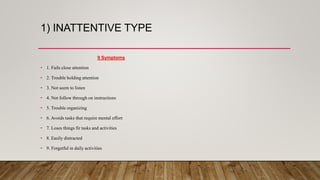
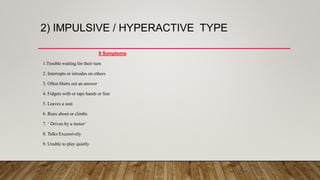
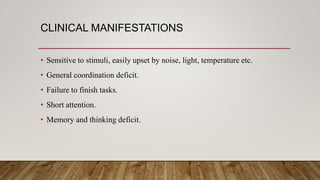
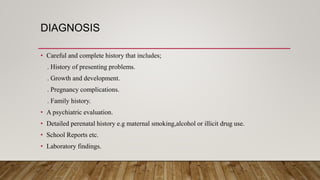
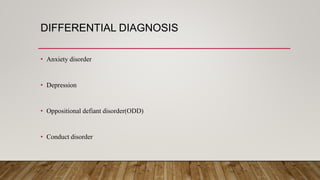
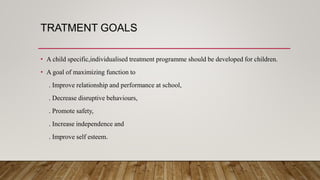
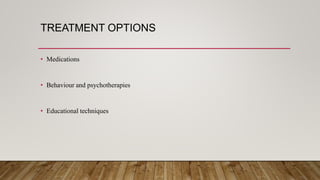
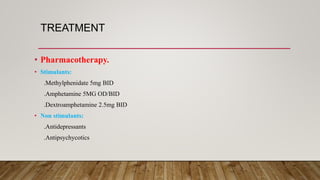
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, hyperactivity, and impulsivity. It affects approximately 9% of primary school children globally, though prevalence varies by country. Boys are four times more likely to be diagnosed than girls. ADHD has been linked to genetic and environmental factors and often co-occurs with other disorders. Treatment involves medication, behavioral therapies, educational support, and nursing interventions to create a structured environment and reinforce positive behaviors. Careful diagnosis and ongoing follow-up care are important to properly manage the condition.