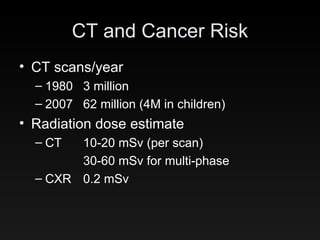
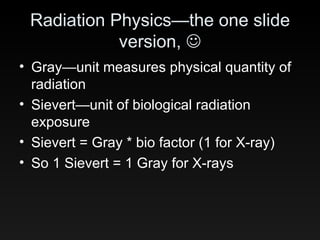
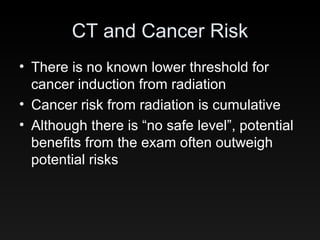
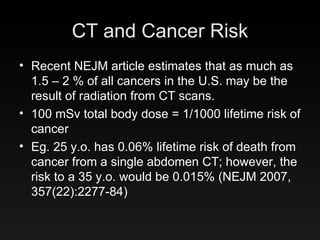
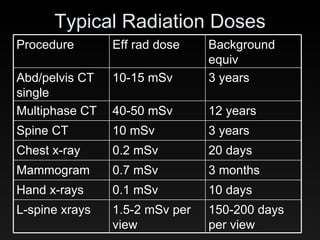
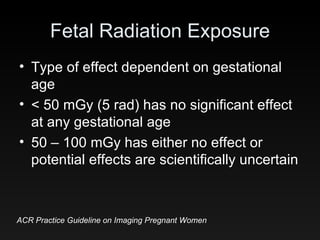
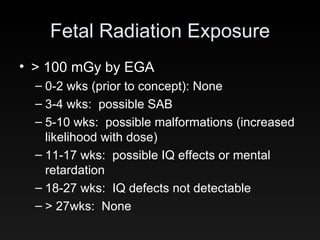
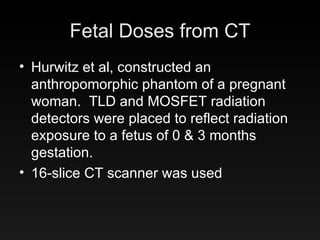
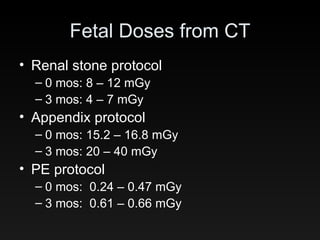
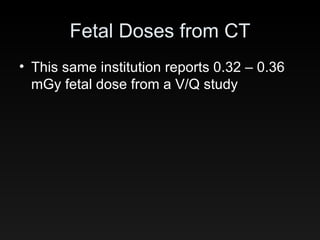
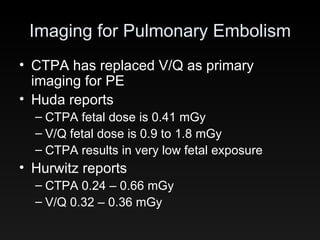
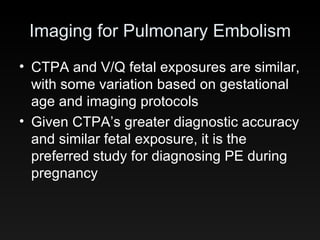
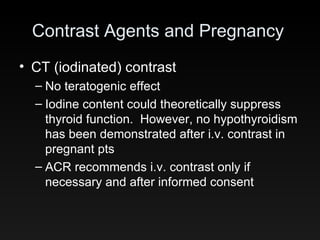
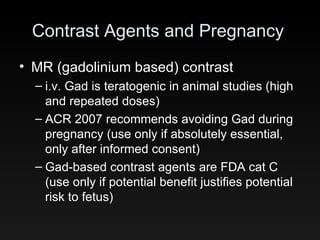
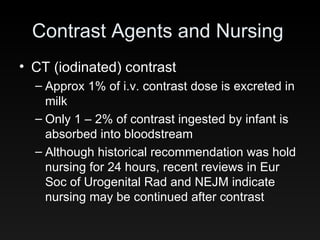
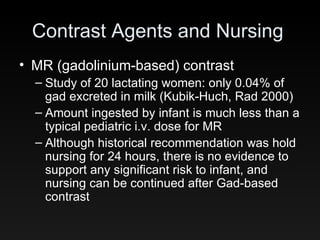
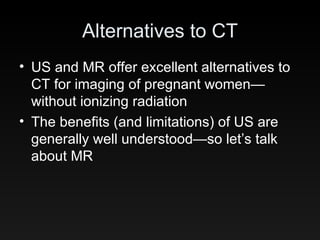
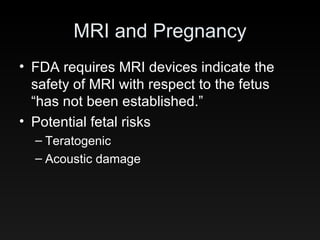
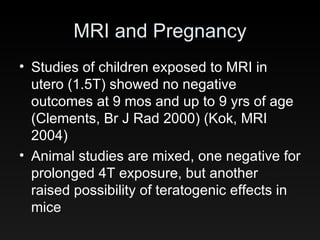
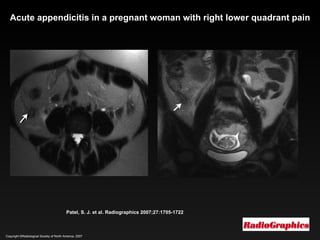
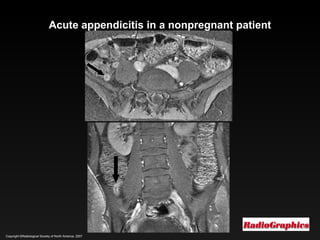
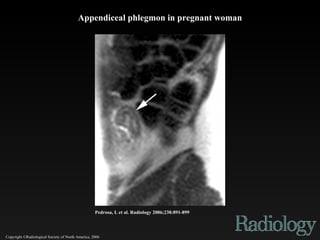
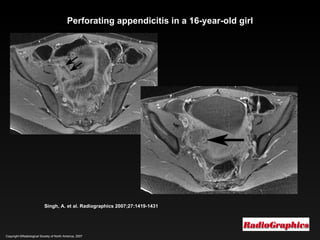
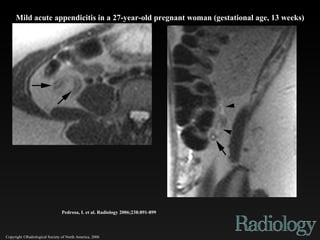
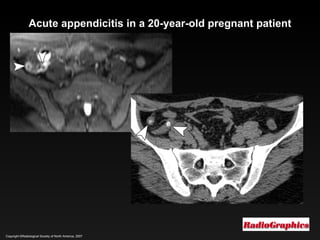
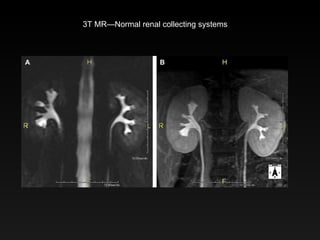
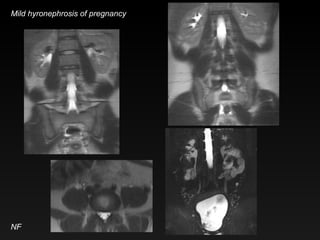
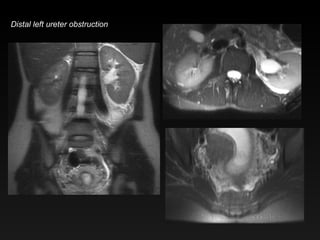
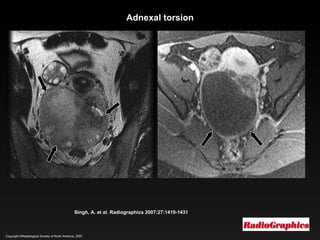
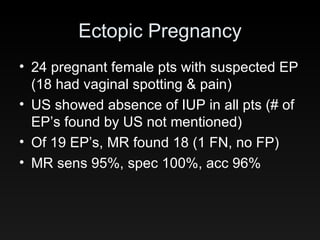
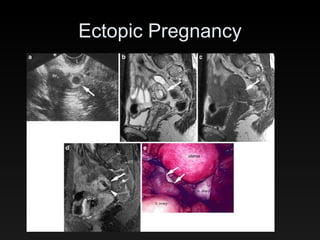
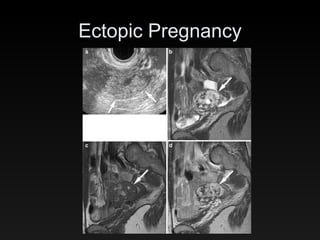
The document discusses the implications of maternal imaging during pregnancy, focusing on the radiation risks associated with CT scans and their potential effects on fetal health. It highlights the cumulative nature of radiation exposure and the associated cancer risks, while also presenting guidelines on imaging practices for pregnant women. Additionally, it compares imaging modalities such as CT and MRI, emphasizing the safety and diagnostic accuracy of MRI as a preferable alternative for certain conditions in pregnant patients.