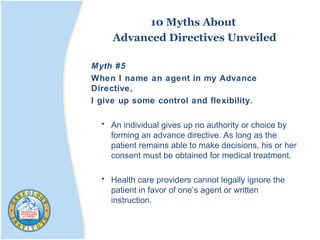
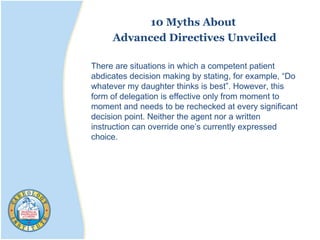
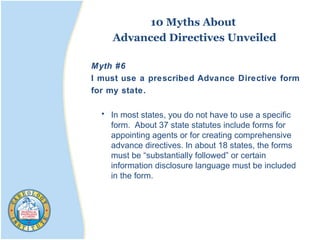
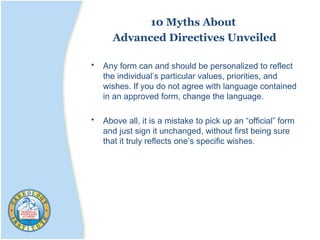
This document provides information about advanced directives. It defines an advanced directive as a legal document that specifies a person's wishes for medical treatment if they become unable to make decisions. It discusses the importance of advanced directives for patients, families, and physicians. It also describes different types of advanced directives like living wills, medical powers of attorney, and do not resuscitate orders.