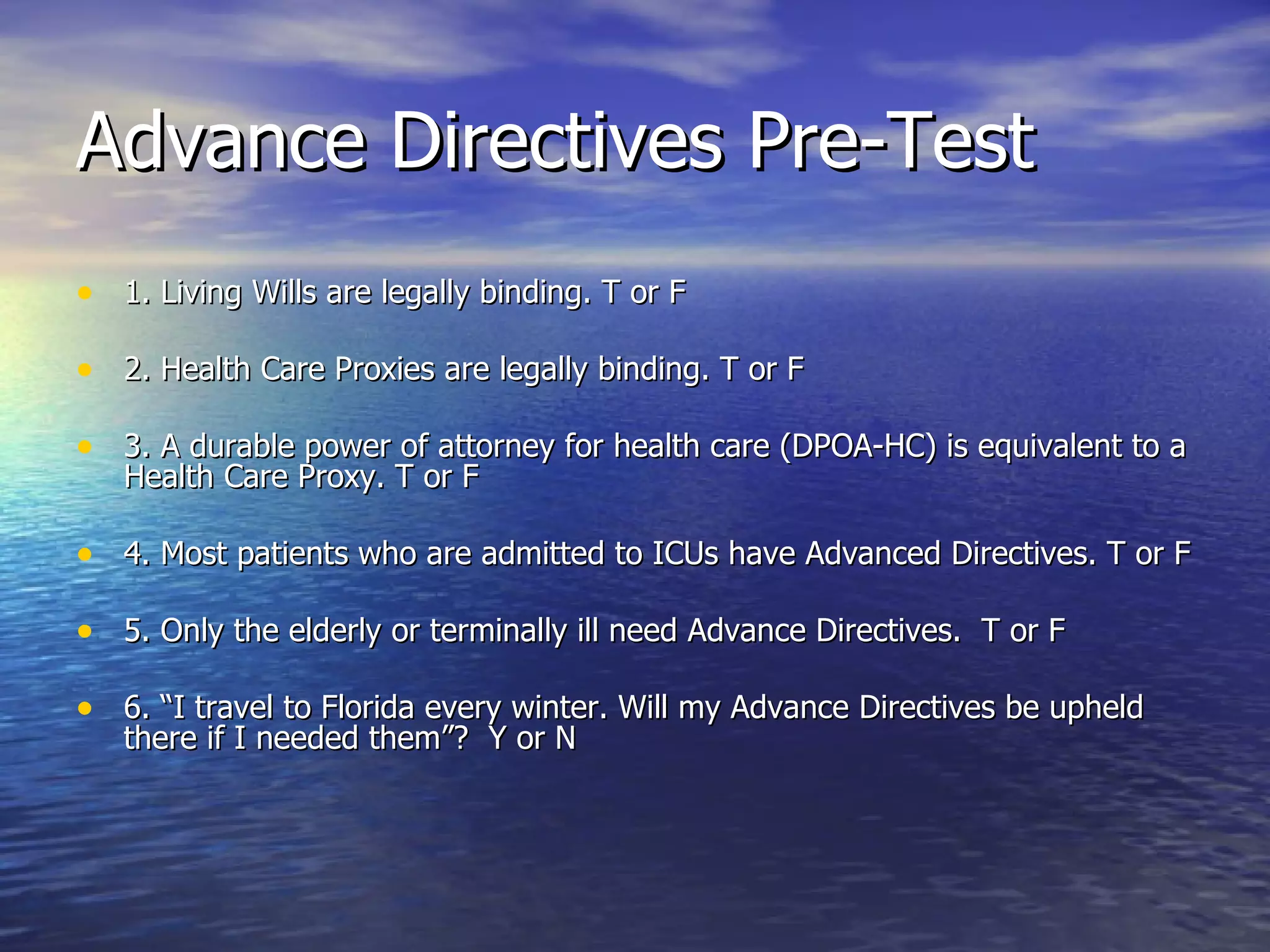
The document discusses advance directives, including living wills and health care proxies, detailing their legal implications, components, and importance for patient decision-making regarding end-of-life care. It emphasizes the need for education on creating and honoring these directives among healthcare providers and patients alike, while also addressing common barriers to their implementation. Resources and references for further information and assistance in understanding advance directives are also provided.
![An Important Point to Remember: Patient Education When discussing the CC/DNR option (and all Advance Directives) with patients it is important to discuss where these documents and bracelets should be kept. They should not be locked away. They need to be where anyone can find them. “ The answer here is not a gadget. The answer – as is the case in every EMS issue – is education… If it [the CC/DNR Verification form] is not immediately available for medical personnel, it might as well not exist.” AJ Hidell from an online discussion on www.EMTlife.com](https://image.slidesharecdn.com/advancedirectives-12796555803936-phpapp01/75/Advance-Directives-11-2048.jpg)