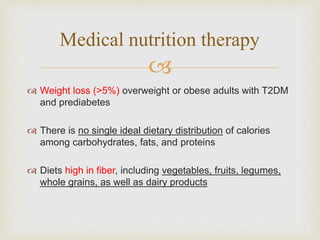
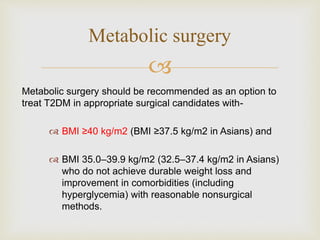
This document provides classifications, diagnostic criteria, screening recommendations, treatment targets, and management strategies for different types of diabetes and related complications. It discusses classifications of diabetes, criteria for diagnosing and staging pre-diabetes and diabetes, recommendations for vaccinations and medical evaluations. It also outlines lifestyle management approaches, guidelines for glycemic, blood pressure, and lipid control, and considerations for treating diabetes-related complications including diabetic kidney disease and retinopathy.




















![
Glucose (15–20 g) is the preferred treatment for the
conscious individual with blood glucose <70 mg/dL [3.9
mmol/L]
15 minutes after treatment, if SMBG shows continued
hypoglycemia, the treatment should be repeated.
Treatment](https://image.slidesharecdn.com/adaguidelines2019dr-190312112310/85/ADA-guidelines-2019_Dr-Tarik-22-320.jpg)