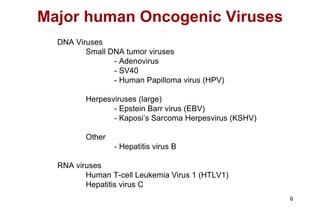
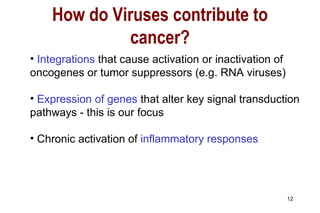
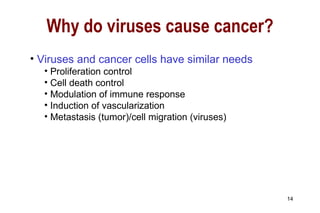
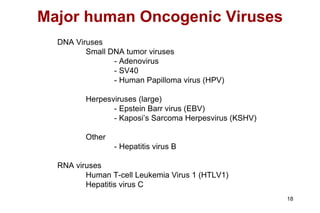
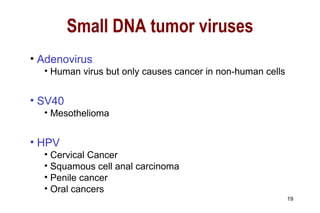
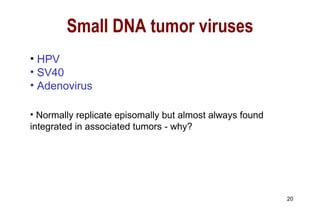
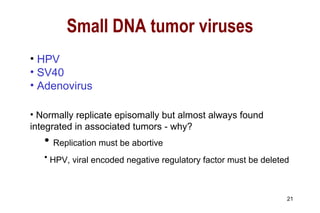
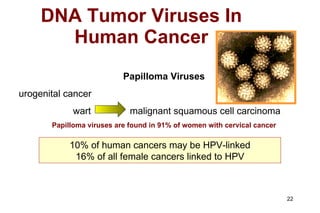
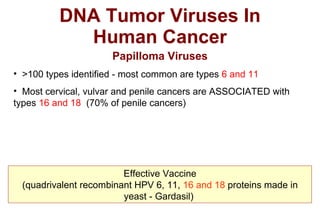
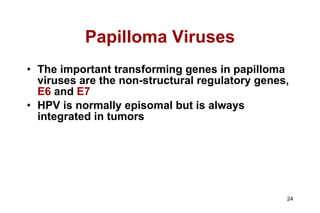
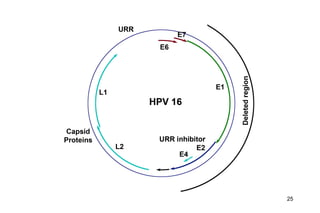
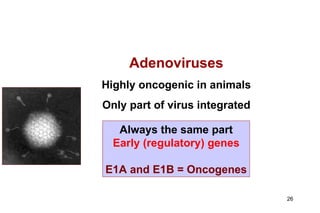
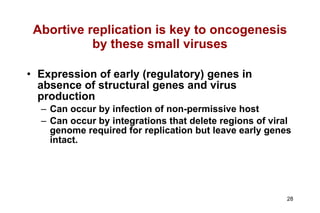
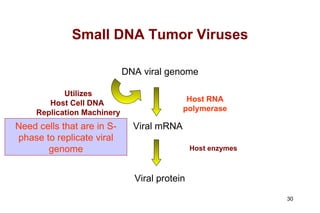
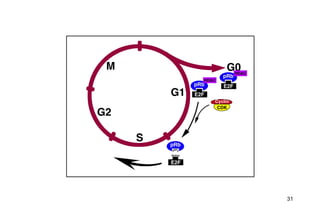
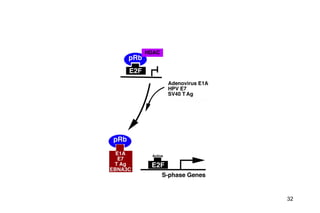
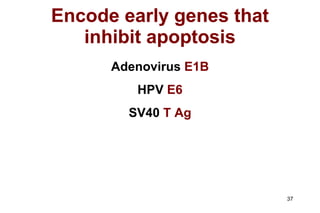
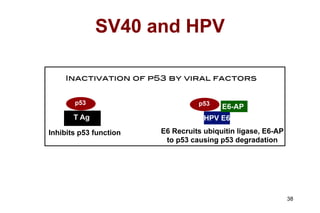
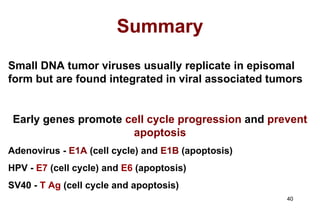
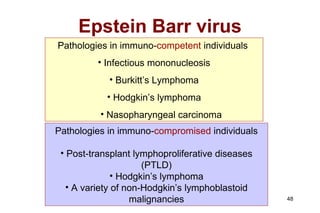
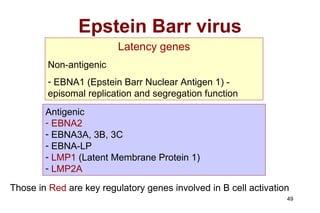
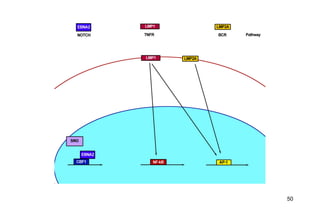
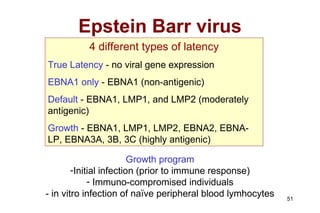
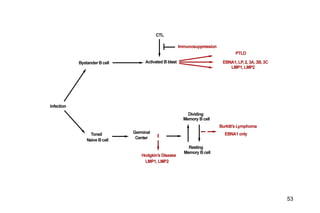
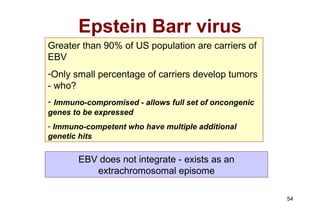
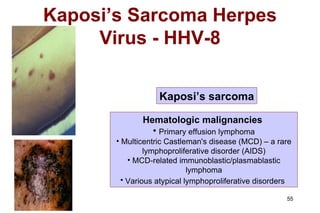
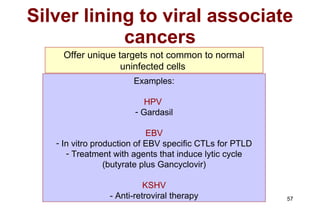
Viruses can cause cancer through several mechanisms. Small DNA tumor viruses like HPV and adenovirus often integrate into the host genome and express early genes that promote cell cycle progression and prevent apoptosis. This leads to uncontrolled cell growth. Herpesviruses like EBV and KSHV can cause cancer during their latency phase by expressing genes that induce cell activation and proliferation programs. Chronic viral infections may also cause cancer over long periods through prolonged inflammation. Studying virus-associated cancers provides insights into cancer mechanisms and potential new targets for treatment.