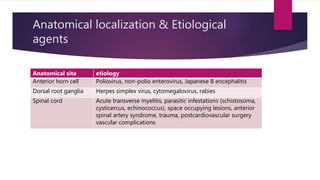
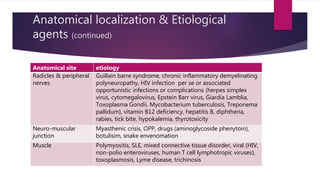
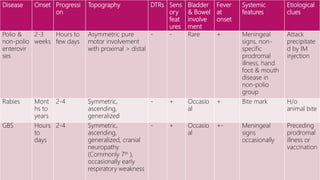
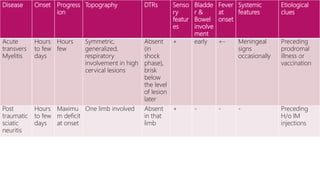
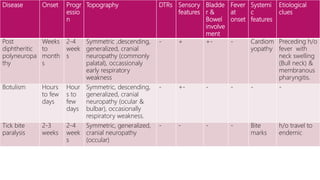
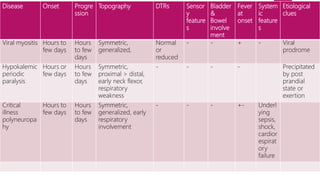
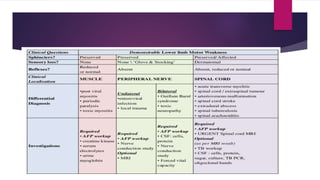
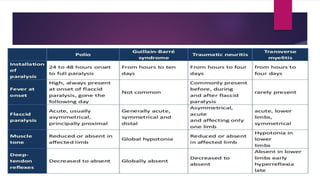
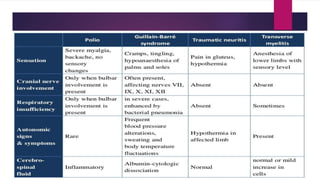
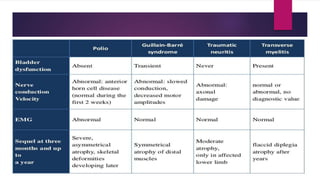
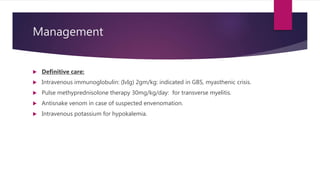
This document provides information about acute flaccid paralysis (AFP), including its definition, anatomical localization, etiological agents, clinical features, investigations, treatment, and AFP surveillance. AFP is a lower motor neuron lesion characterized by sudden onset of weakness or paralysis in a previously normal limb in a patient under 15 years old. It can be caused by viruses, bacteria, toxins affecting different areas of the motor neuron. Clinical features vary depending on the cause but may include asymmetric weakness, sensory changes, bladder involvement and fever. Treatment involves supportive care and addressing the underlying cause. AFP surveillance is important for detecting polio cases and importation through reporting, specimen collection, identification and mapping of viruses.