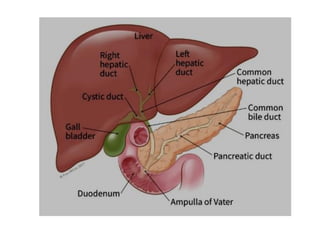
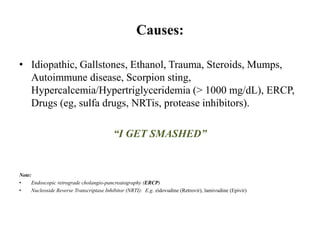
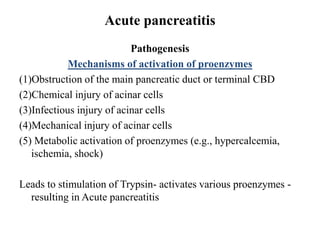
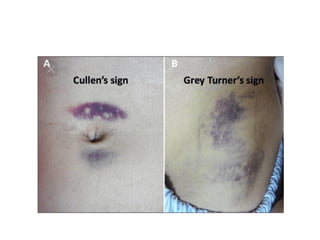
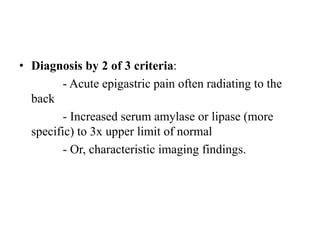
Acute pancreatitis is an inflammatory disorder of the pancreas that can range from mild to severe with widespread tissue death. The major causes are alcohol abuse and gallstones. The pathogenesis involves premature activation of pancreatic enzymes within the pancreas due to obstruction of the pancreatic duct, chemical or infectious injury to pancreatic cells, or metabolic abnormalities. This leads to autodigestion of the pancreas and systemic complications affecting other organs. Symptoms include severe abdominal pain, nausea and vomiting, and systemic complications can include respiratory failure and organ dysfunction. The diagnosis is based on acute abdominal pain combined with high pancreatic enzymes or imaging findings.