Tonsillopharyngitis, commonly referred to as strep throat, is an acute infection affecting the pharynx and tonsils, primarily caused by viral agents but also including bacterial infections like group A strep. Diagnosis involves clinical evaluation and specific tests such as throat swabs, and treatment includes symptomatic relief and antibiotics when necessary, particularly for bacterial causes. Patient education on hygiene and management of symptoms is crucial for minimizing transmission and improving recovery.

![Etiology
• Viral
• Main cause of acute tonsillopharyngitis
• Double-stranded DNA viruses (human adenovirus,
Epstein-Barr virus), single-stranded RNA viruses
(influenza, para-influenza, rhinovirus, enteroviruses,
Coxsackie virus, coronaviruses, respiratory syncytial virus
[RSV], human meta-pneumo-virus), and retroviruses
(human immunodeficiency virus [HIV]) are among the
viral causes
• Bacterial
• Responsible for about 5-15% of clinic consultations for
acute sore throat in adults
• Most commonly caused by Gram-positive cocci known
as S pyogenes
• This organism exhibits beta-hemolysis on blood
agar plates
• Belongs to group A Lancefield classification system
for beta-hemolytic strep infection
• Other bacterial causes include group C and
G Streptococci, Hemophilus
influenzae, Nocardia, Corynebacteria and Neisseria
gonorrhoeae](https://image.slidesharecdn.com/diagnosticmethodsfortonsillopharyngitis-acute-241221110208-2bc47b6e/85/DIAGNOSTIC-METHODS-FOR-TONSILLOPHARYNGITIS-ACUTE-pptx-3-320.jpg)


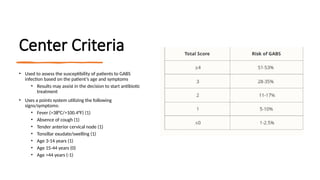
![Conditions Where Lab Tests for GABS are Not
Available or Not Practical
Antibiotics will not be needed for every patient that presents with sore throat
Antibiotics should not be withheld if the clinical condition is severe or GABS is suspected
Modified Centor score or FeverPAIN can be used to decide
on which patients need no testing, lab tests (throat swab or
rapid antigen detection test [RADT]) or empiric antibiotic
therapy
Score of 0 to 1 does not require testing or antibiotic therapy
Patients with score of 2 or 3 require testing, positive results warrant
empiric therapy
Score of ≥4 is at high risk of GABS and empiric therapy is considered](https://image.slidesharecdn.com/diagnosticmethodsfortonsillopharyngitis-acute-241221110208-2bc47b6e/85/DIAGNOSTIC-METHODS-FOR-TONSILLOPHARYNGITIS-ACUTE-pptx-9-320.jpg)