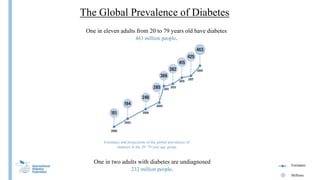
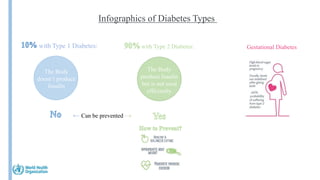
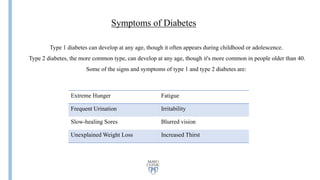
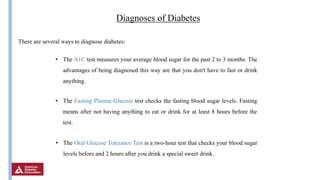
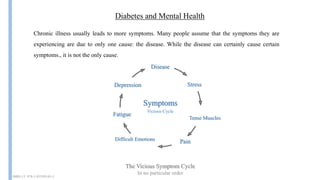
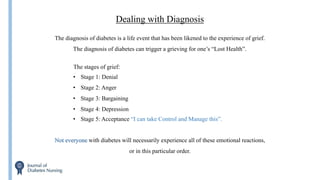
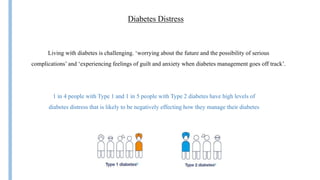
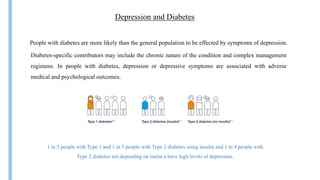
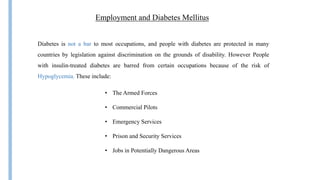
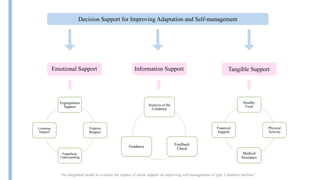
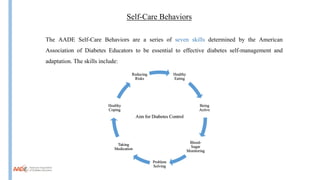
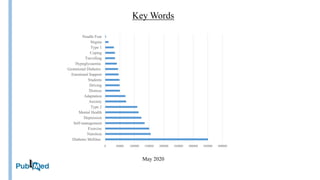
The document discusses diabetes mellitus, covering its physiological aspects, types, historical context, global prevalence, causes, symptoms, diagnoses, psychological impacts, and social considerations. It highlights the relationship between diabetes management and mental health, detailing emotional challenges faced by individuals with diabetes, such as diabetes distress and depression. Additionally, it emphasizes the importance of social support and effective self-care practices in managing diabetes.