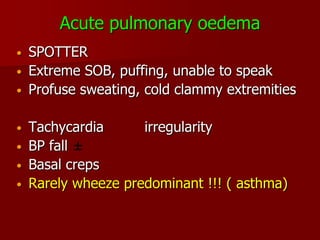
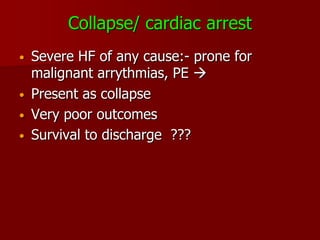
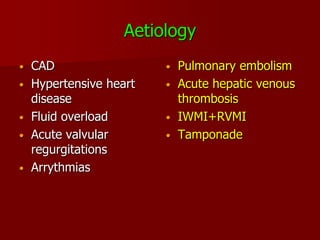
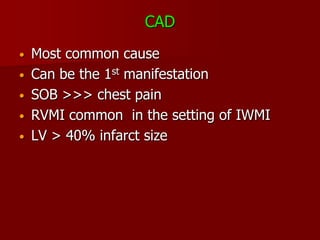
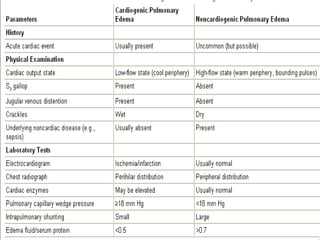
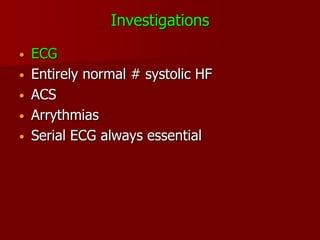
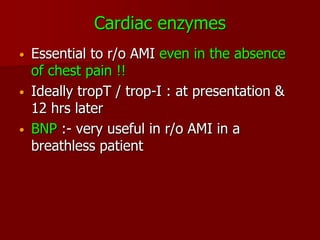
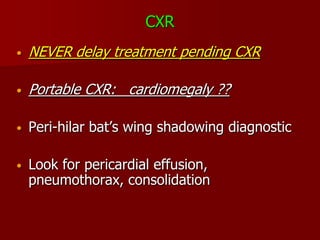
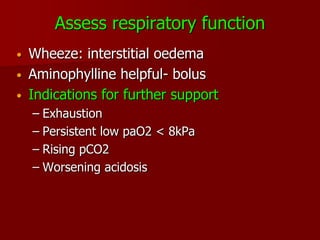
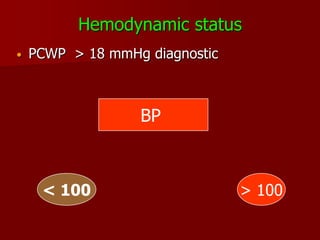
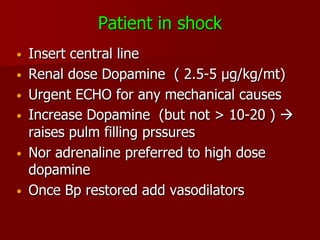
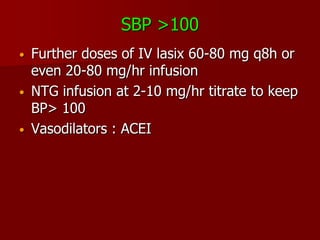
This document discusses acute heart failure, including its high mortality and morbidity. Key presentations include acute shortness of breath, frothy sputum, collapse, shock, and cardiac arrest. Investigations include ECG, cardiac enzymes, chest x-ray, and echocardiogram. Treatment priorities are propped up positioning, IV morphine, 100% oxygen, IV lasix, hemodynamic monitoring, and ensuring optimal blood pressure. Further management depends on respiratory and hemodynamic status, and may include additional diuretics, nitrates, inotropes, or vasodilators.