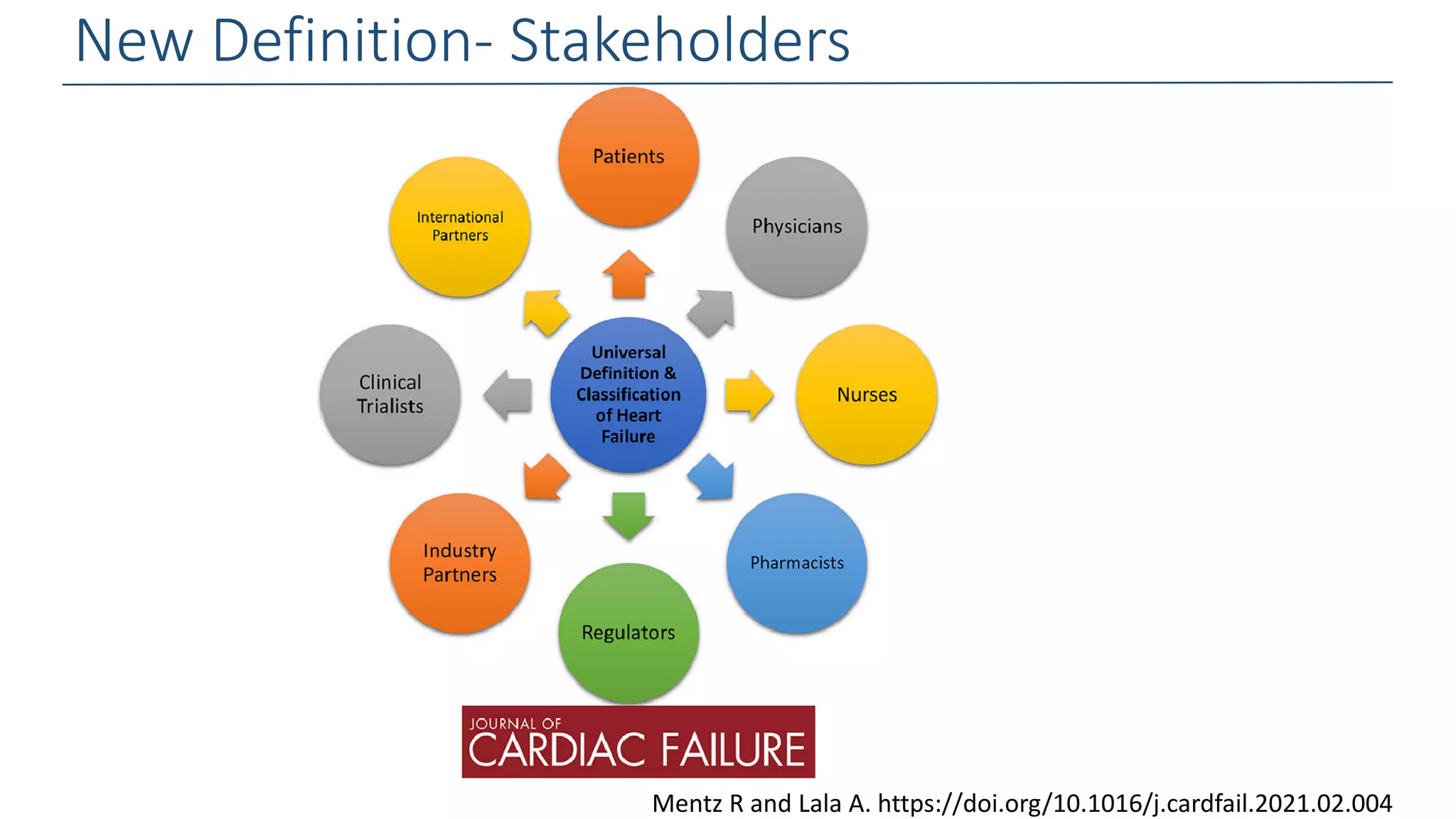
1. The document presents an overview of Biykem Bozkurt, an expert in heart failure, and their work updating the definition and classification of heart failure.
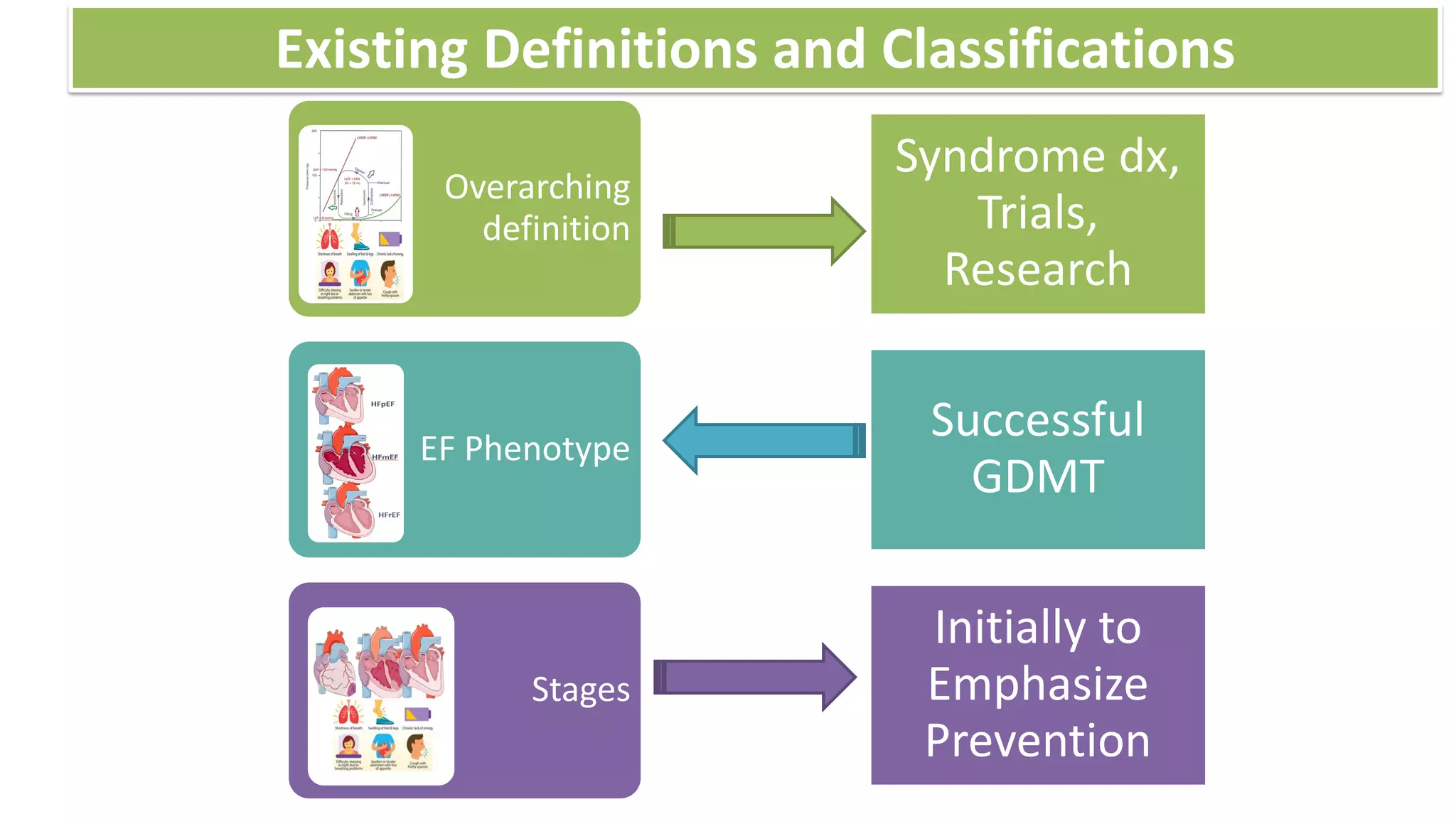
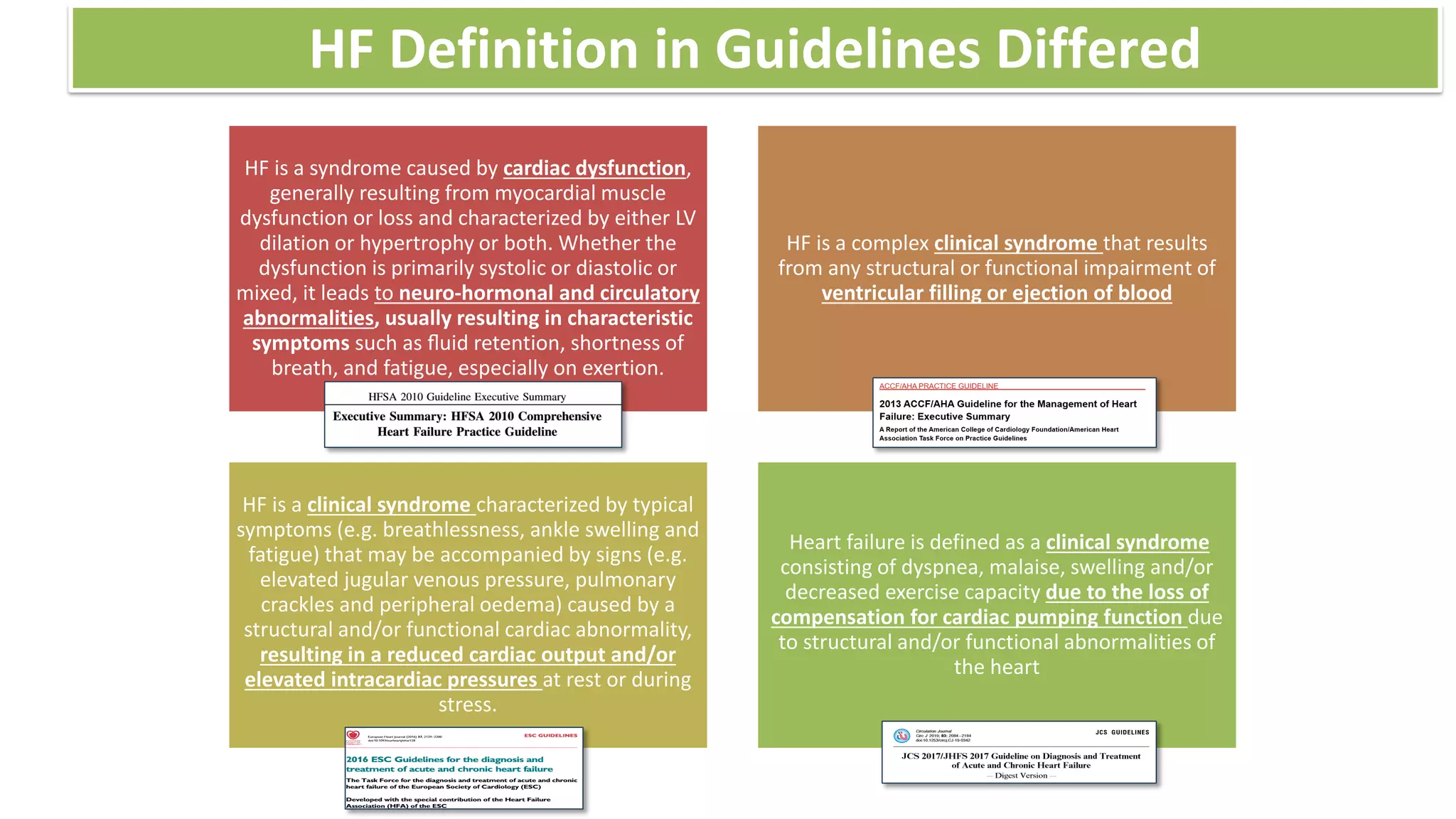
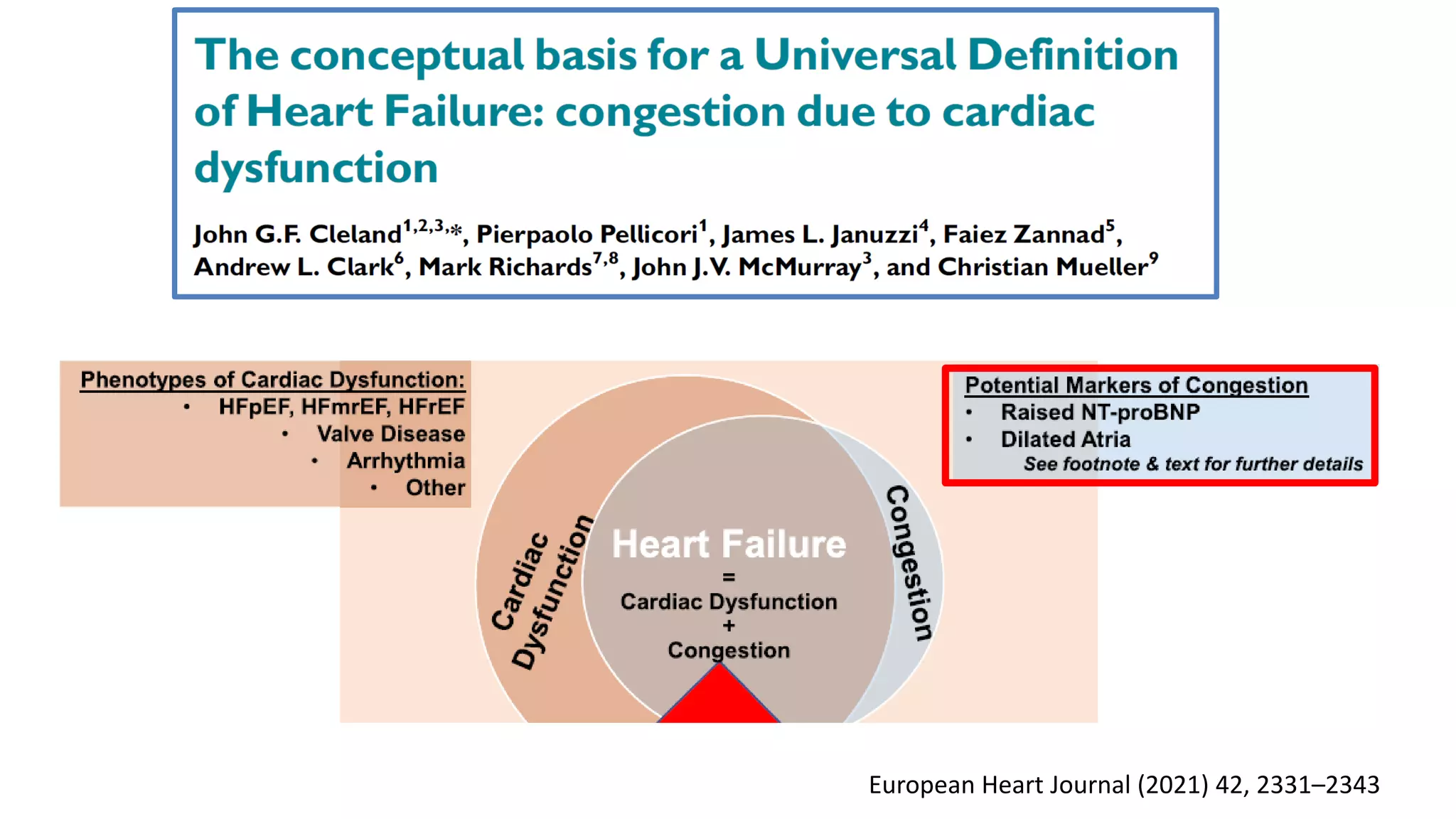
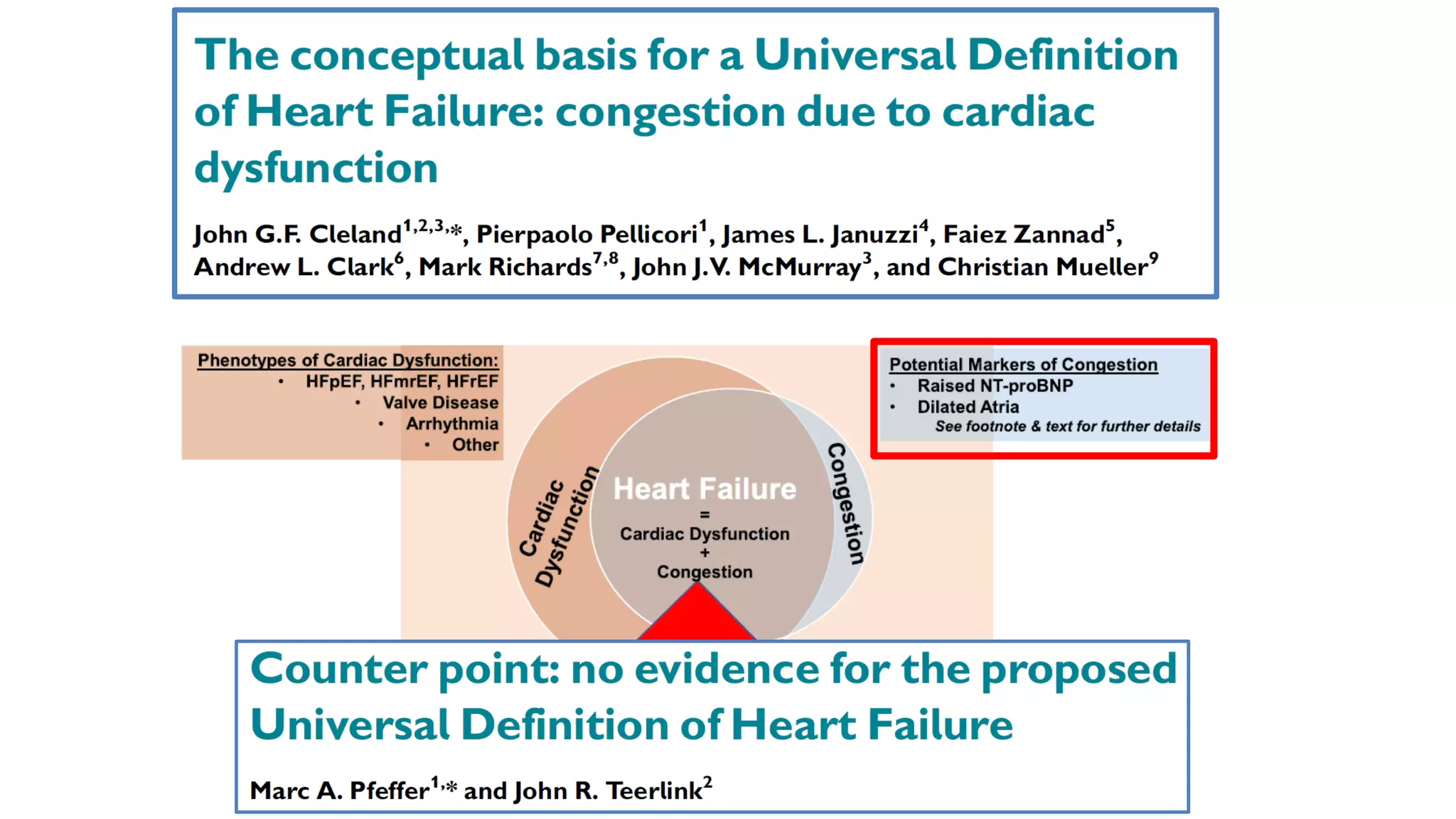
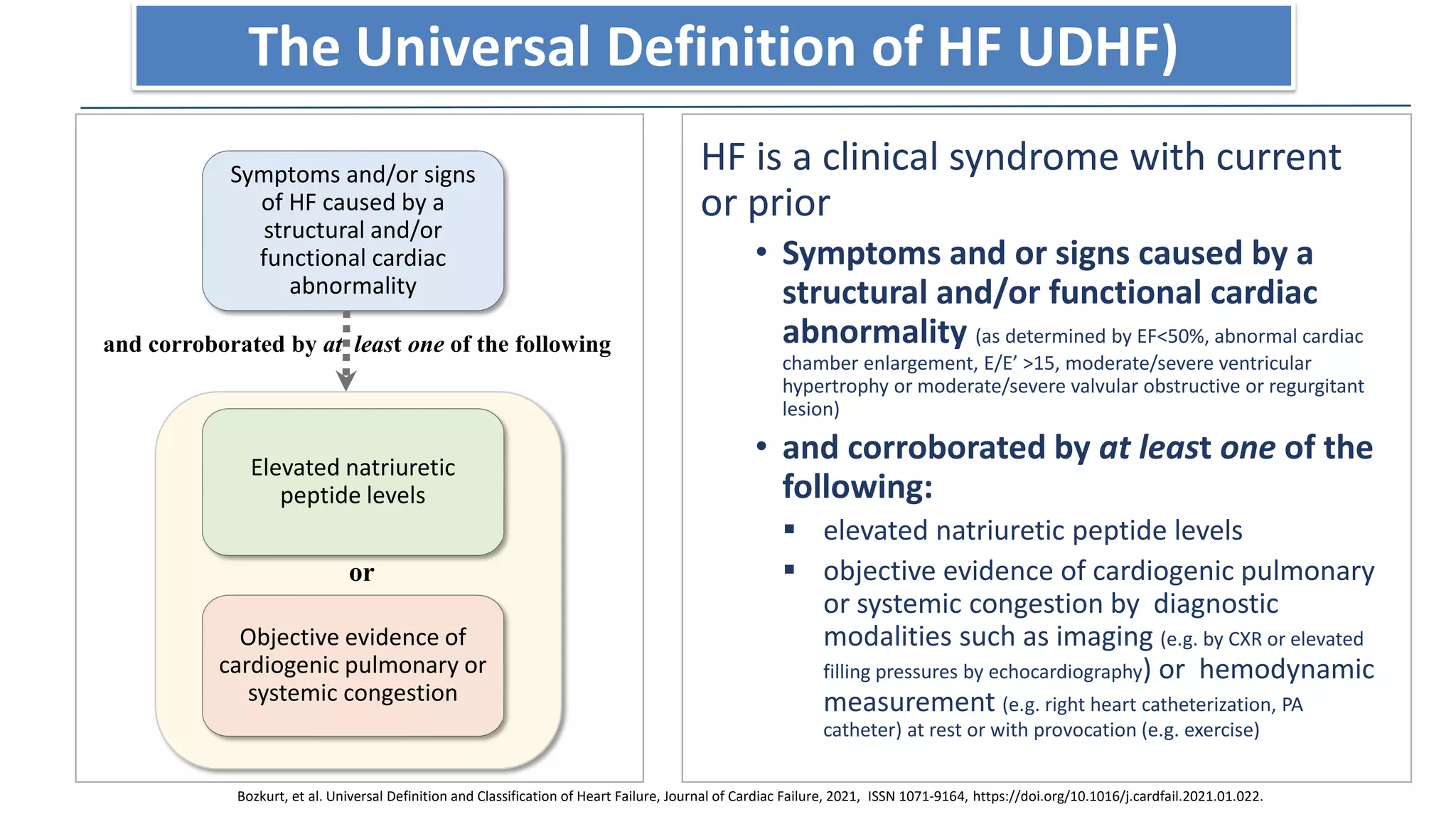
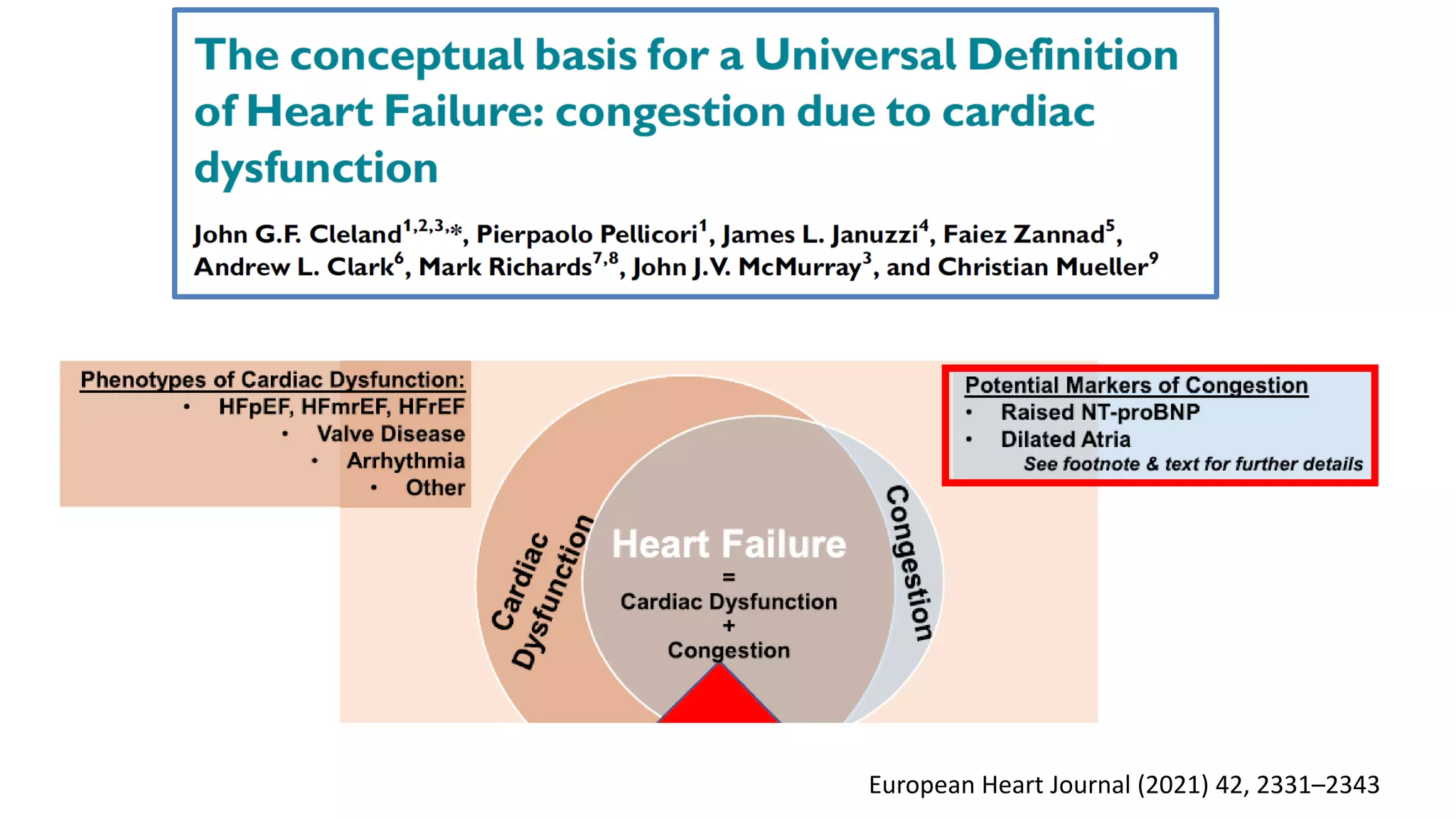
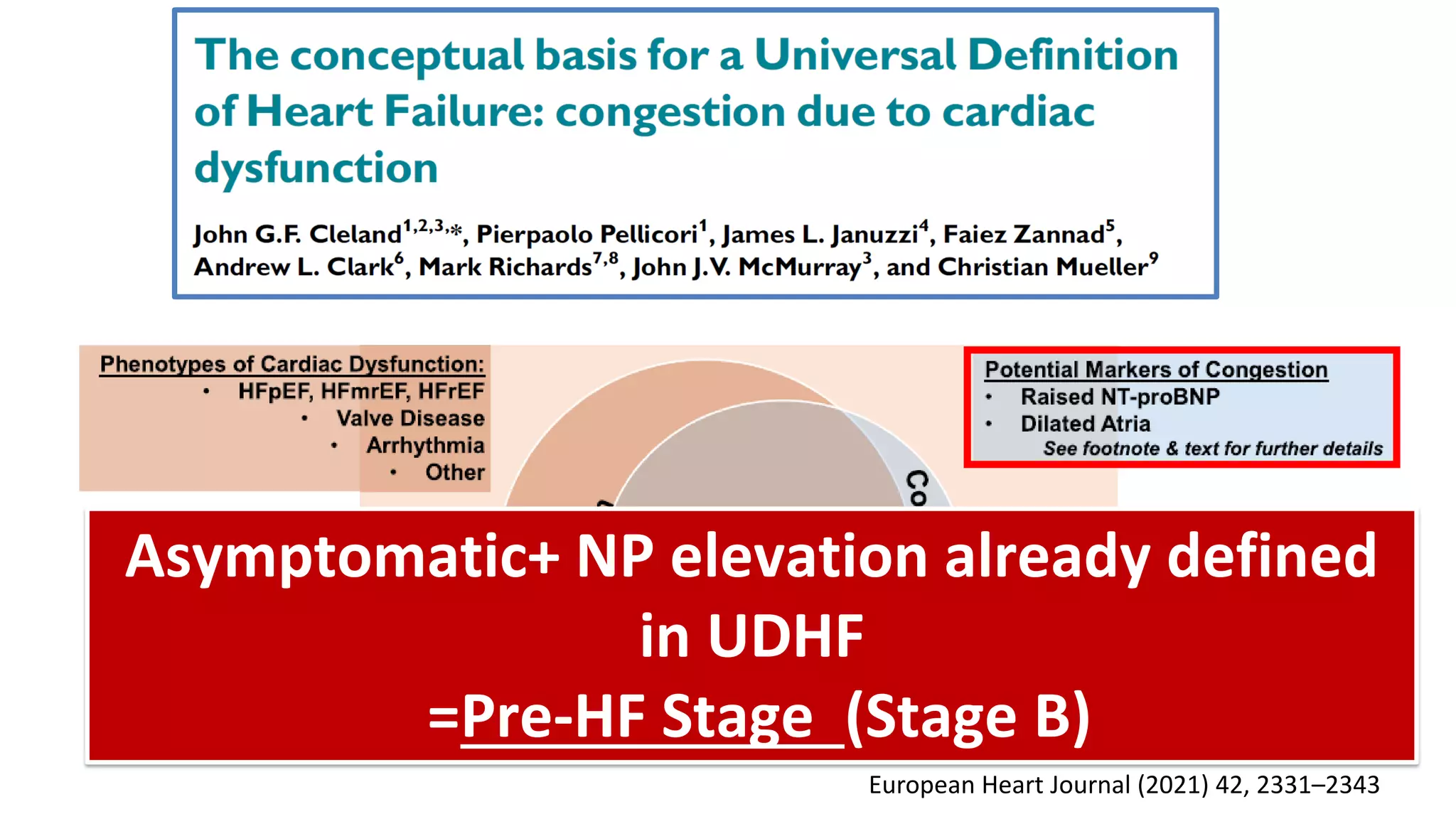
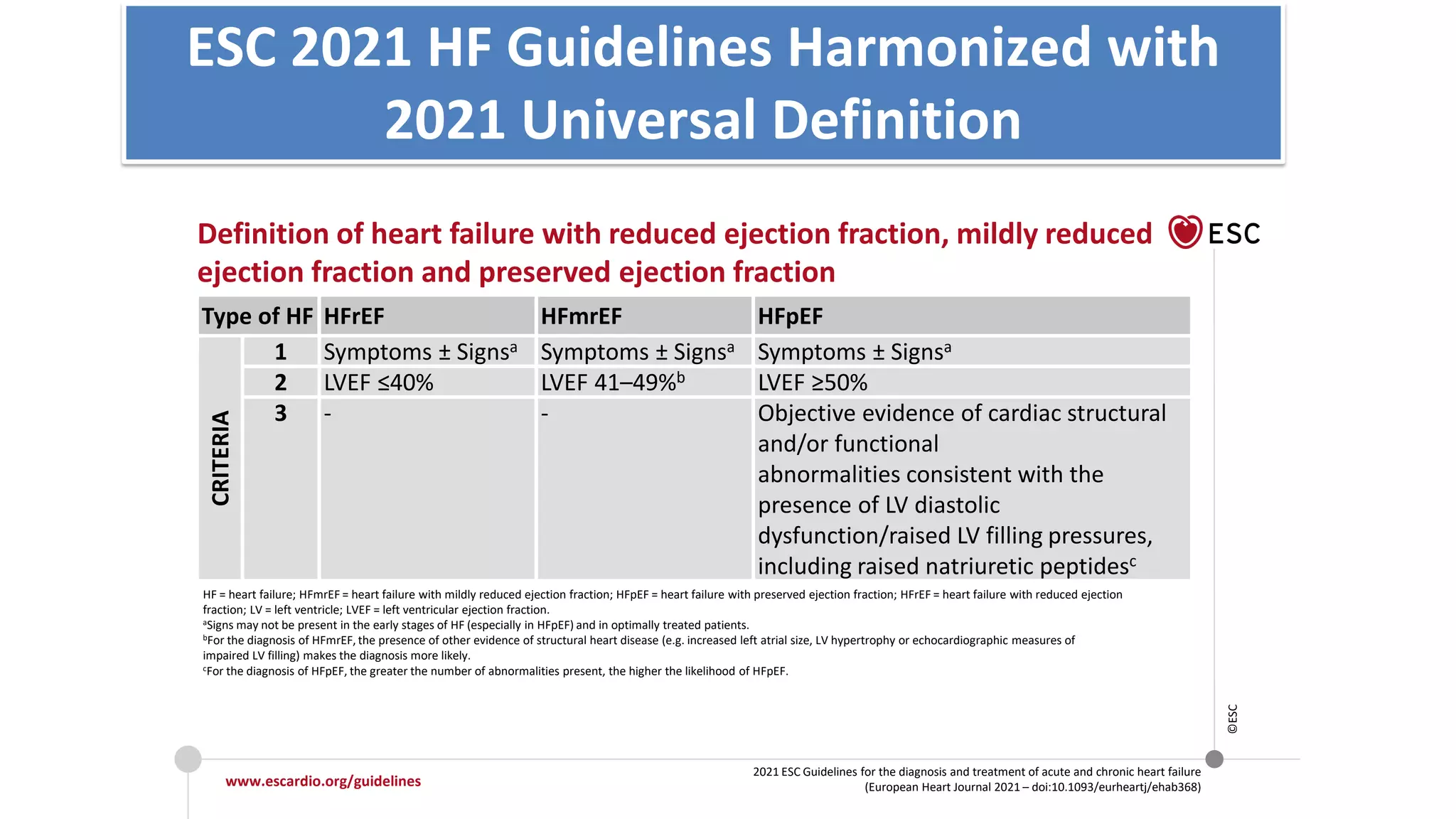
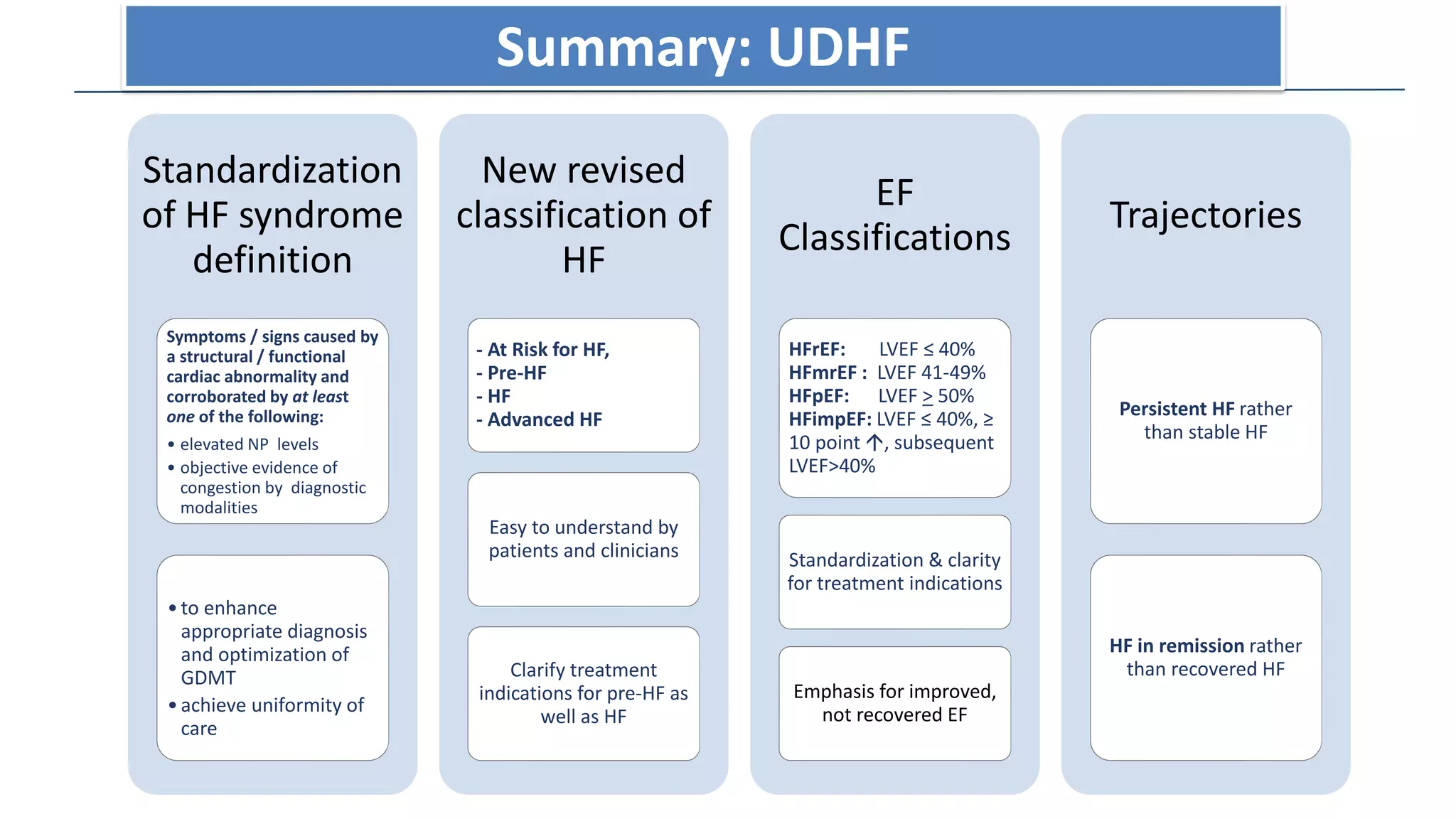
2. The Universal Definition of Heart Failure (UDHF) defines heart failure as a clinical syndrome with current or prior symptoms and/or signs caused by structural and/or functional cardiac abnormalities, as corroborated by elevated natriuretic peptide levels or objective evidence of congestion.
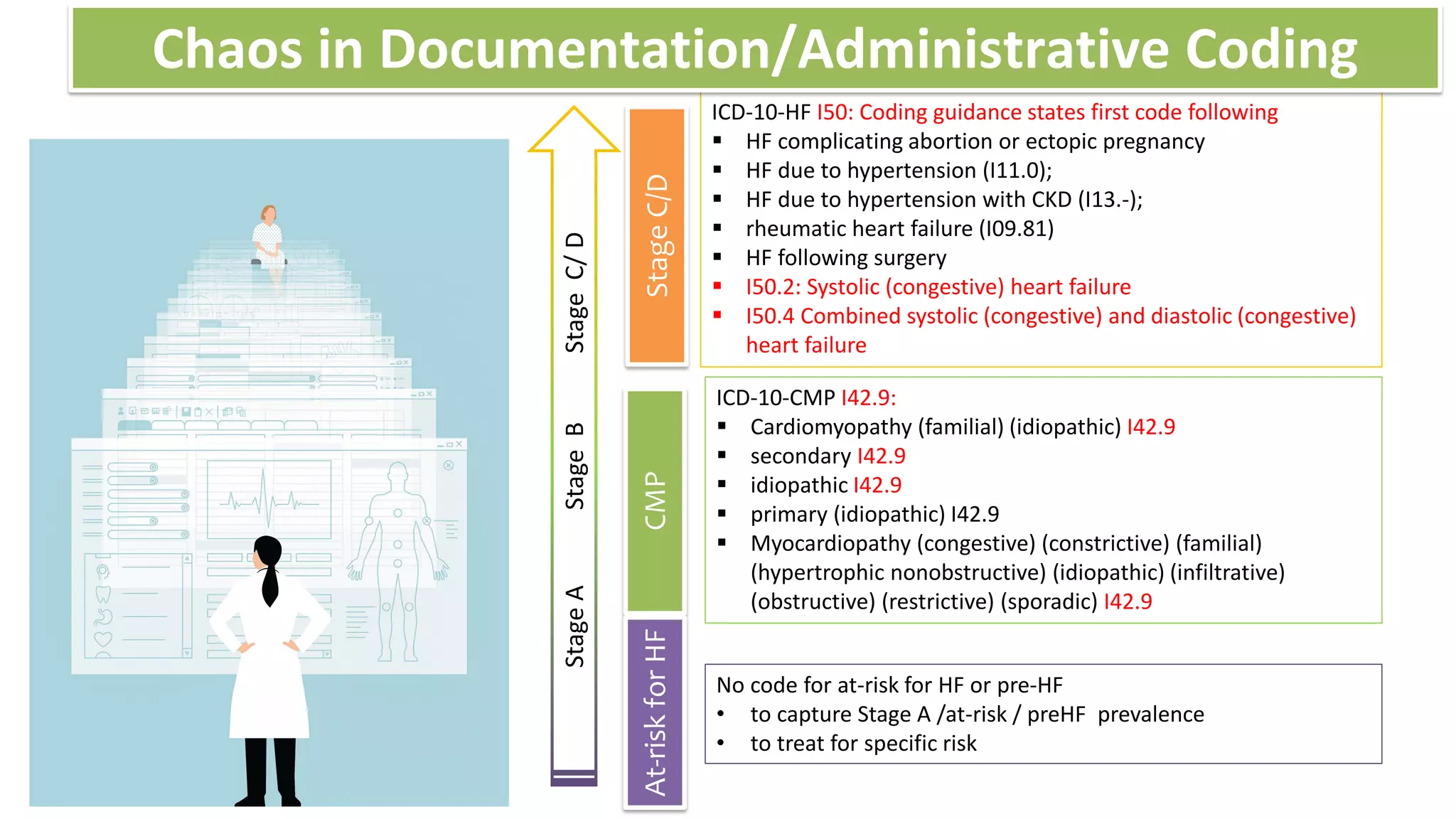
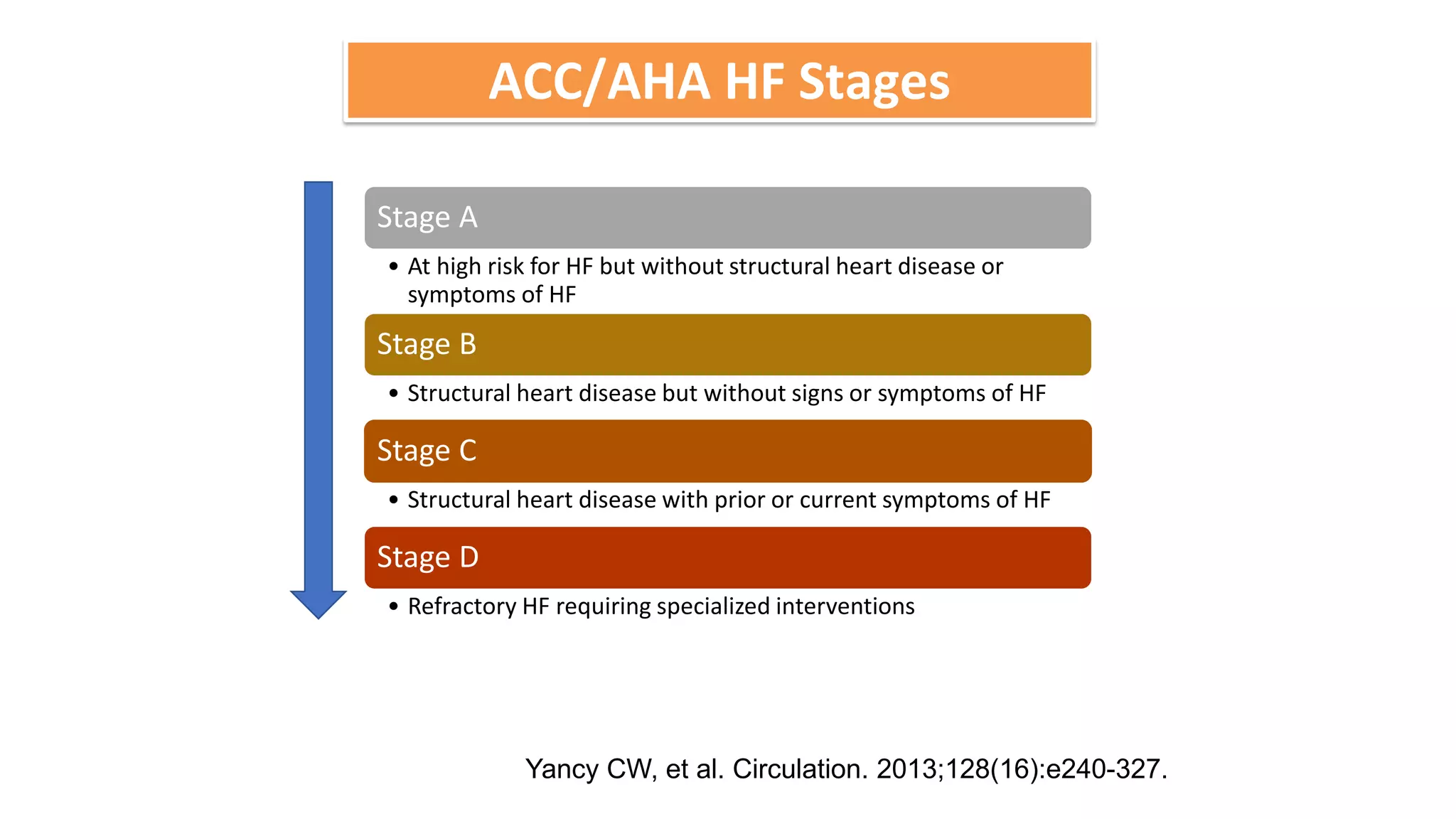
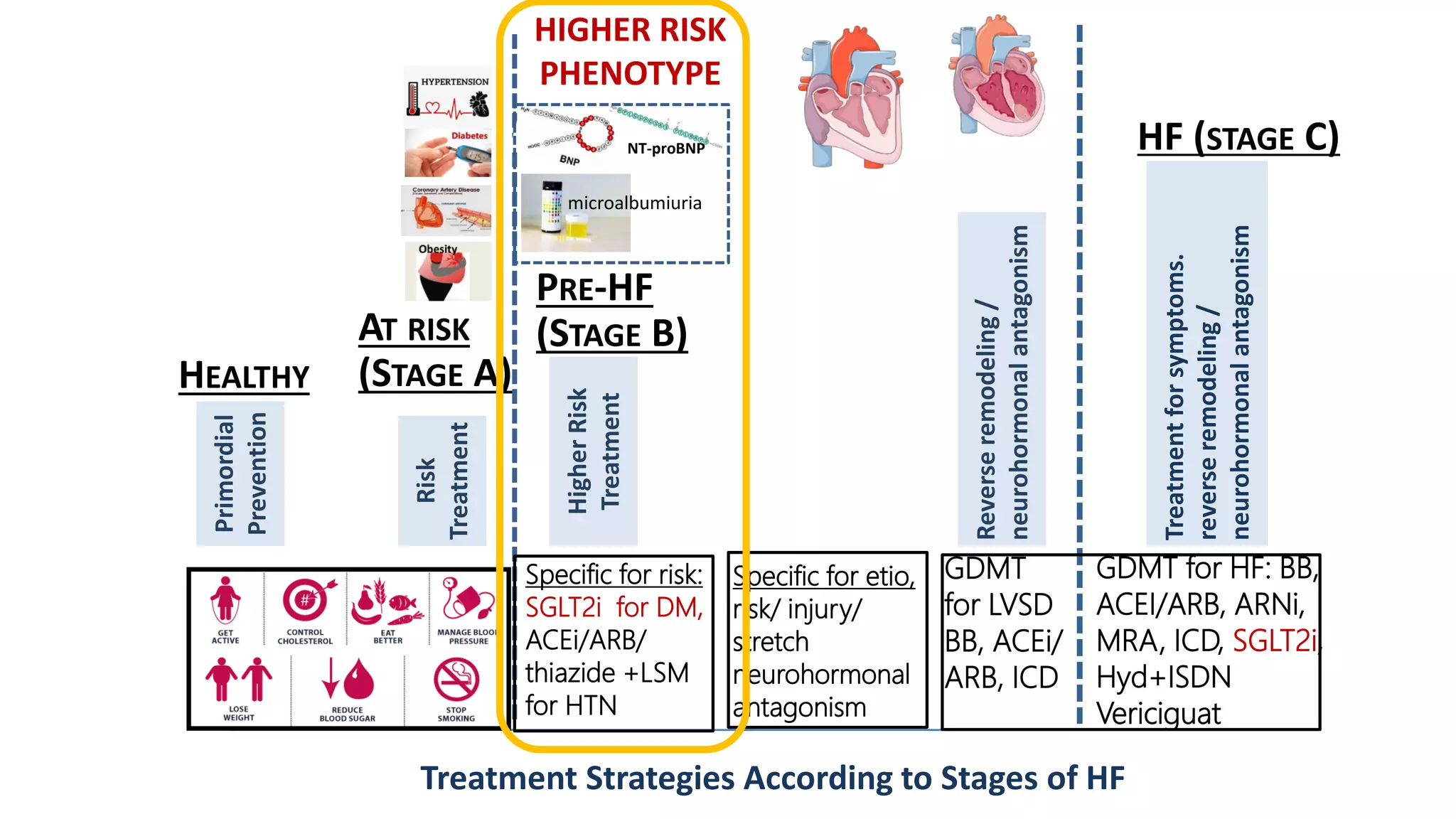
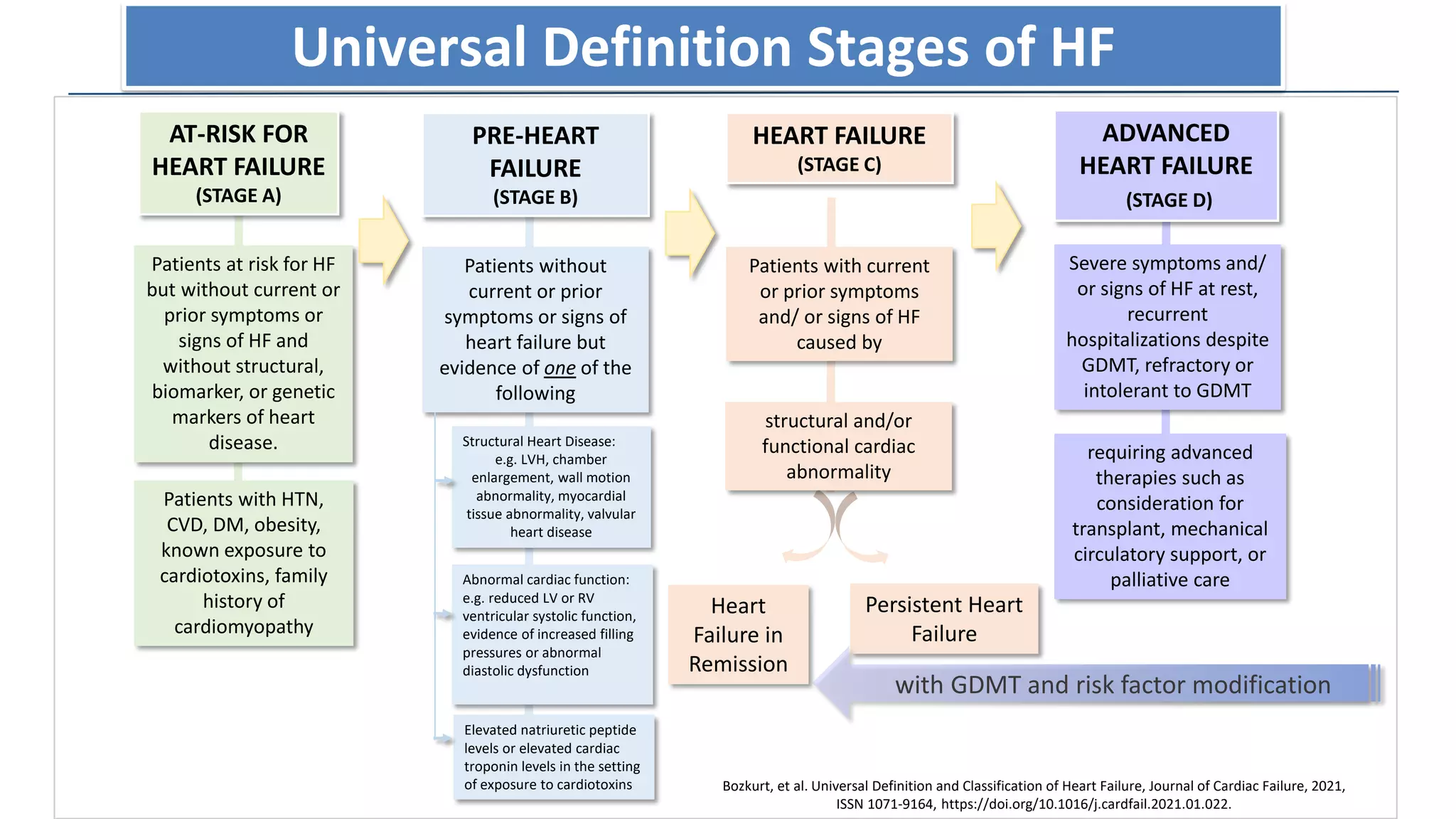
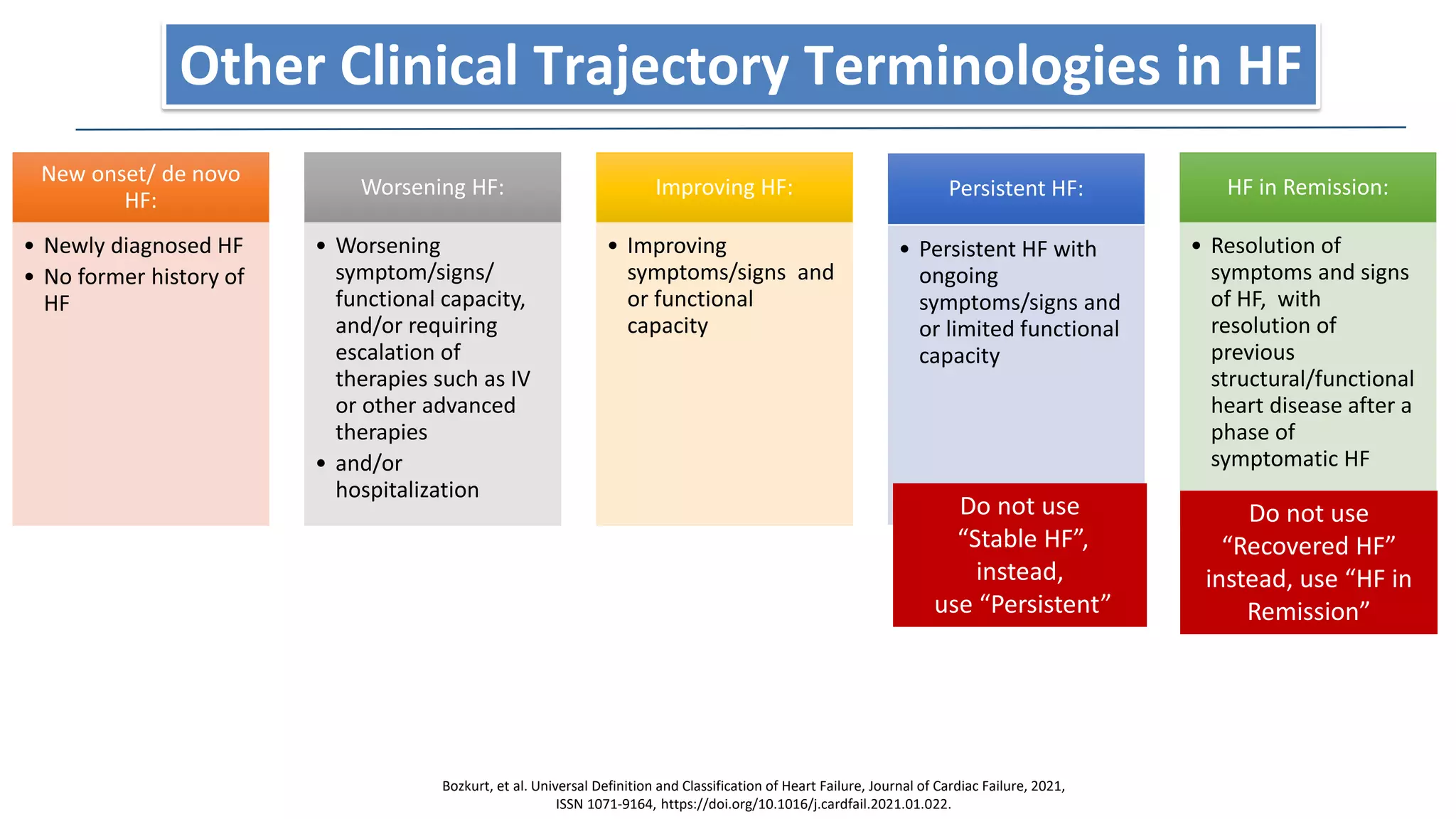
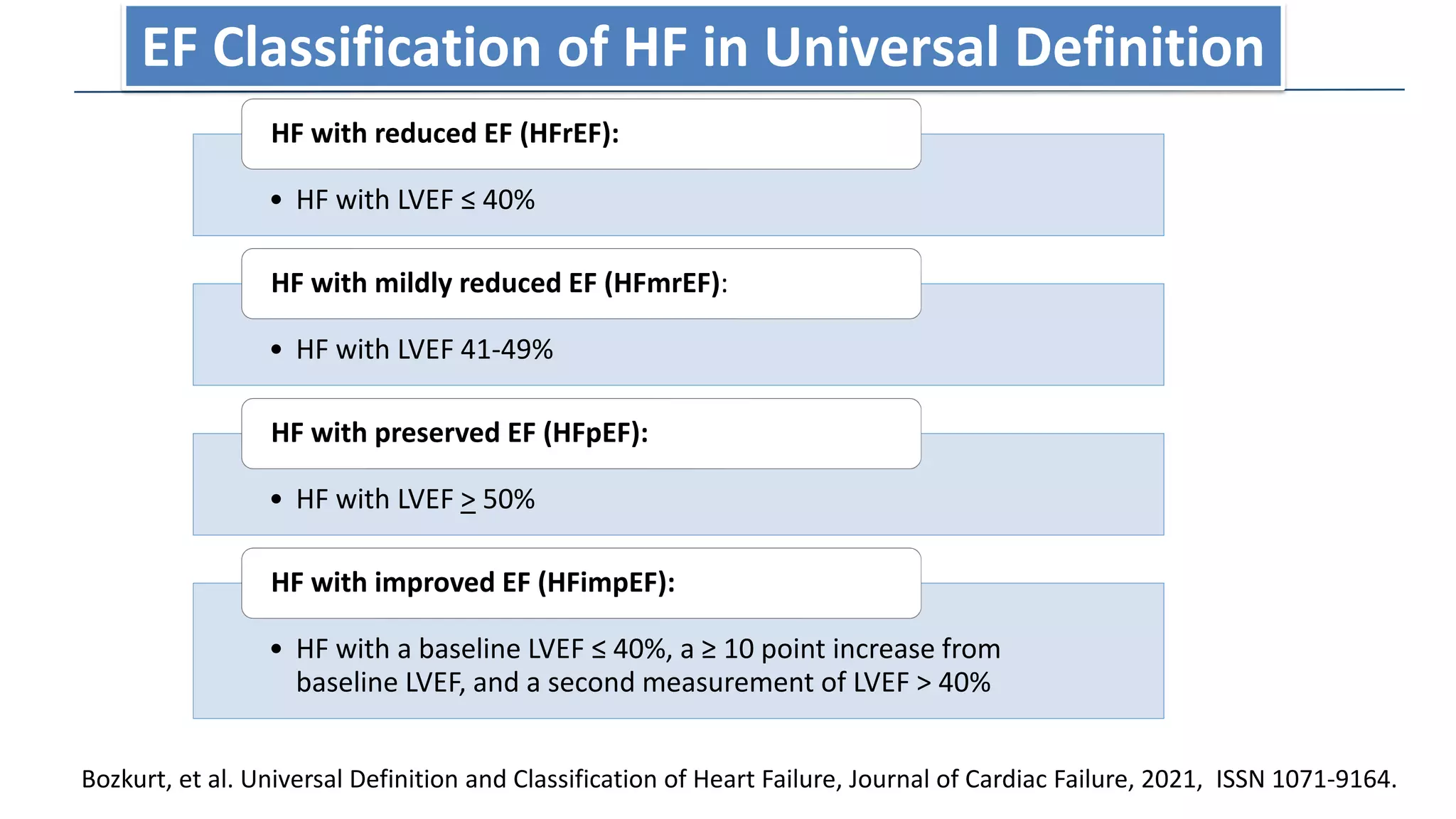
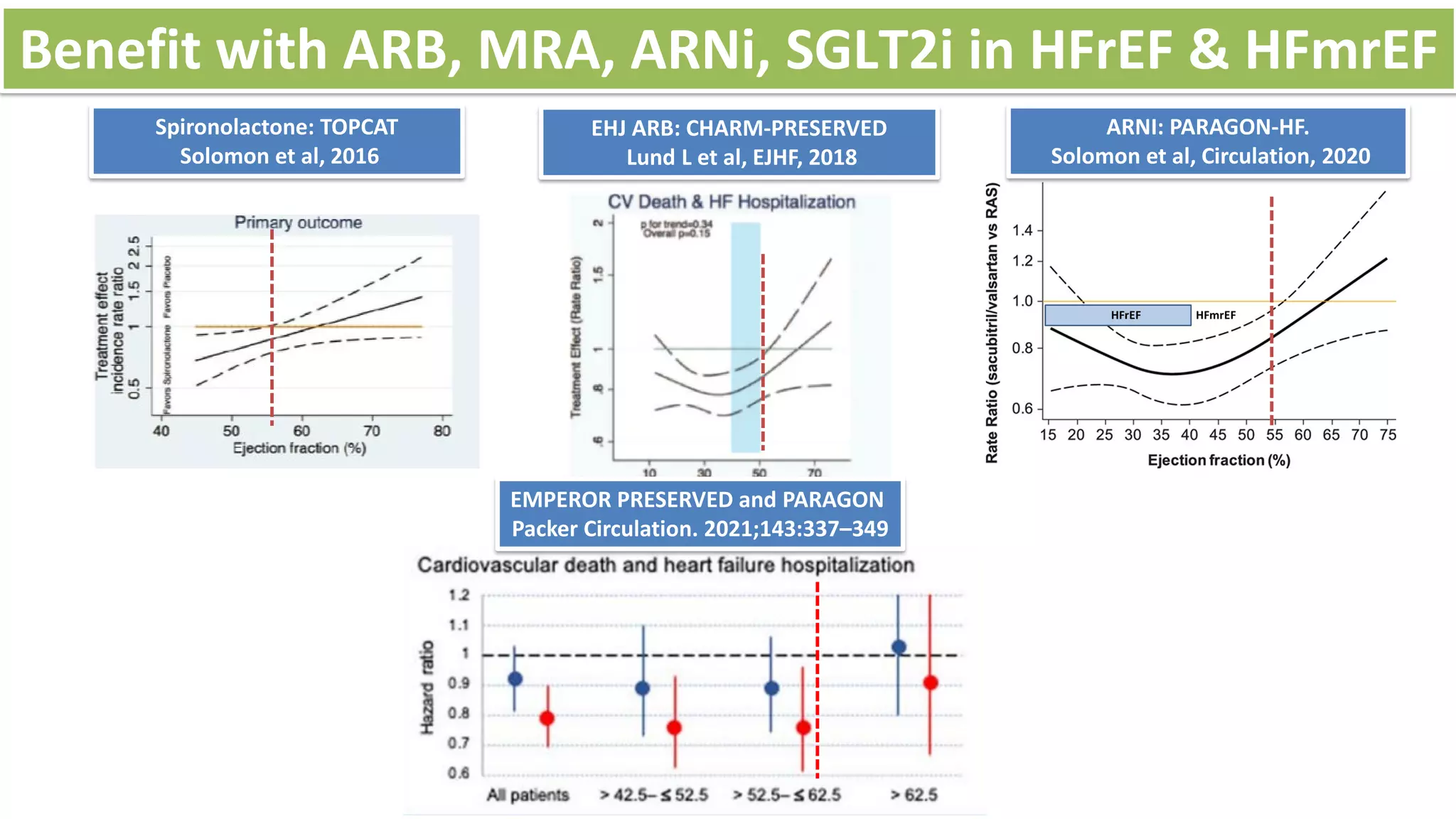
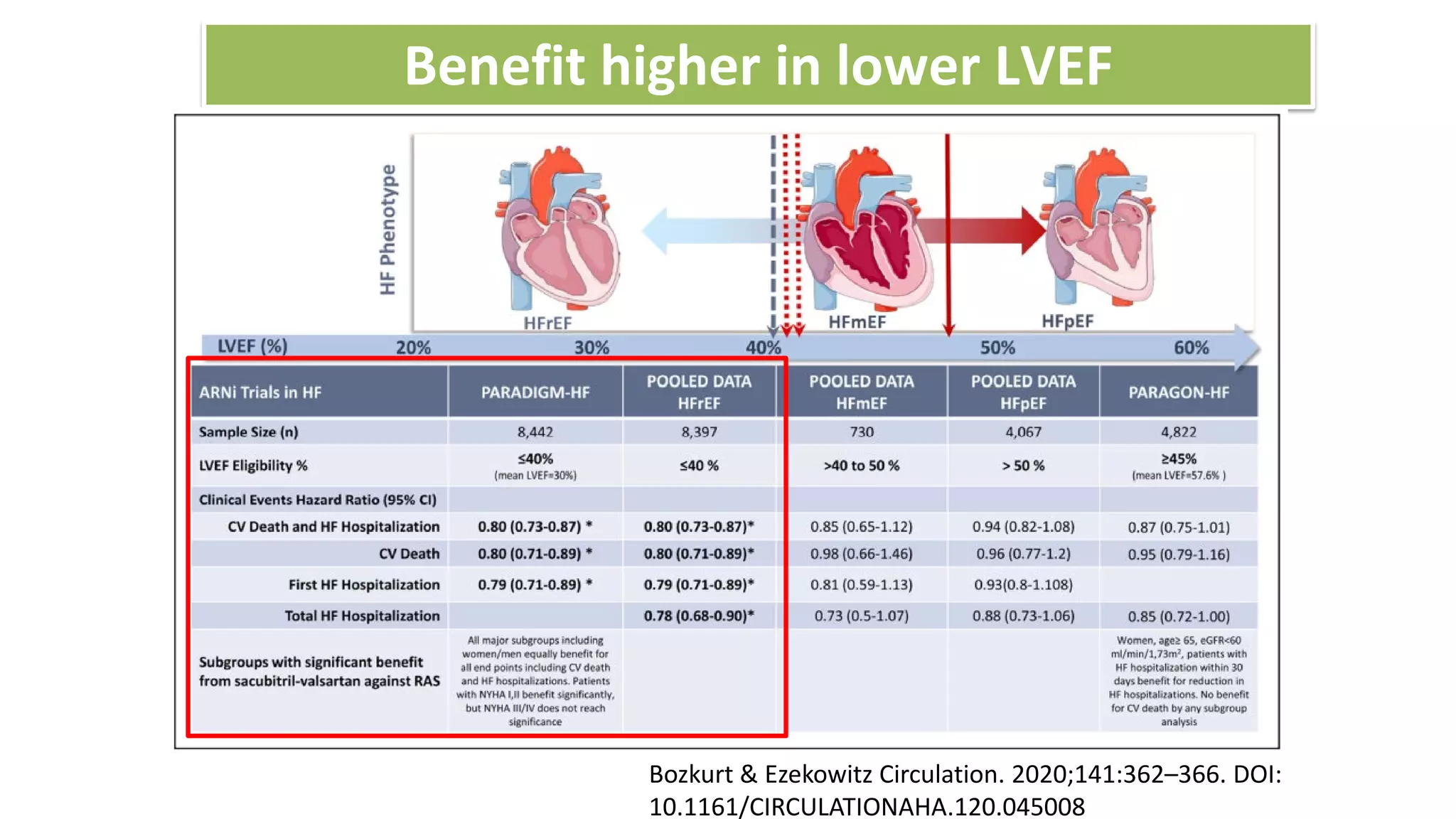
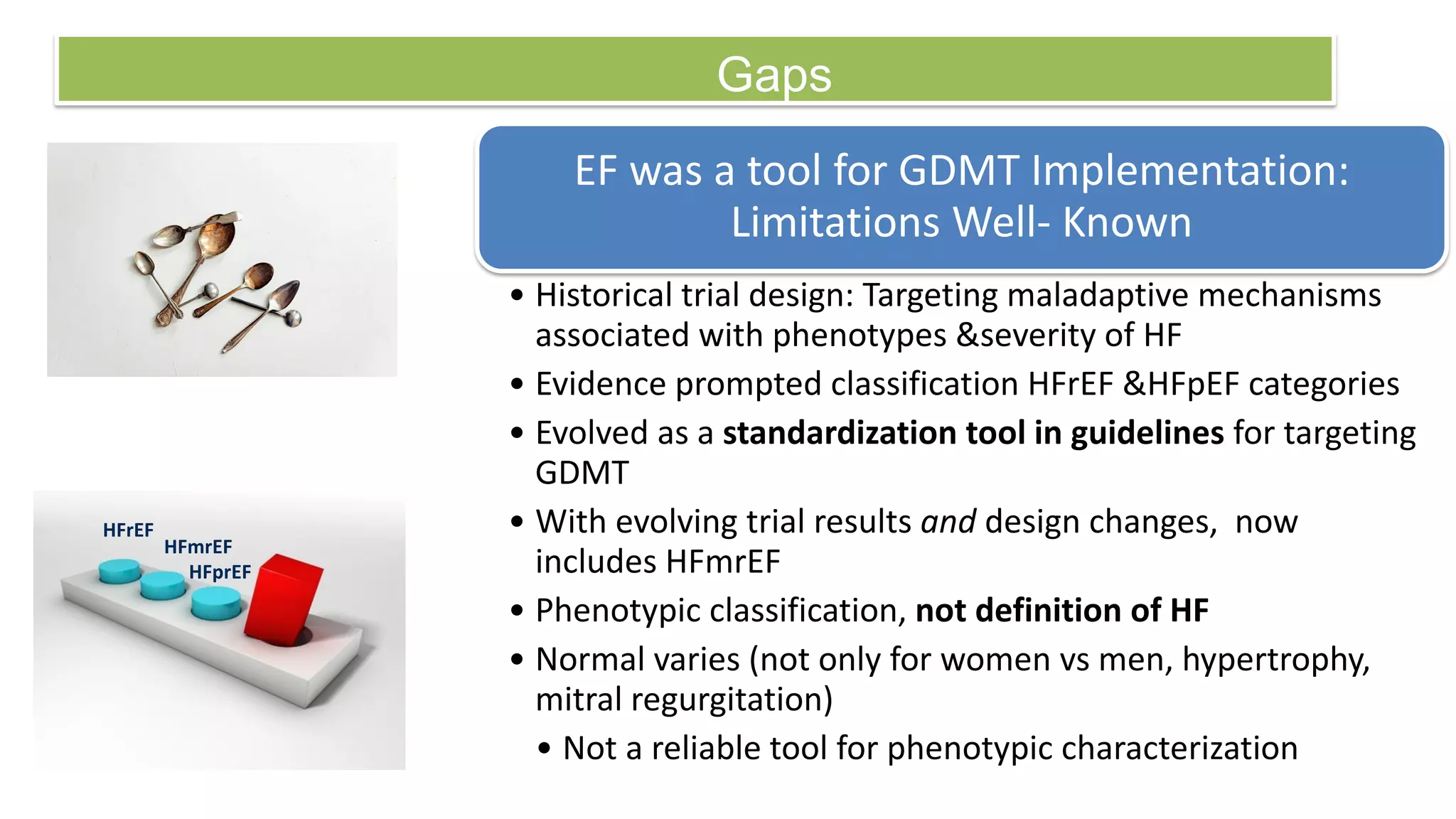
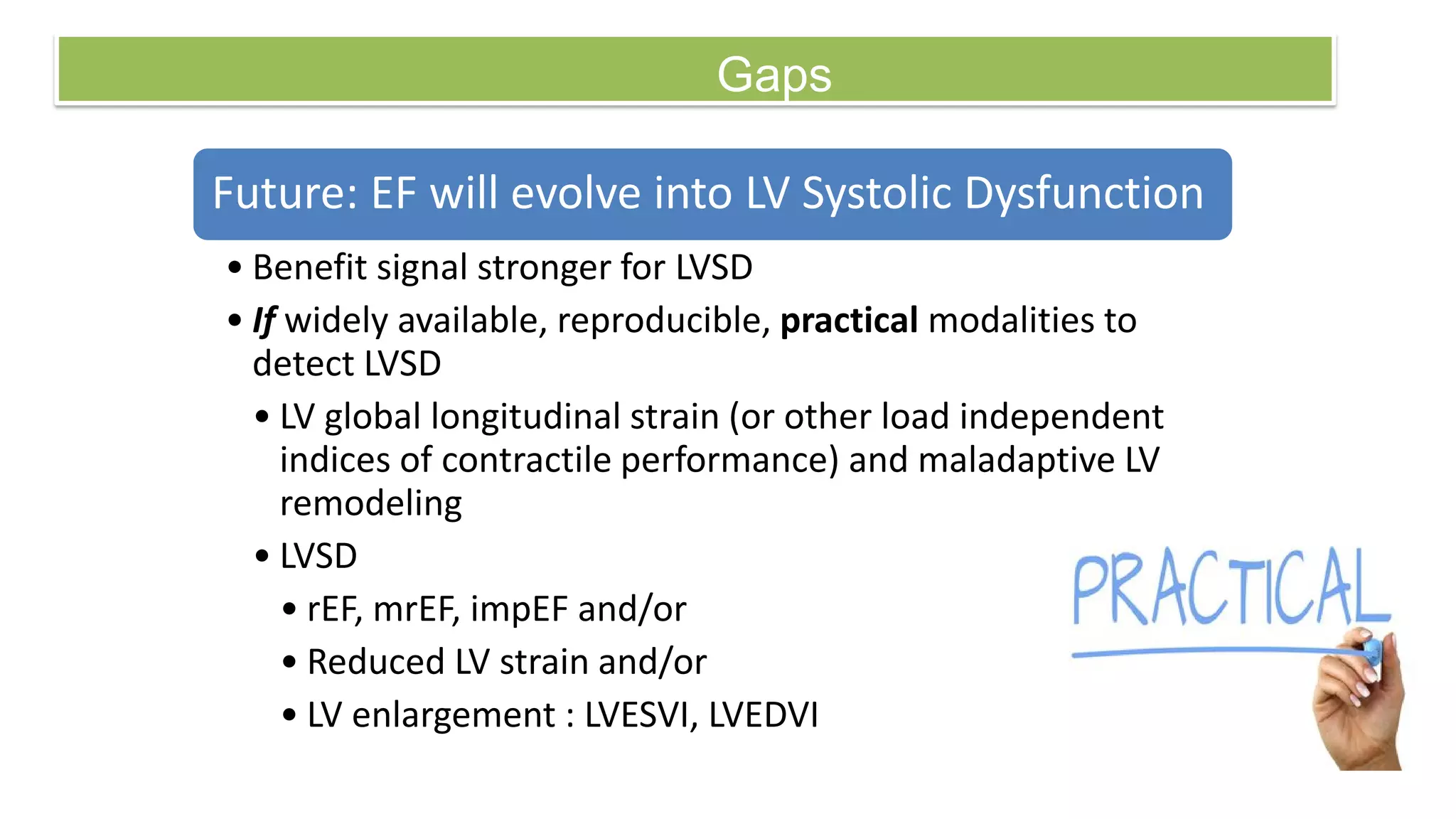
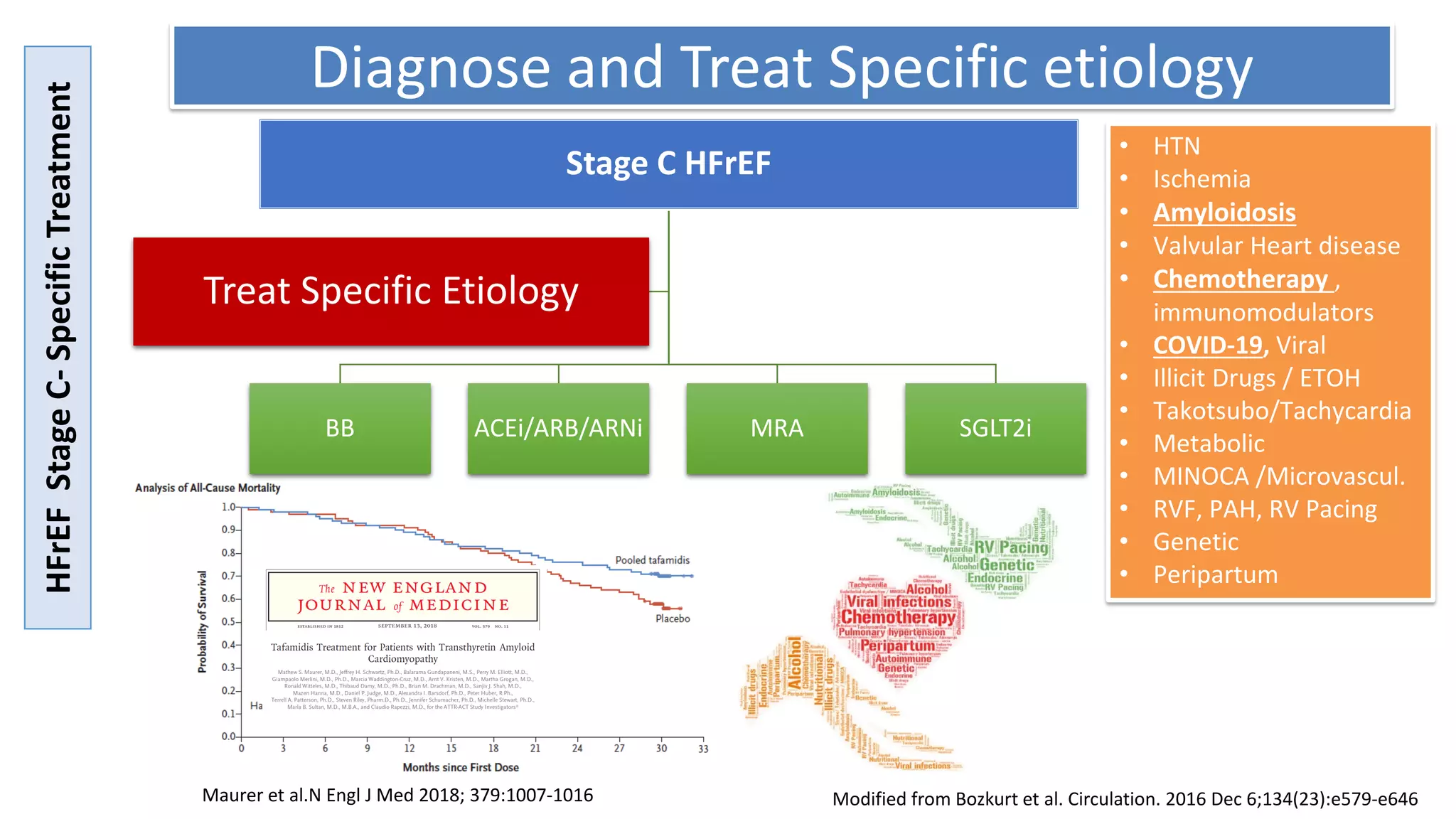
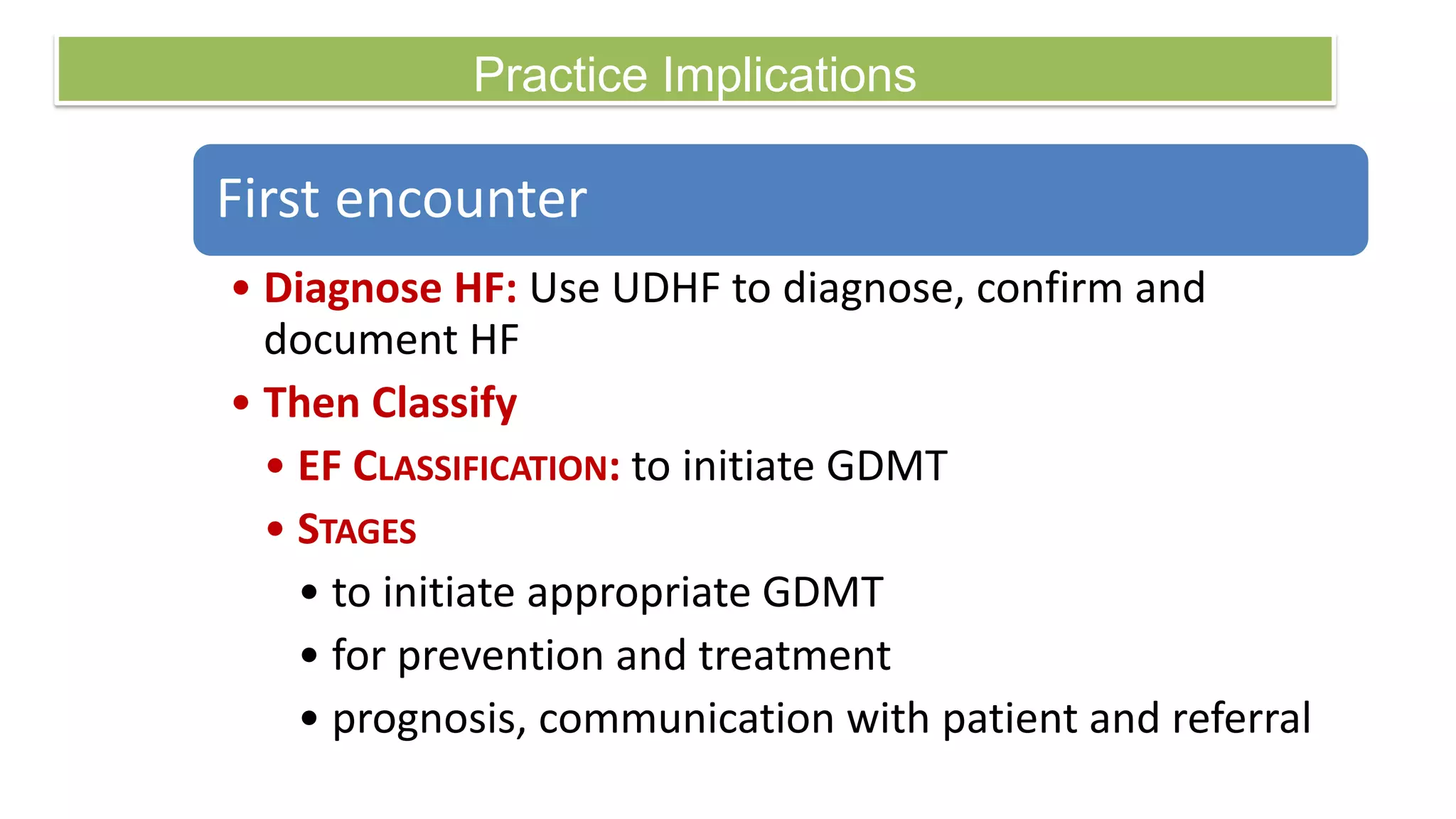
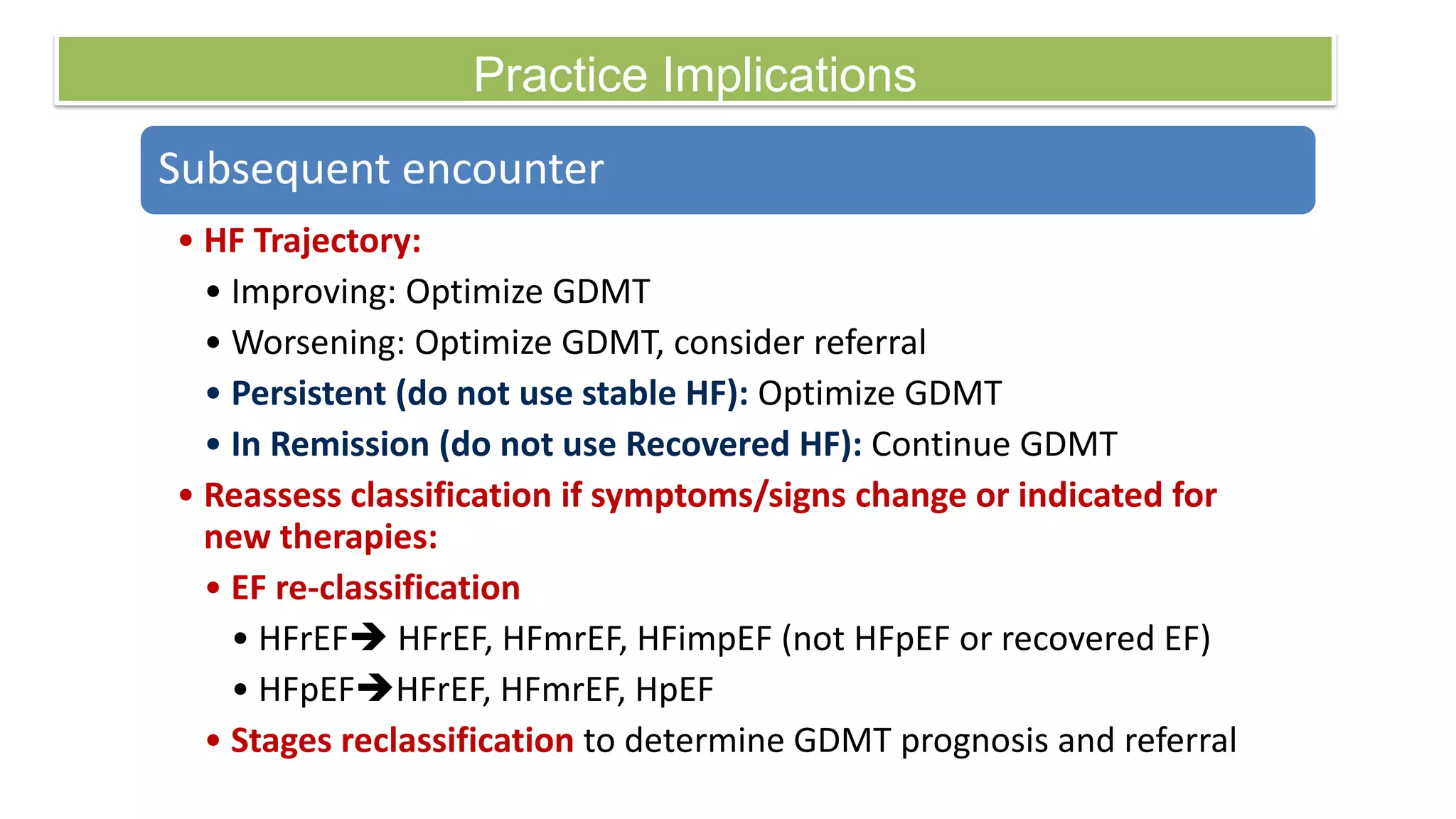
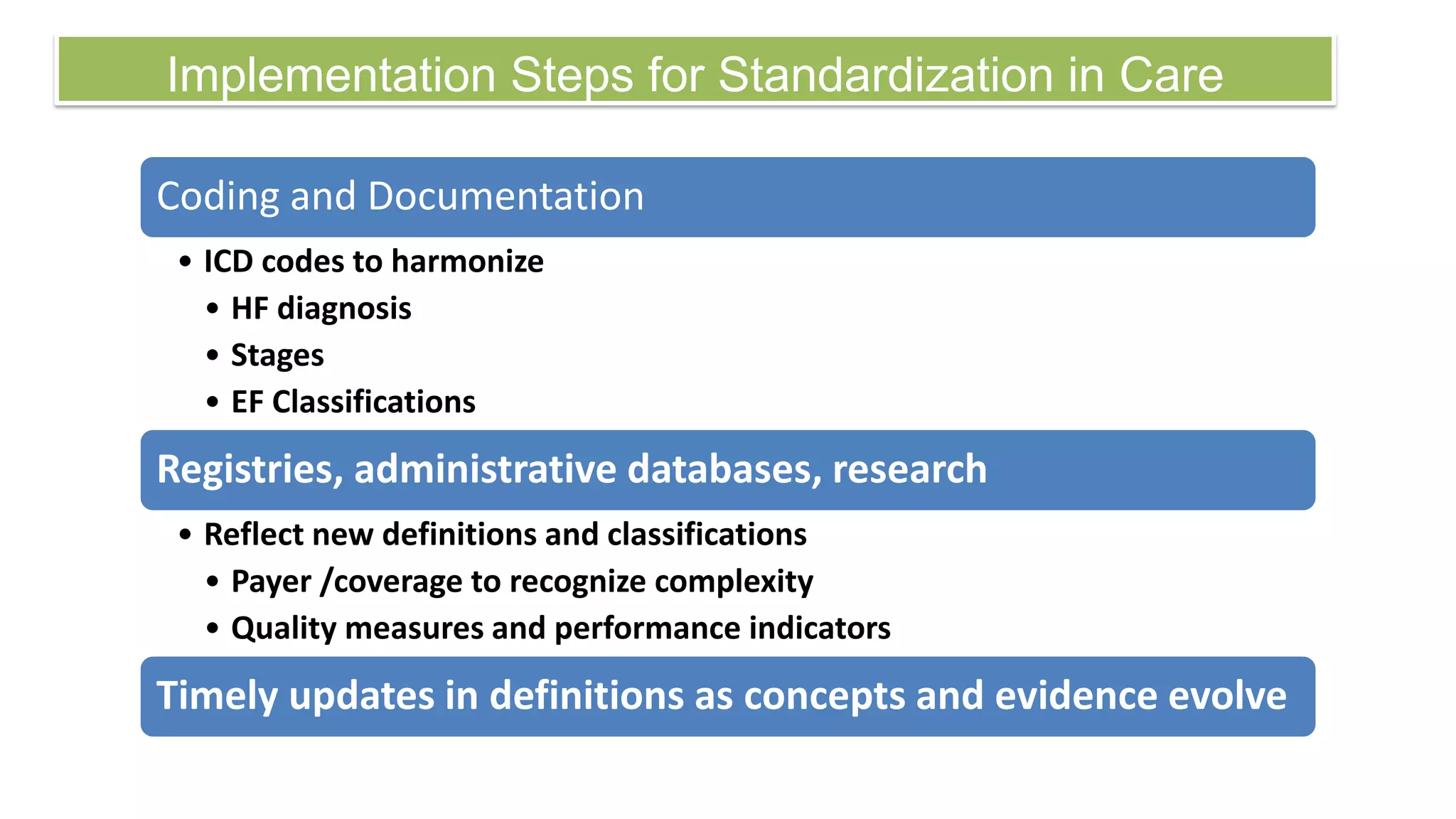
3. The UDHF also establishes a classification system with Stages A through D based on risk, presence of structural heart disease, and severity of symptoms, to help guide treatment strategies according to the stage of heart failure.