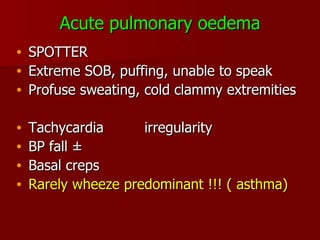
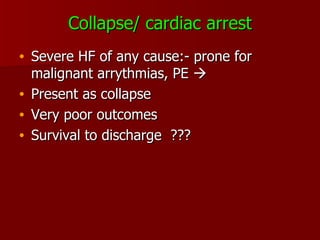
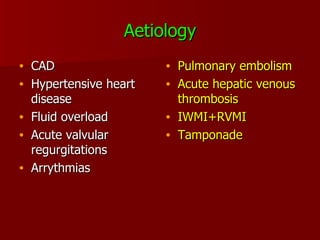
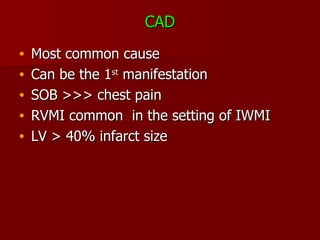
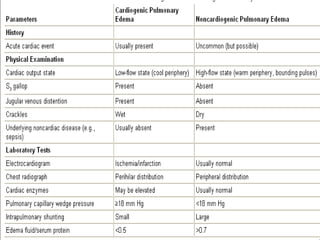
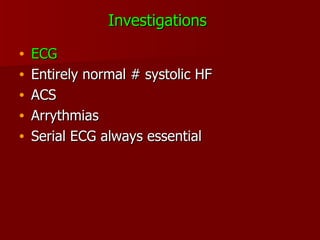
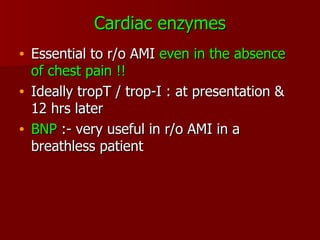
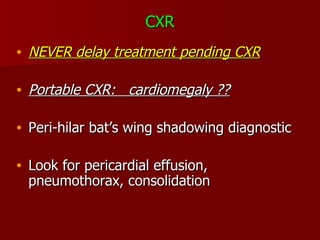
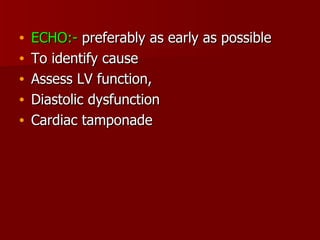
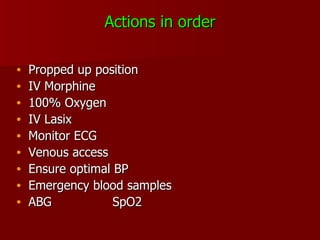
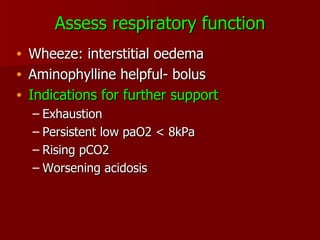
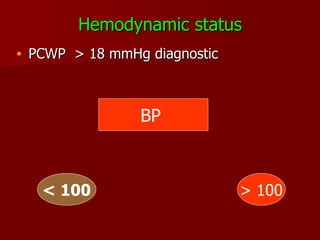
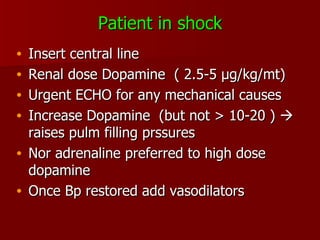
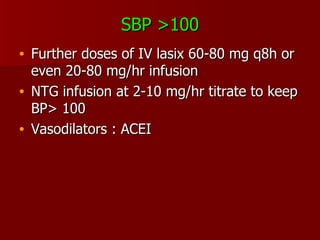
Acute heart failure is a common emergency presentation with high mortality and morbidity. While clinical examination findings are not always sensitive or specific, prompt recognition and stabilization of the patient is a priority. Presentations can include shortness of breath, frothy sputum, collapse, or cardiac arrest. Investigations including ECG, cardiac enzymes, BNP, CXR, and echocardiogram help determine the cause and assess cardiac function. Initial stabilization involves propping the patient up, administering oxygen, diuretics, and monitoring vital signs to optimize hemodynamic status before further treatment.