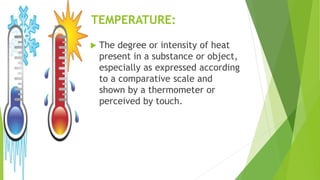
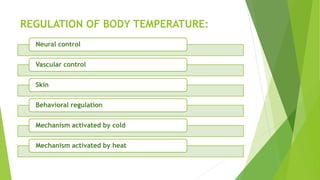
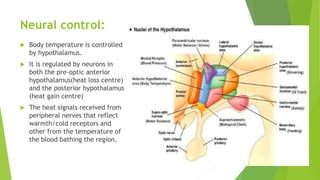
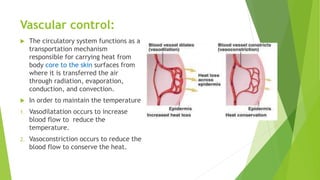
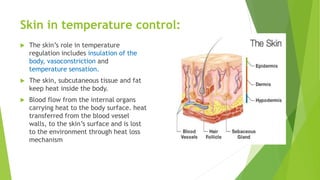
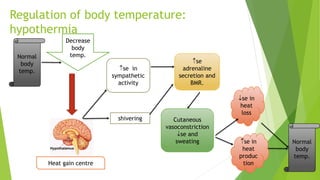
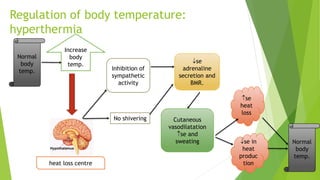
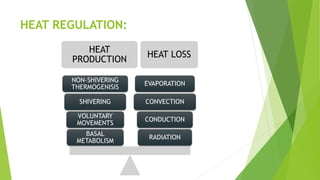
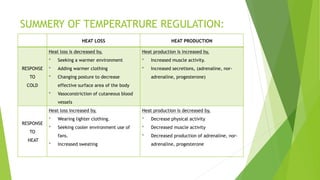
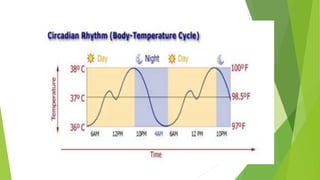
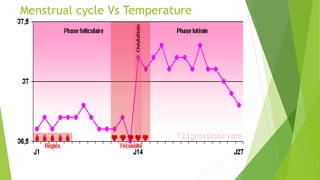
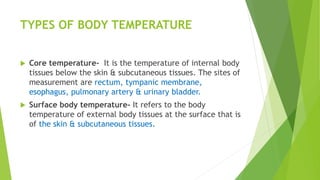
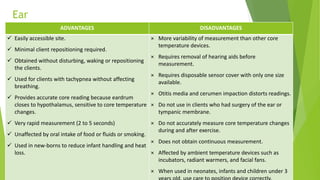
The document discusses body temperature regulation and factors that can alter it. It defines key terms like thermogenesis, thermolyis, basal metabolic rate, and circadian rhythm. It describes the normal ranges for oral, rectal, tympanic, and axillary temperatures. Temperature is regulated by the hypothalamus through neural control of the circulatory system, skin, and behavioral responses. Mechanisms for heat production include basal metabolism, movement, shivering, and non-shivering thermogenesis. Heat is lost through radiation, conduction, convection, and evaporation. The document summarizes how the body responds to cold with heat production and responses to heat with increased heat loss.
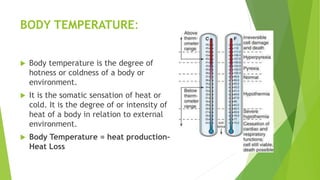
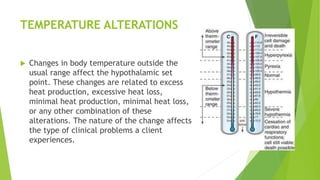






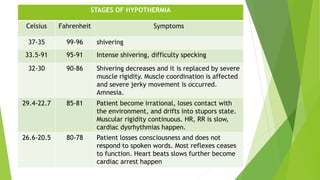
![Altered body
temperature
(37°C/ 98.6°F)
Increased body
temperature
(38°C/99°F)
[hyperthermia]
Fever (39°C/102.2°F)
Hyperthermia
(uncontrolled increase of
temperature)
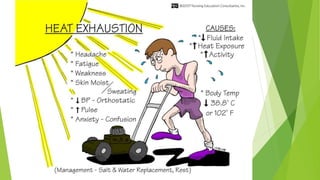
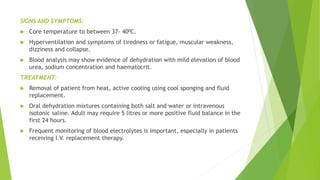
Heat exhaustion
(40°C/104°F)
Heat cramps
Heat stroke (40°C/104°F)
decreased body
temperature
(35°C/95°F)
[hypothermia]
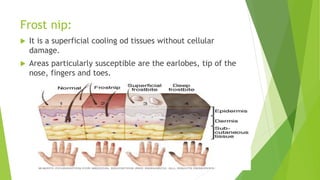
Frost nip (superficial
ulcers)
Frost bite (tissue
temperature below 0°C)
Death due to freezing (-
35°C)](https://image.slidesharecdn.com/alteredbodytemperature-190108162821/85/Altered-body-temperature-50-320.jpg)