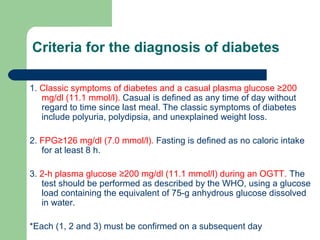
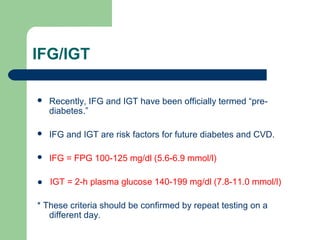
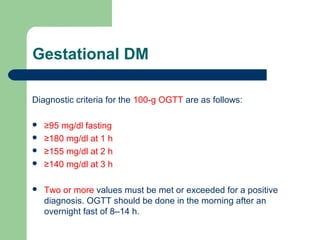
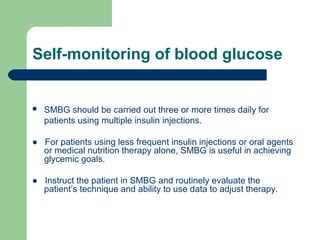
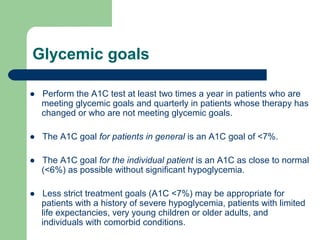
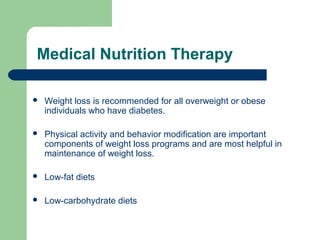
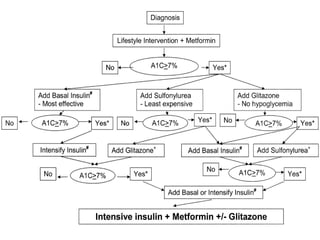
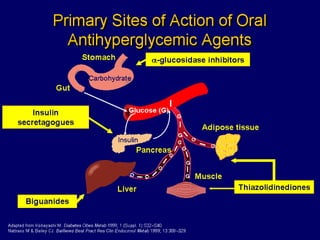
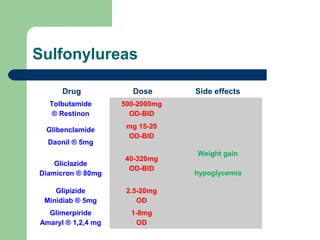
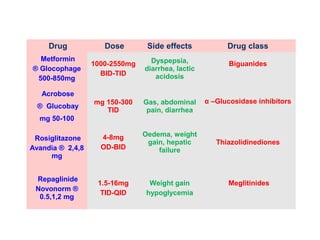
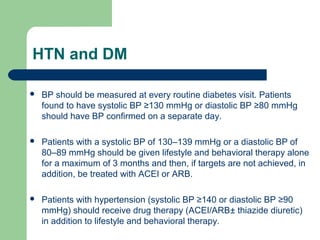
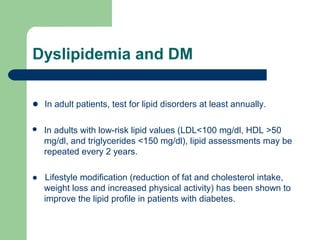
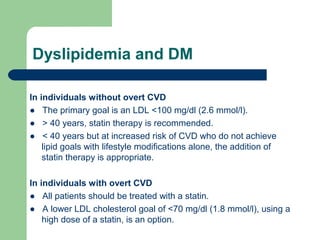
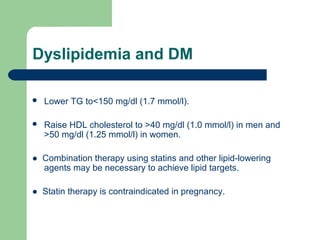
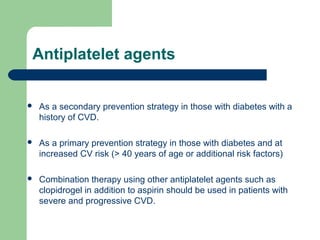
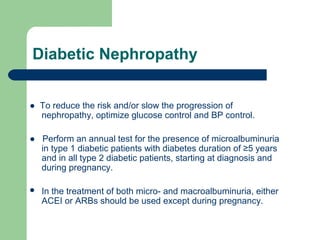
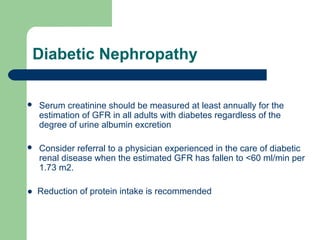
Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia. DM prevalence in Saudi Arabia is high at 23.7%. DM is diagnosed based on classic symptoms and elevated blood glucose levels. Prediabetes conditions like impaired fasting glucose and impaired glucose tolerance are risk factors for future diabetes and cardiovascular disease. Glycemic goals aim for an A1C below 7% and treatment involves medical nutrition therapy, oral medications, insulin, and preventing complications. Management of DM focuses on controlling blood glucose, blood pressure, lipids, and screening for and treating common complications.