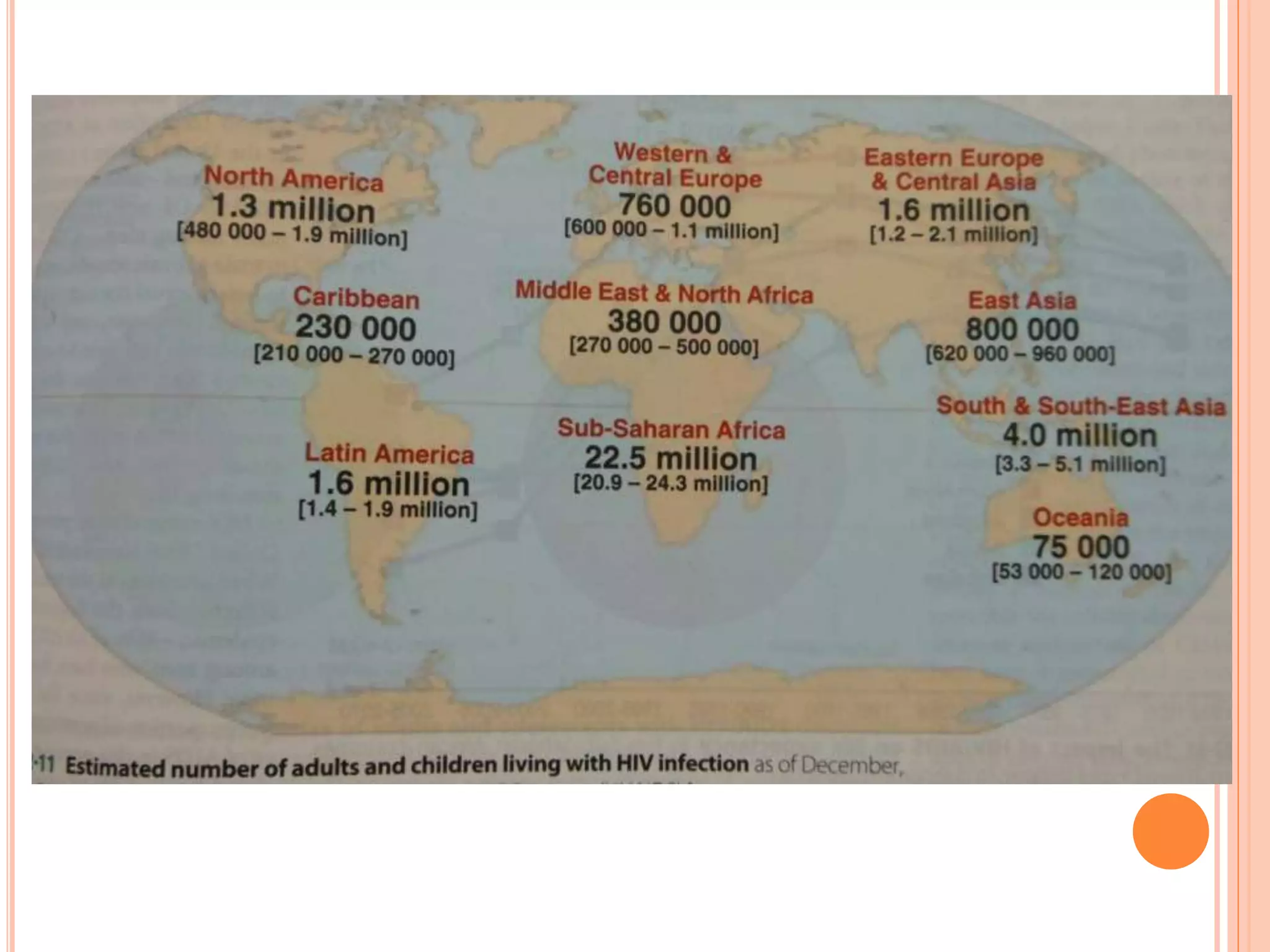
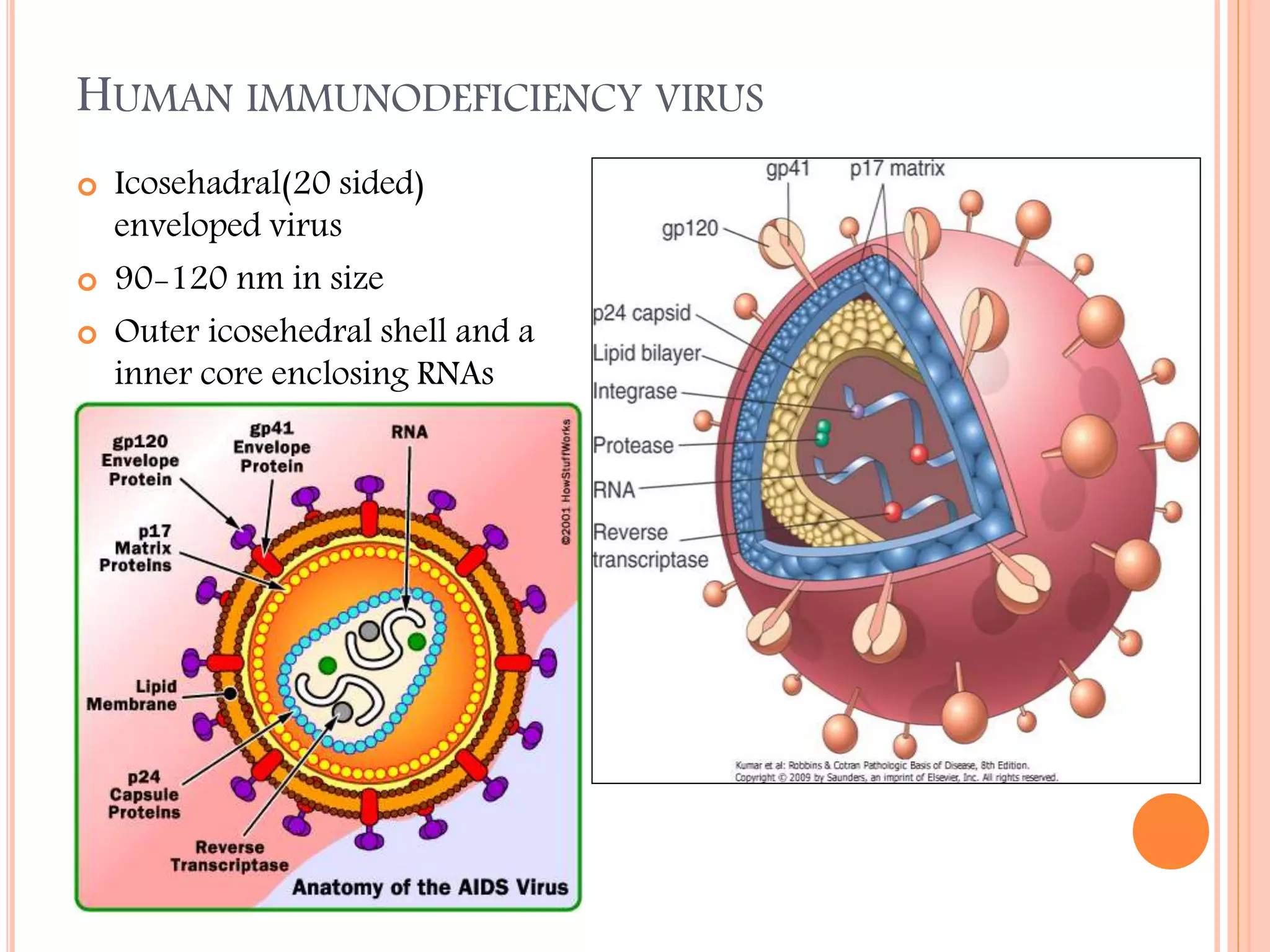
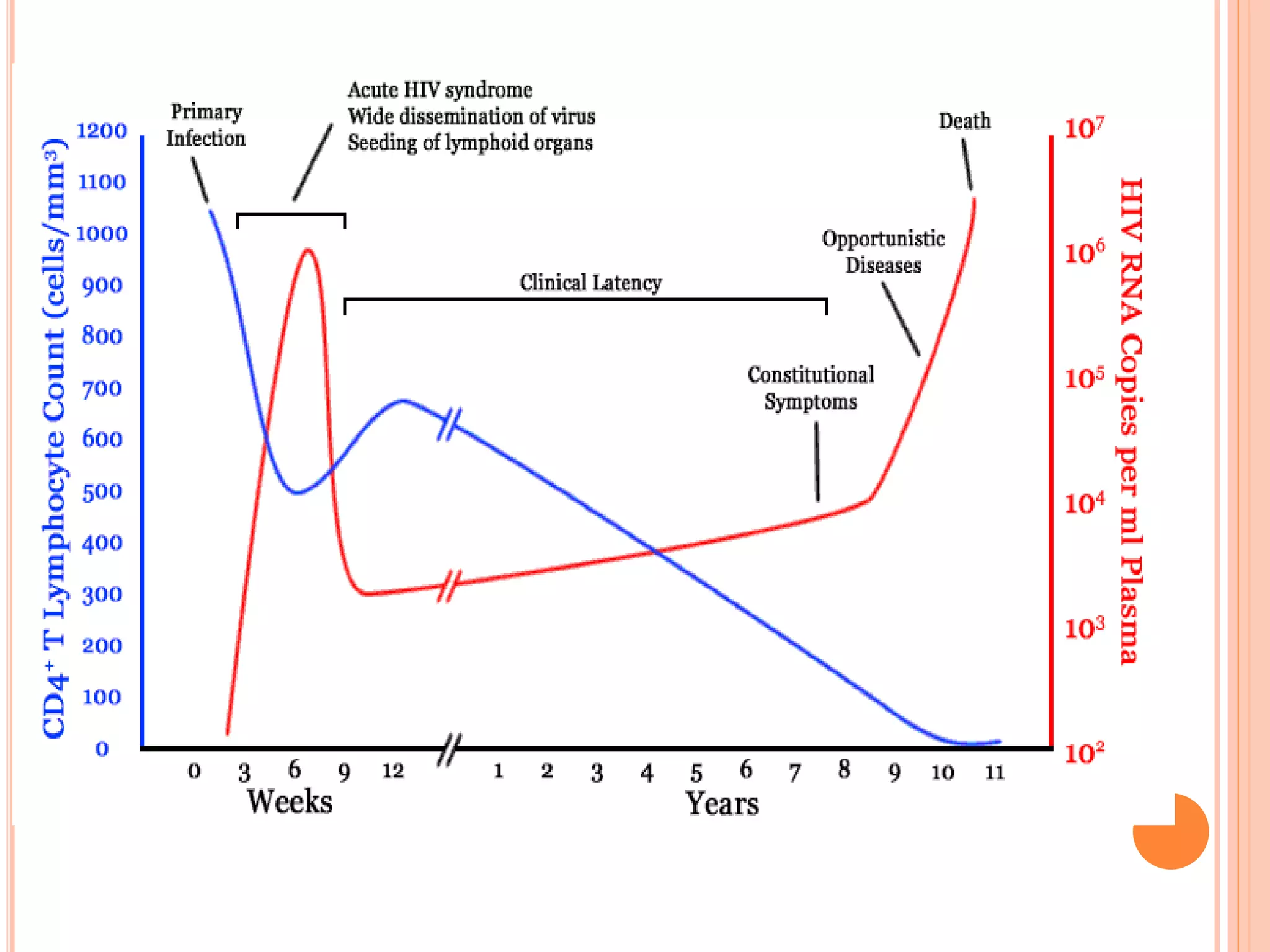
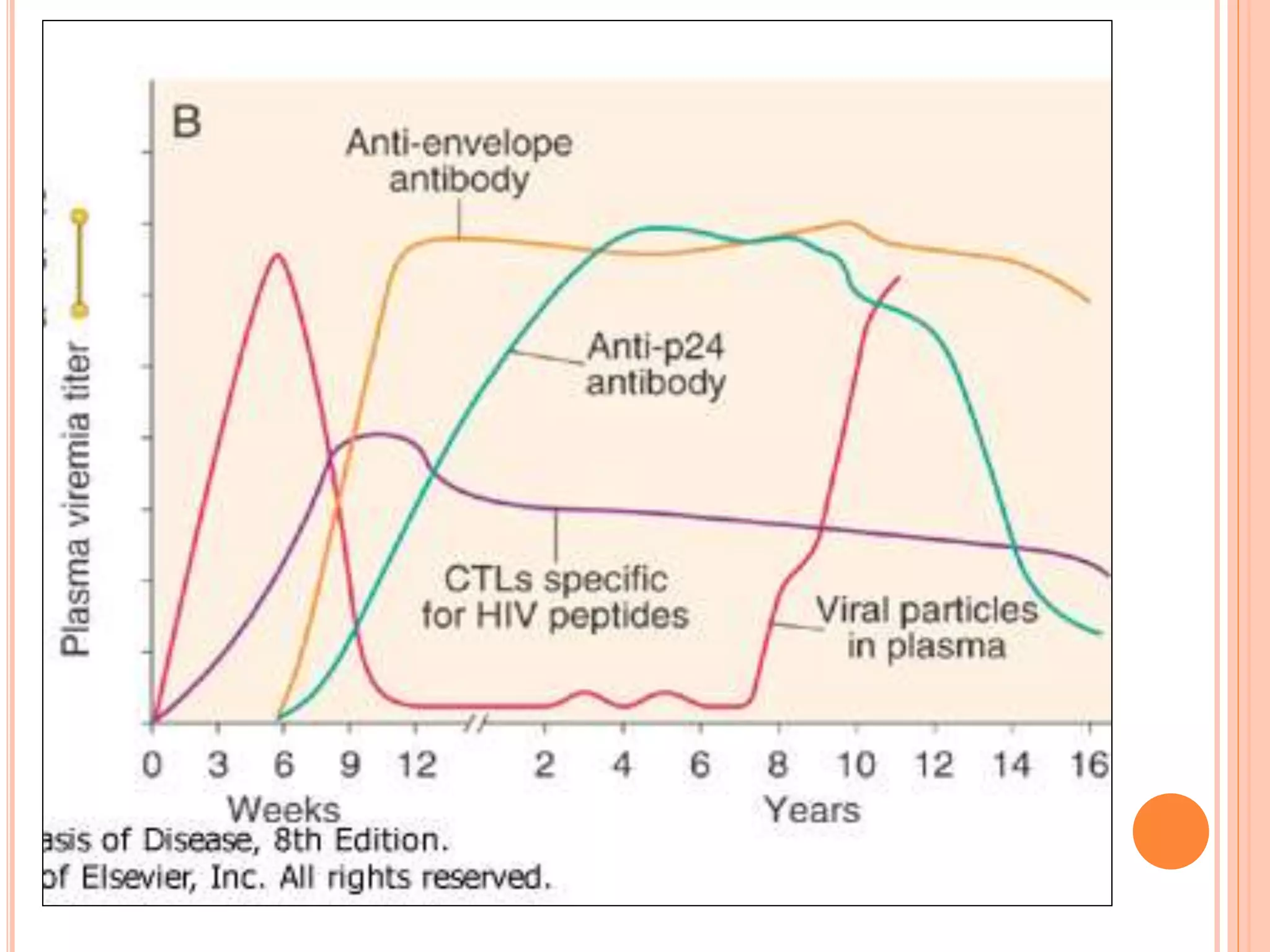
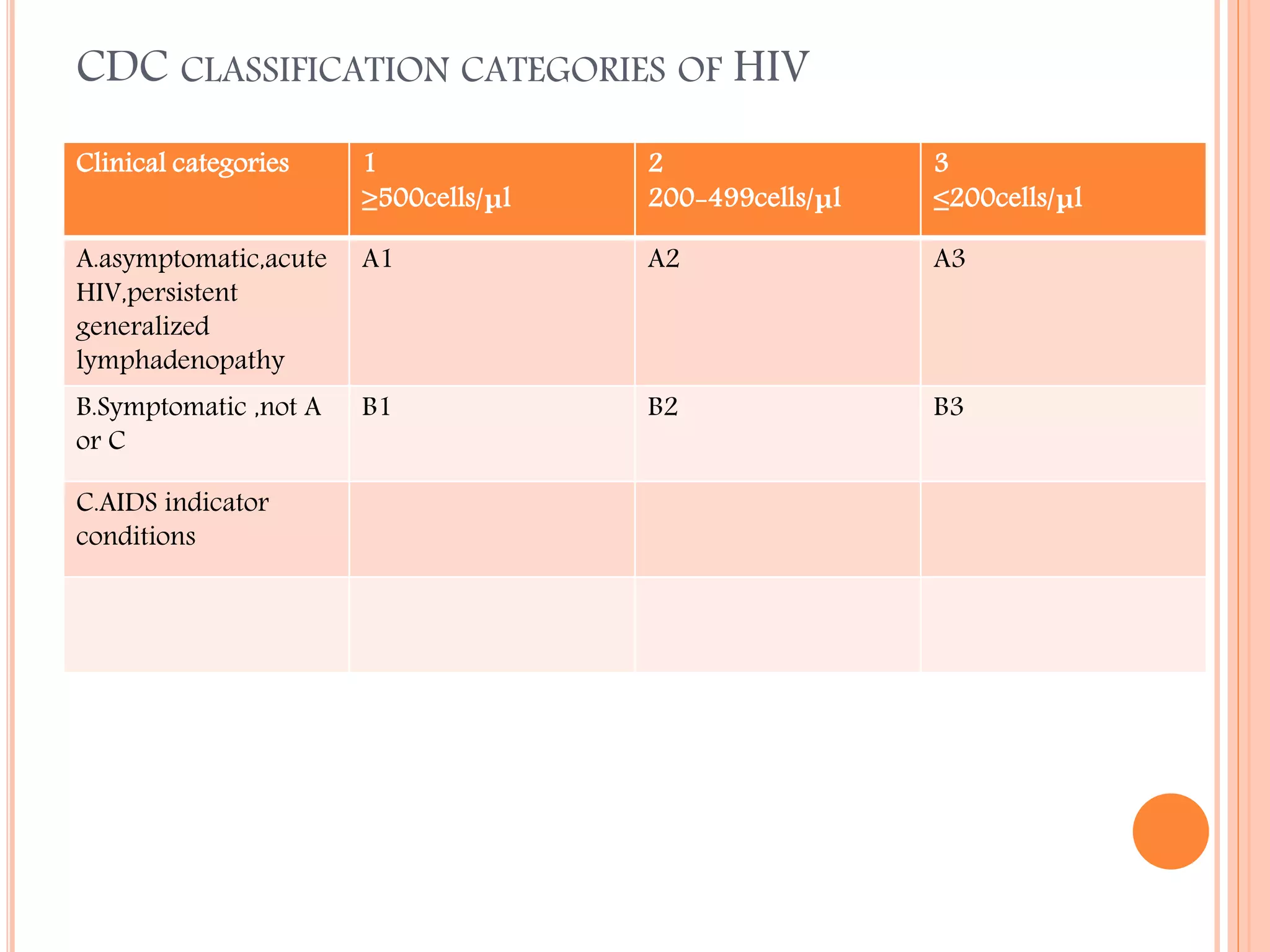
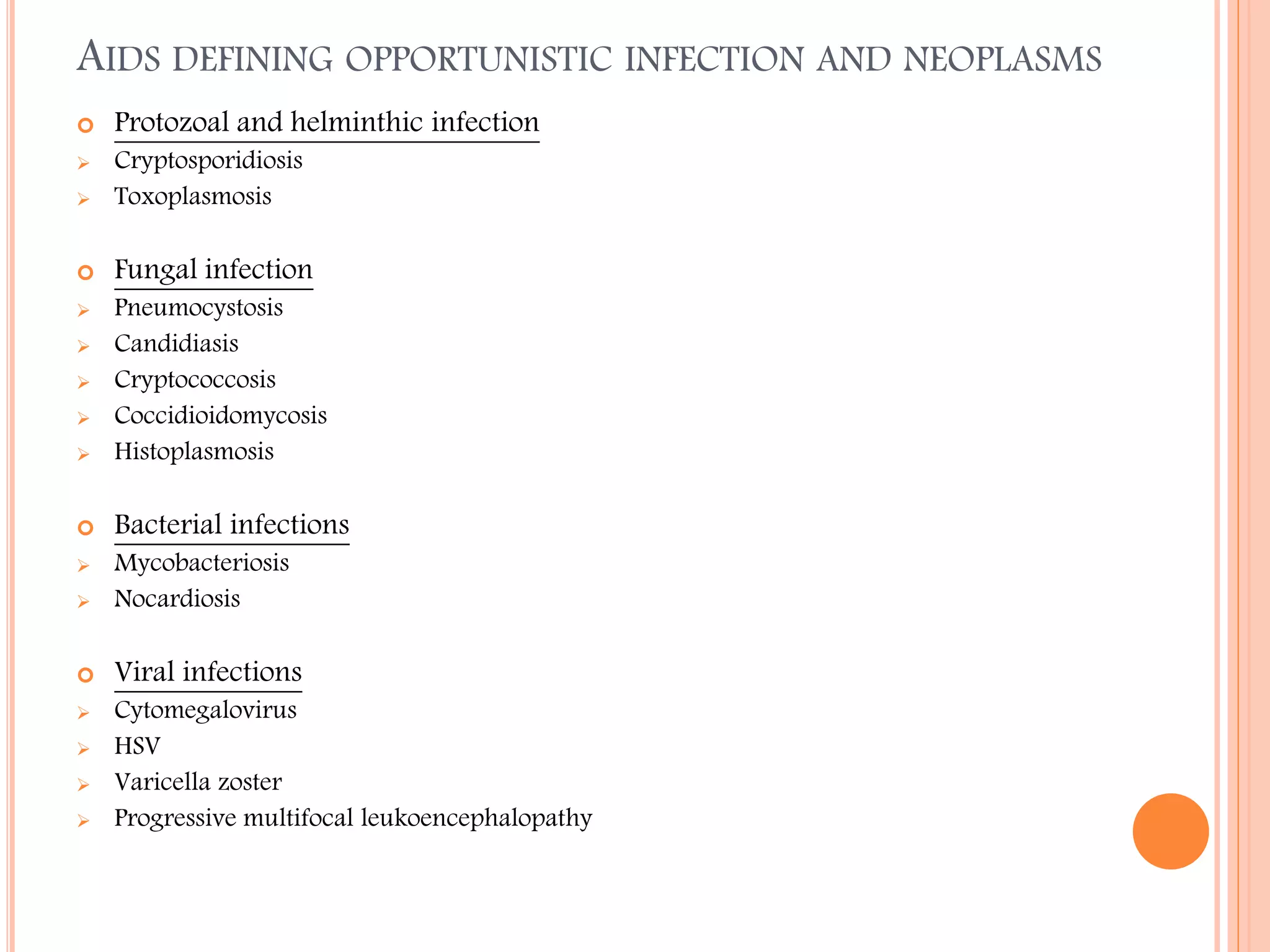
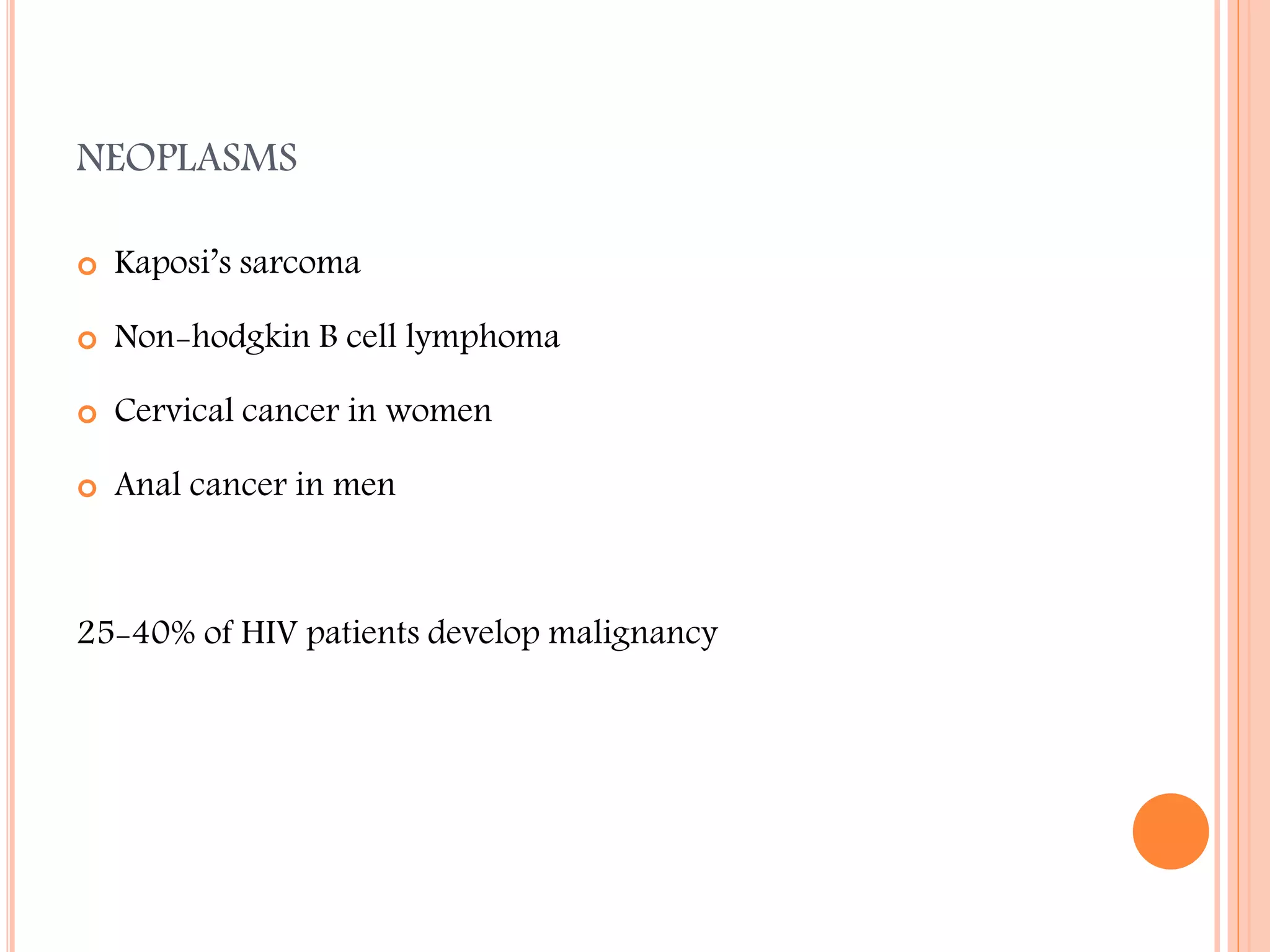
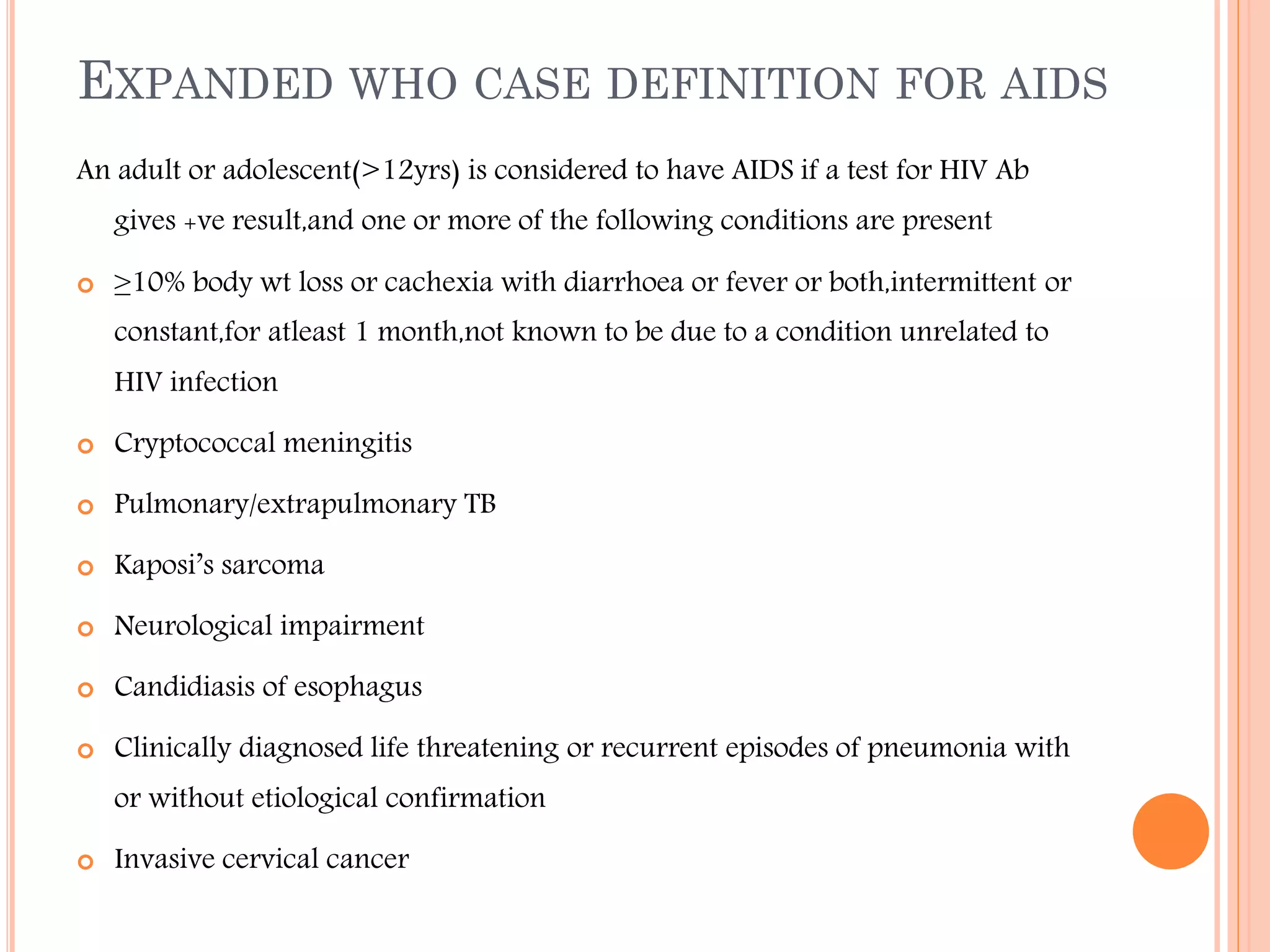
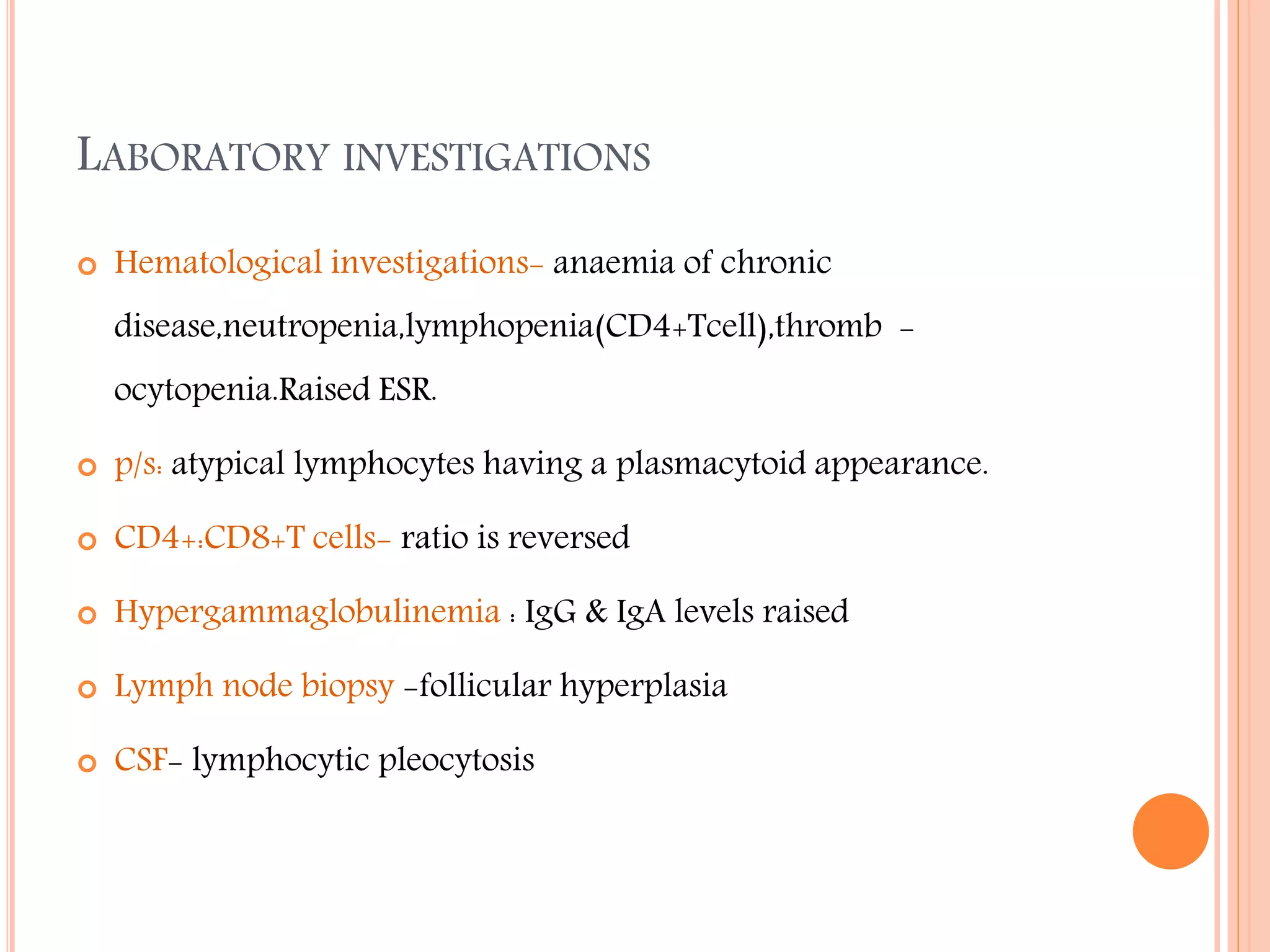
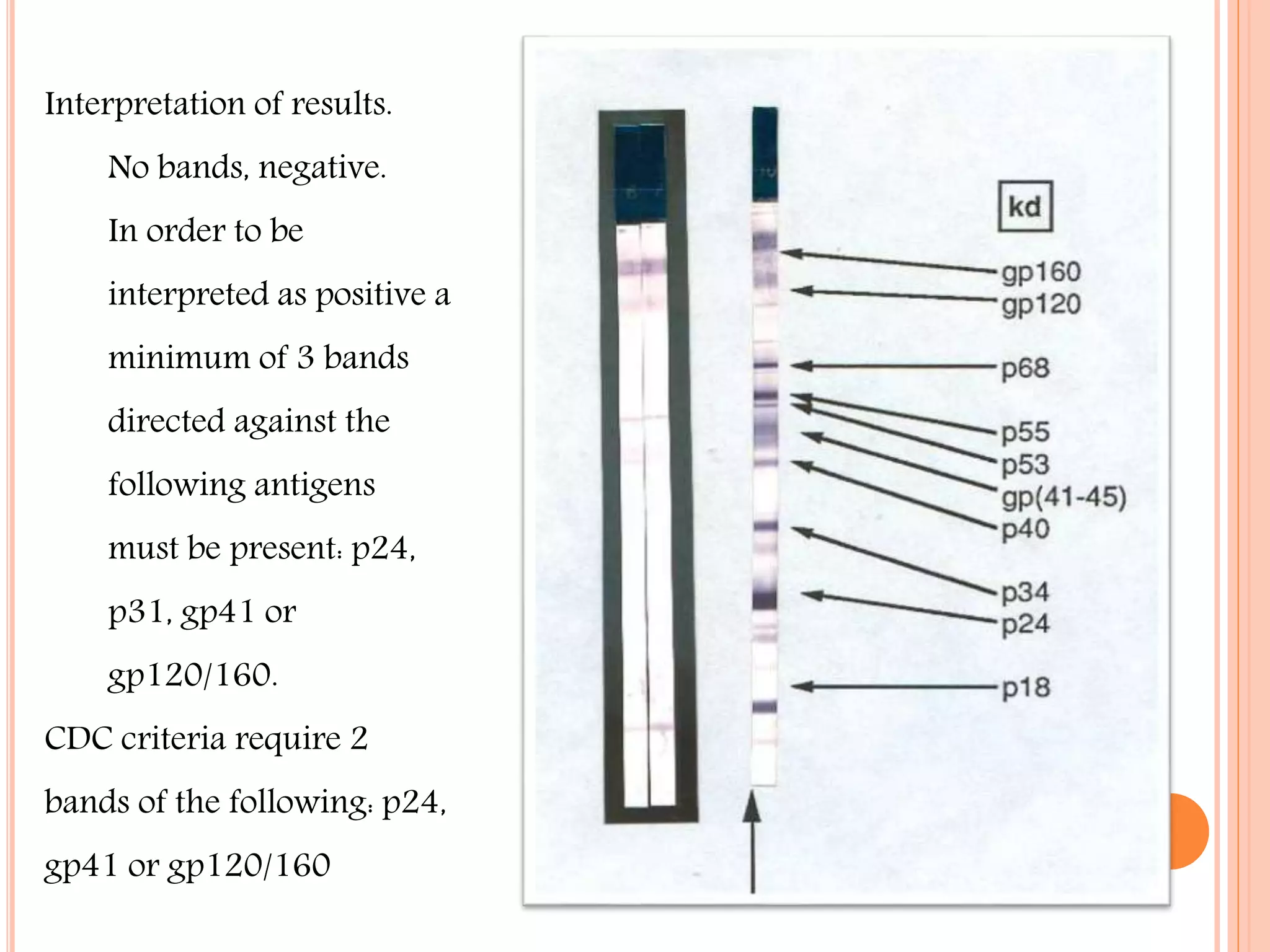
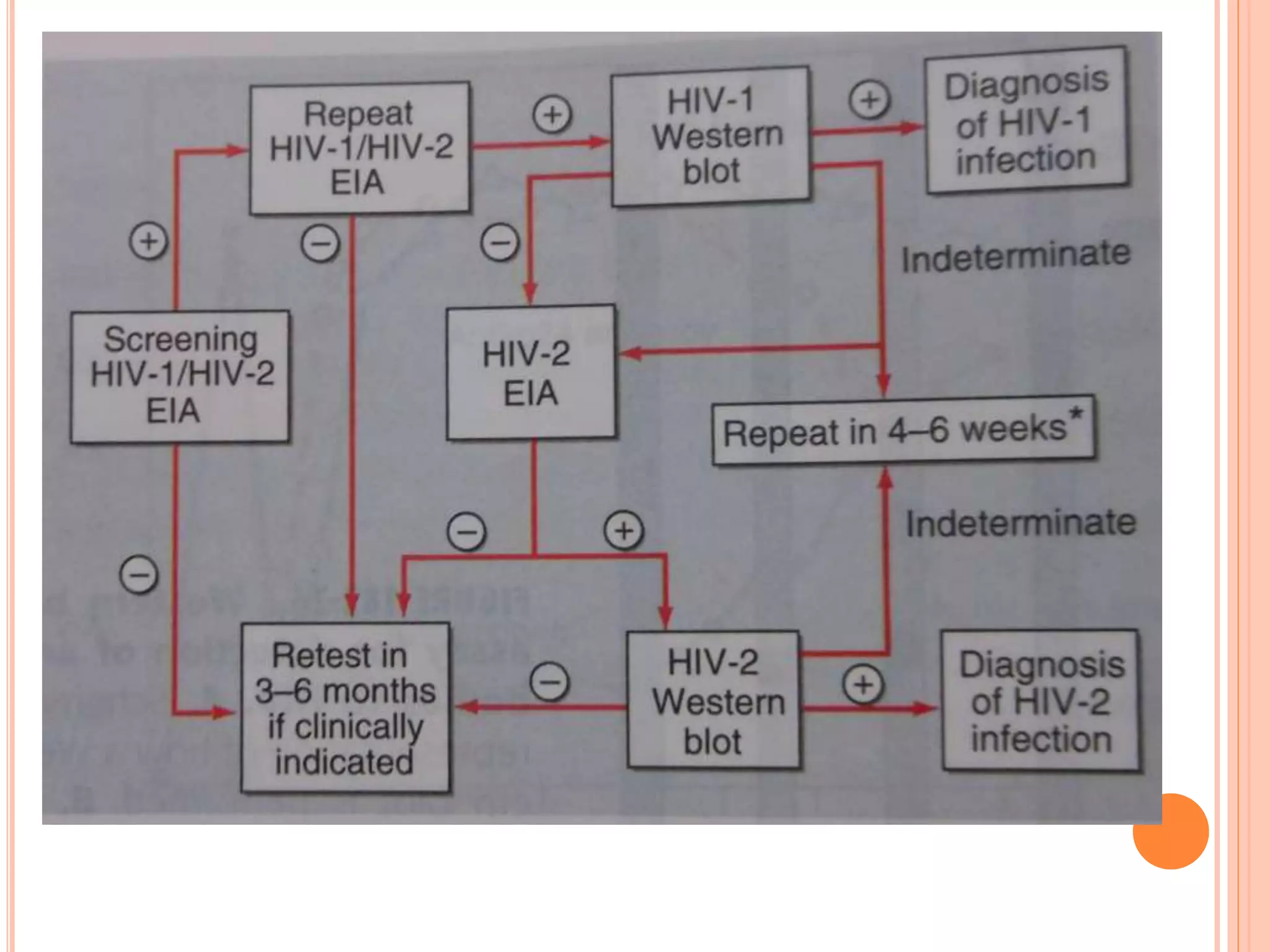
The document summarizes key information about AIDS/HIV. It describes how AIDS was first identified in 1981 from cases of rare illnesses in young adults. HIV was discovered in 1983-84 as the causative agent. AIDS has since become a global pandemic, with over 33 million people living with HIV in 2007. The virus primarily transmits through sexual contact, blood, and from mother to child. Laboratory tests are used to diagnose HIV by detecting antibodies, antigens, or viral RNA. Treatment involves antiretroviral drugs, while prevention strategies include safe sex practices, needle exchange programs, and blood screening.