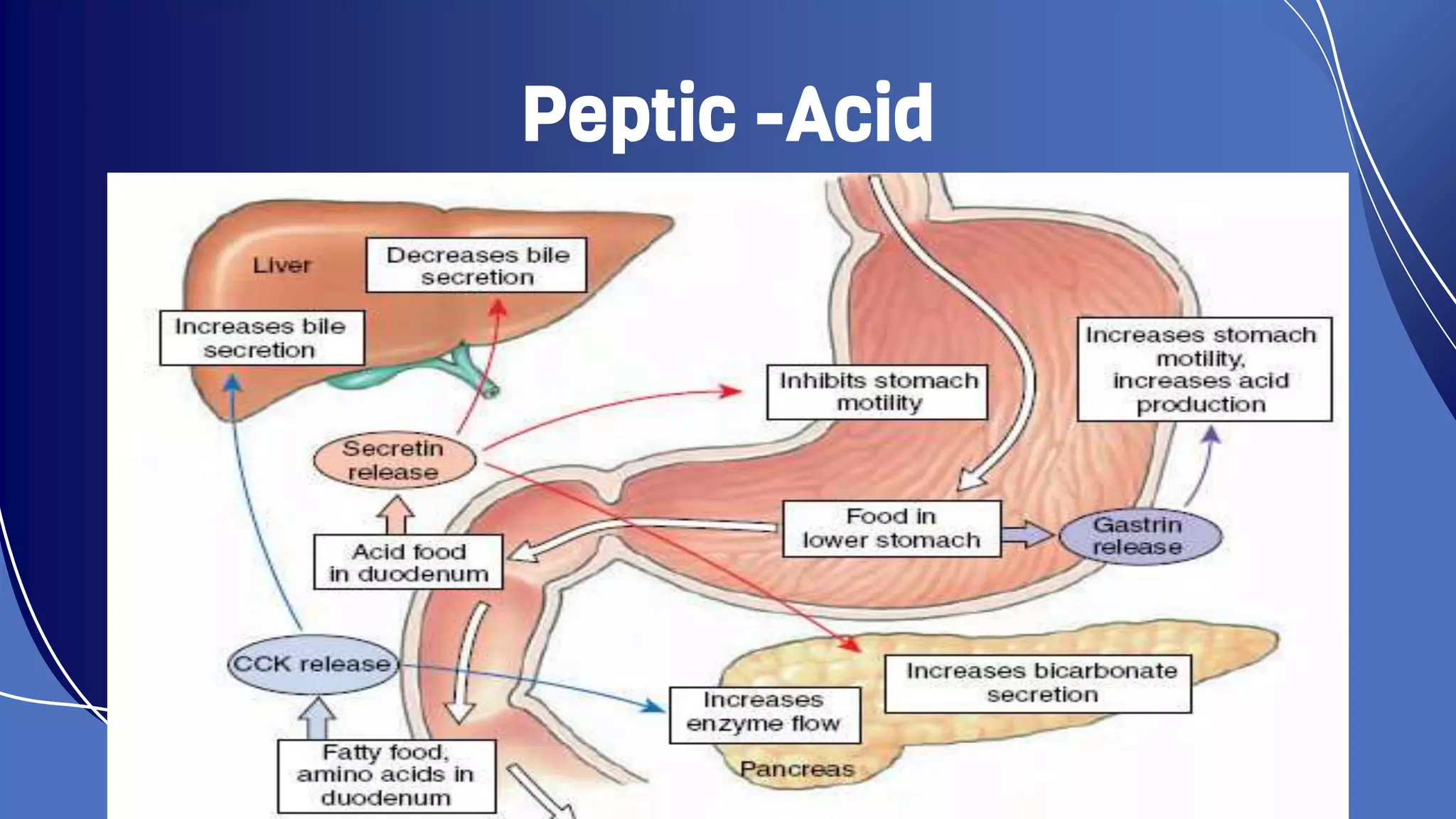
This document summarizes various acid peptic diseases. It defines acid peptic disease as a collection of diseases involving excessive acid secretion or diminished mucosal defense in the stomach and nearby gastrointestinal tract. It then briefly describes several conditions under this category including gastroesophageal reflux disease (GERD), gastritis, gastric ulcer, duodenal ulcer, esophageal ulcer, Zollinger-Ellison syndrome, and Meckel's diverticulum ulcer. For each condition, it provides details on symptoms, causes, diagnostic methods, and treatment approaches.