The document discusses advance care planning, lasting power of attorney, and advance medical directives. It provides information on:
- What advance care planning involves and its benefits in reducing crisis decision-making.
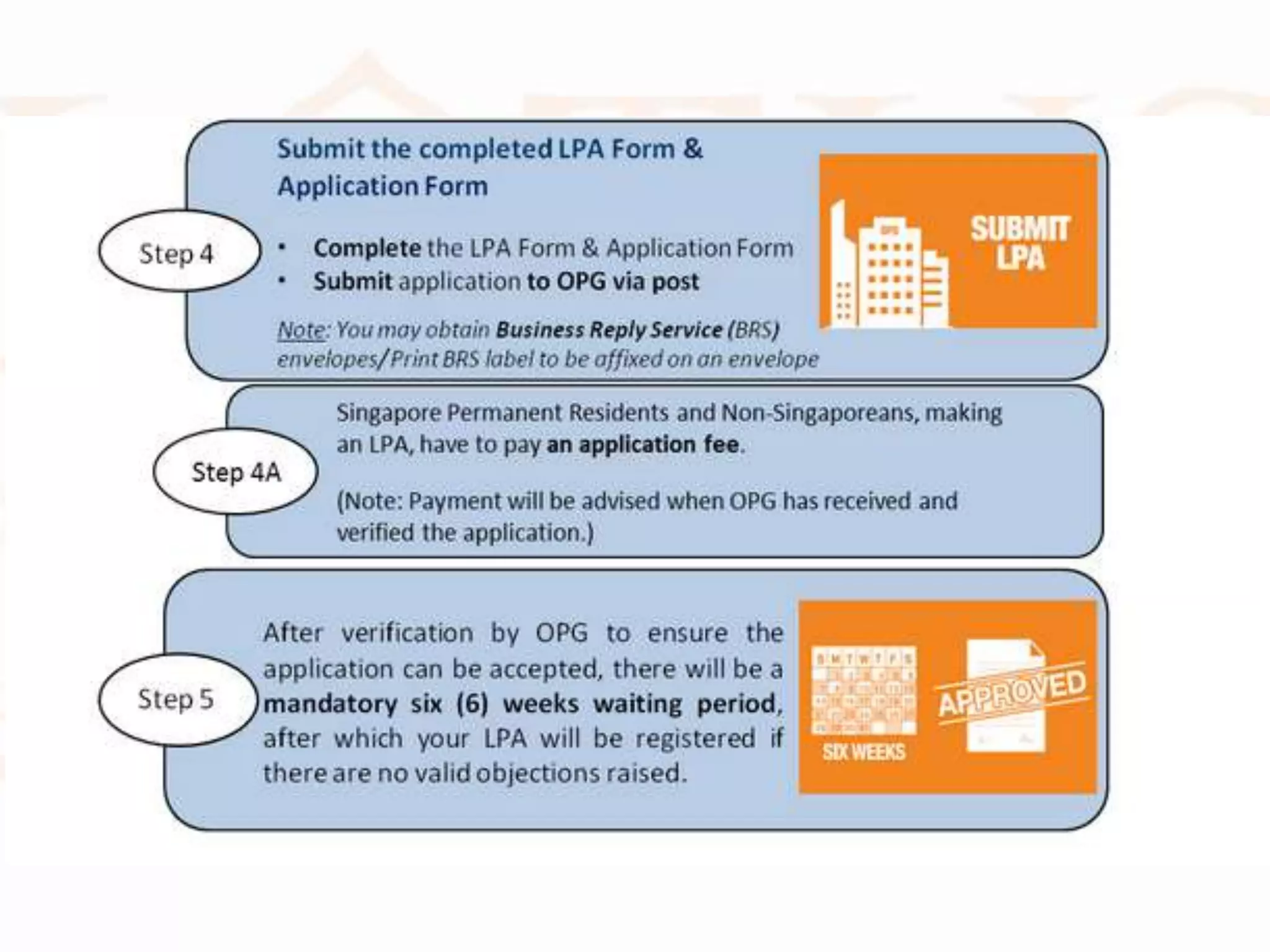
- The process of completing a lasting power of attorney, including appointing a donee to make decisions on one's behalf if mental capacity is lost.
- What an advance medical directive is and the process of completing one to inform doctors of wishes regarding life-sustaining treatment for a terminal illness.
- Challenges that can arise with implementation of these plans in real clinical situations.

















![Guidebooks
• http://www.publicguardian.gov.sg/Portals/0/Gui
des/Caregivers_Eng.pdf
• http://www.publicguardian.gov.sg/Portals/0/Gui
des/Donees%20Guide_Eng.pdf
• http://www.publicguardian.gov.sg/Portals/0/Gui
des/Guide%20to%20LPA_Eng.pdf
• http://www.publicguardian.gov.sg/Portals/0/Gui
des/Deputys%20Guide-Eng.pdf
• http://www.publicguardian.gov.sg/Portals/0/Gui
des/[EN]%20COP_3%20Apr%202014.pdf](https://image.slidesharecdn.com/2014lpaamdtalk2014-171111090206/75/2014-LPA-AMD-ACP-Talk-21-2048.jpg)