This document provides an overview of pancreatitis, including:
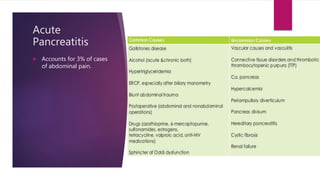
- It describes acute and chronic pancreatitis, with acute pancreatitis presenting with abdominal pain and elevated enzymes.
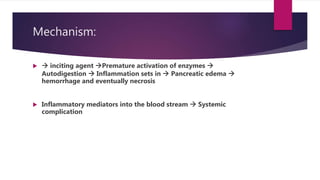
- The mechanism involves premature enzyme activation leading to autodigestion and inflammation of the pancreas.
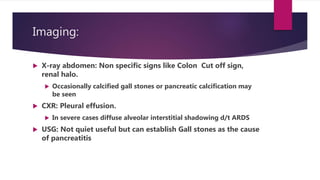
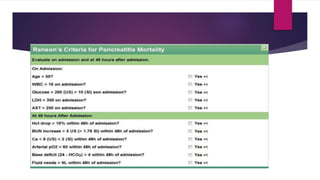
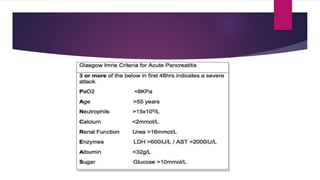
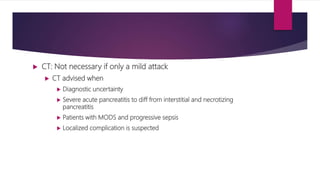
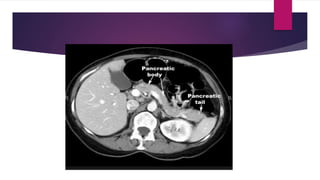
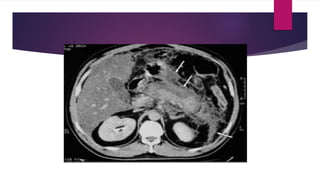
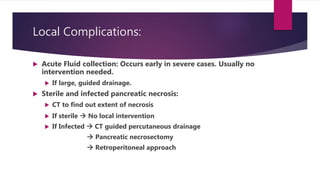
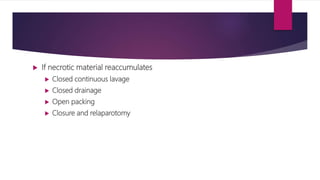
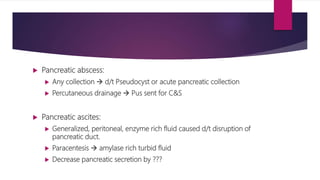
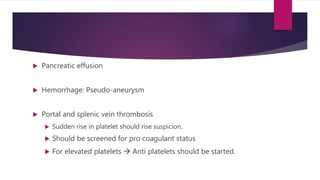
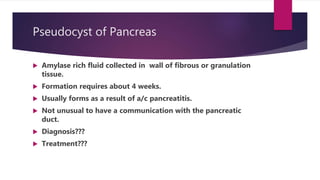
- Signs, symptoms, and imaging findings are discussed for assessing severity and managing acute pancreatitis. Complications like fluid collections, necrosis, and abscesses are also covered.
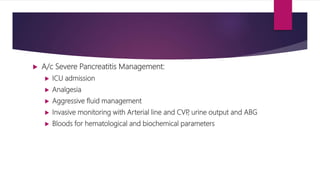
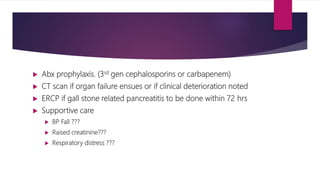
- Treatment involves conservative management for mild cases and intensive care, monitoring, antibiotics and drainage procedures for more severe cases.