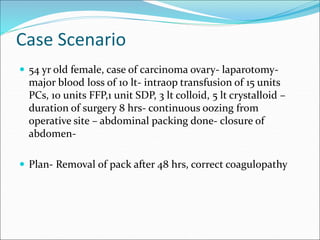
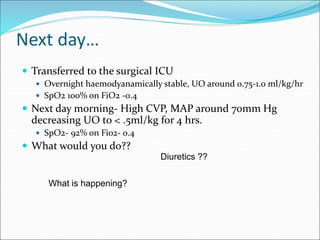
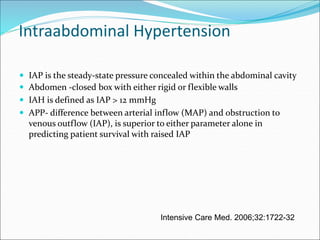
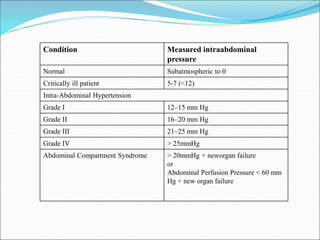
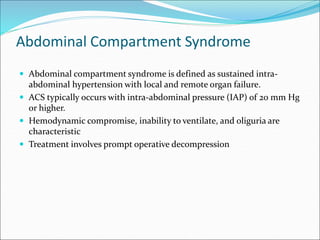
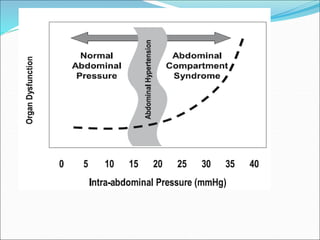
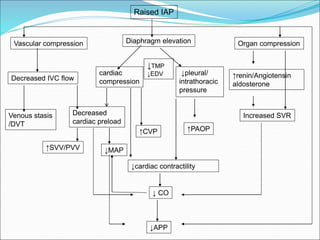
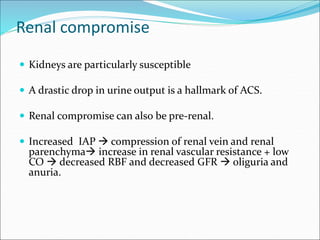
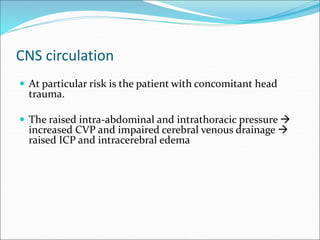
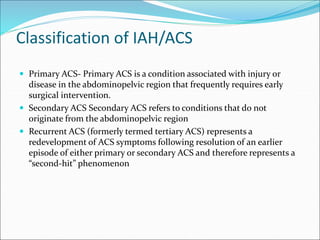
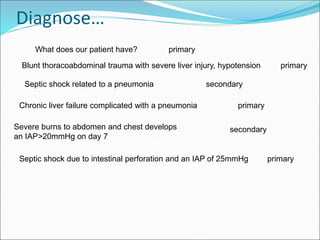
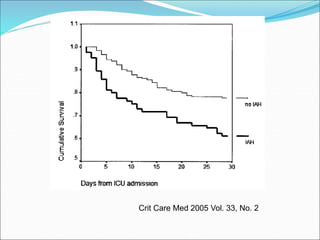
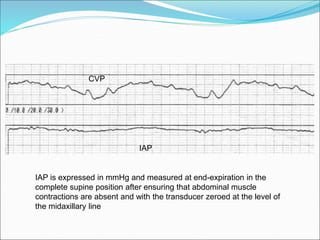
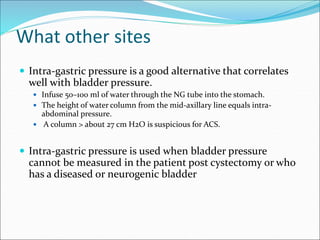
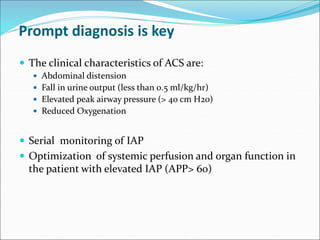
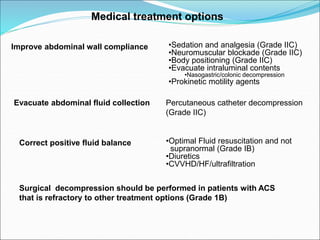
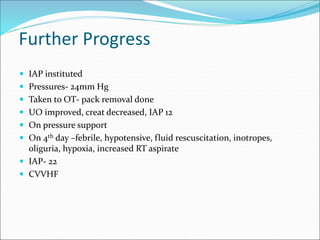
A 54-year old female underwent a major surgery for carcinoma ovary with significant blood loss requiring multiple transfusions. Post-operatively she developed signs of intra-abdominal hypertension including decreased urine output, elevated CVP and hypotension. Her intra-abdominal pressure was measured to be over 20 mmHg consistent with abdominal compartment syndrome, a condition where elevated intra-abdominal pressure compromises organ function. She required surgical decompression to relieve the pressure and allow organ recovery.