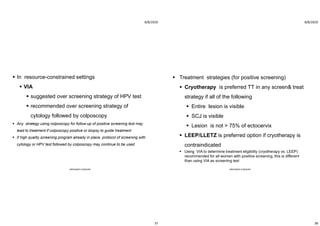
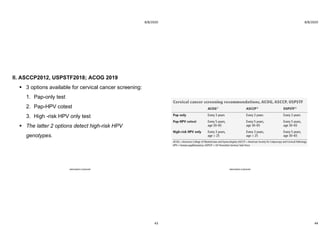
This document discusses guidelines for human papillomavirus (HPV) and cervical cancer prevention and screening. It covers HPV types and infection, how HPV infection can lead to cancer, and risk factors. It discusses three main approaches to cervical cancer prevention - primary prevention through HPV vaccination, secondary prevention via screening and treatment of precancerous lesions, and tertiary prevention. The document provides details on HPV vaccines, screening recommendations, challenges to vaccination, and treatment options.