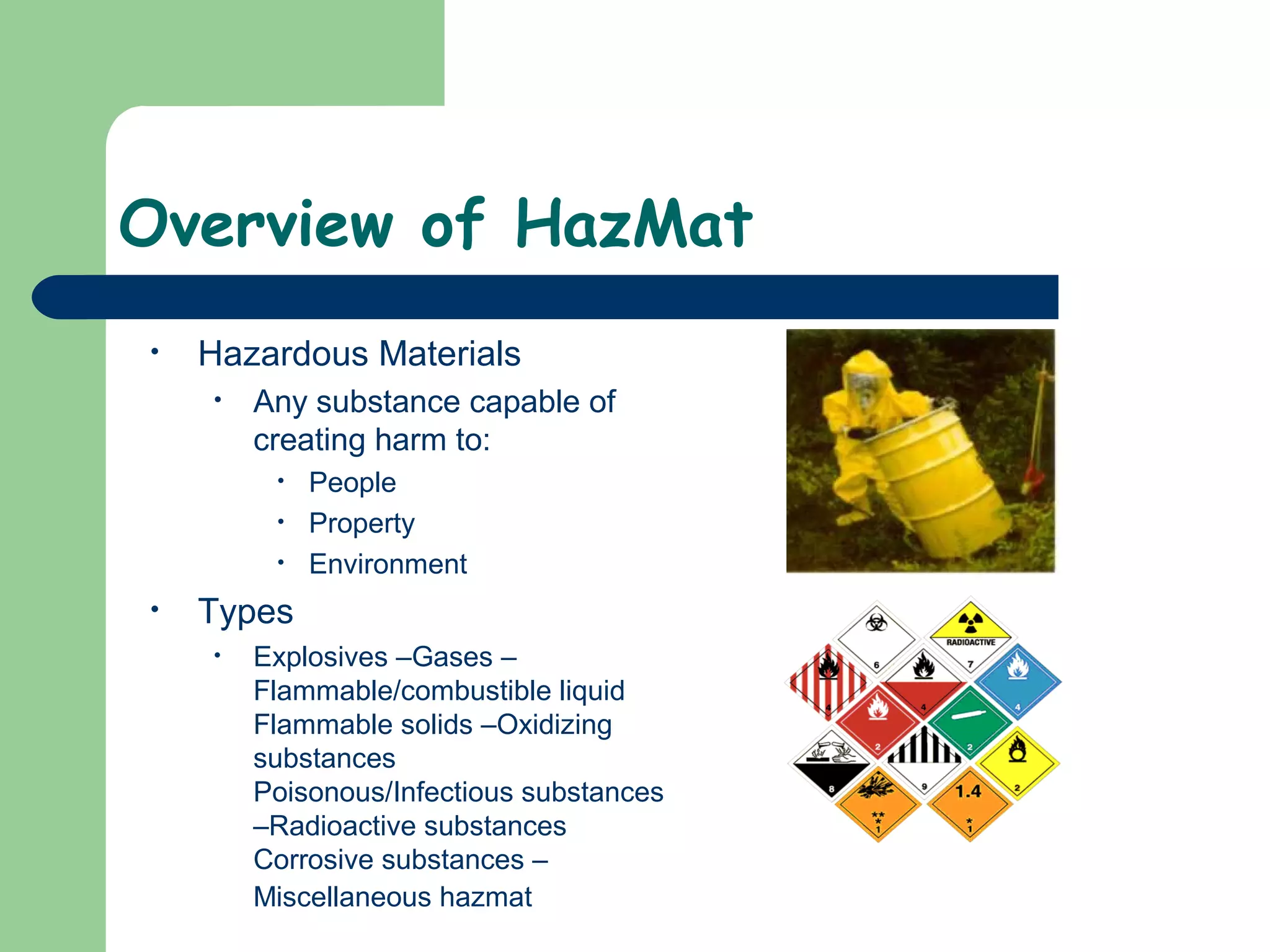
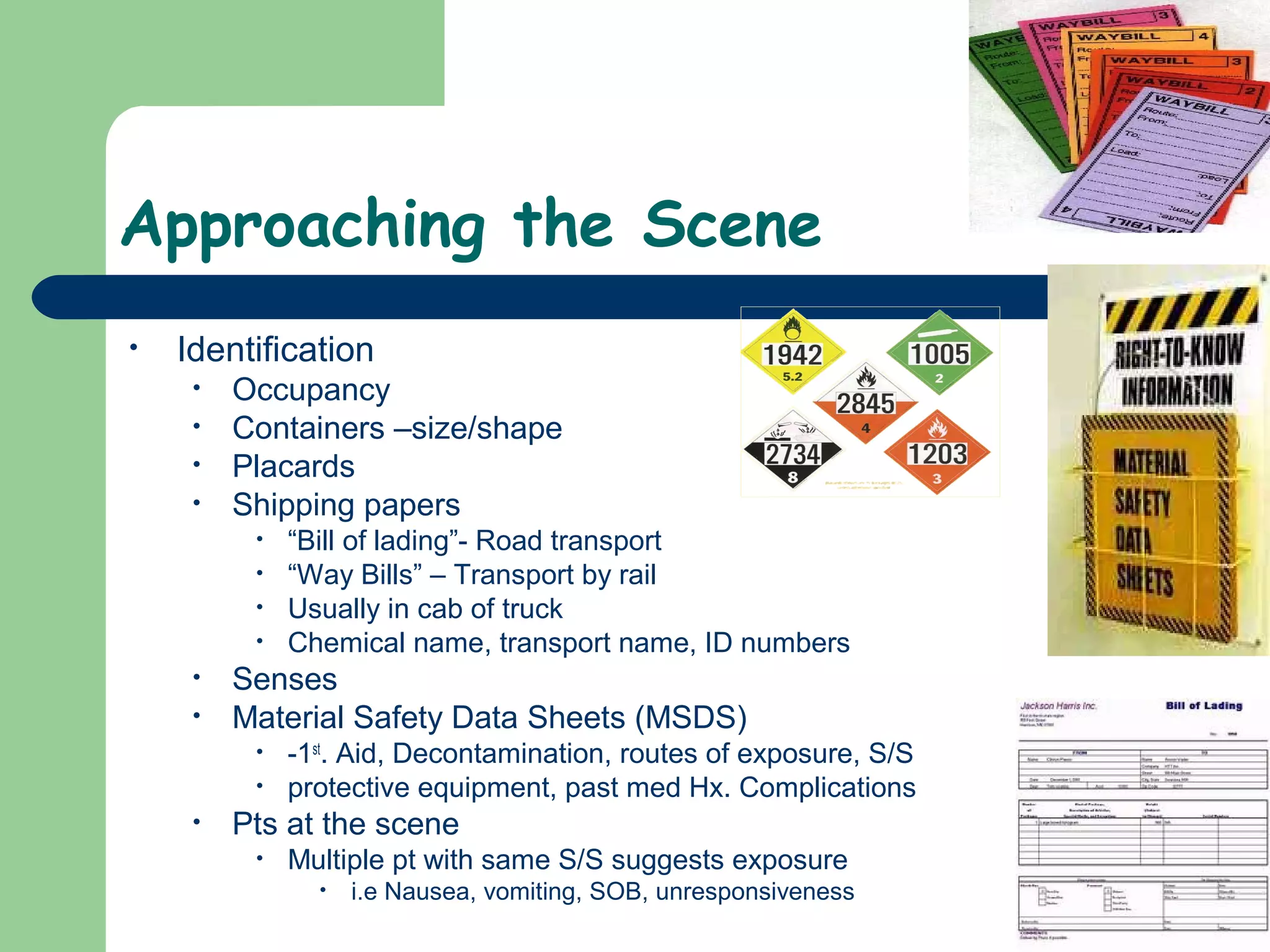
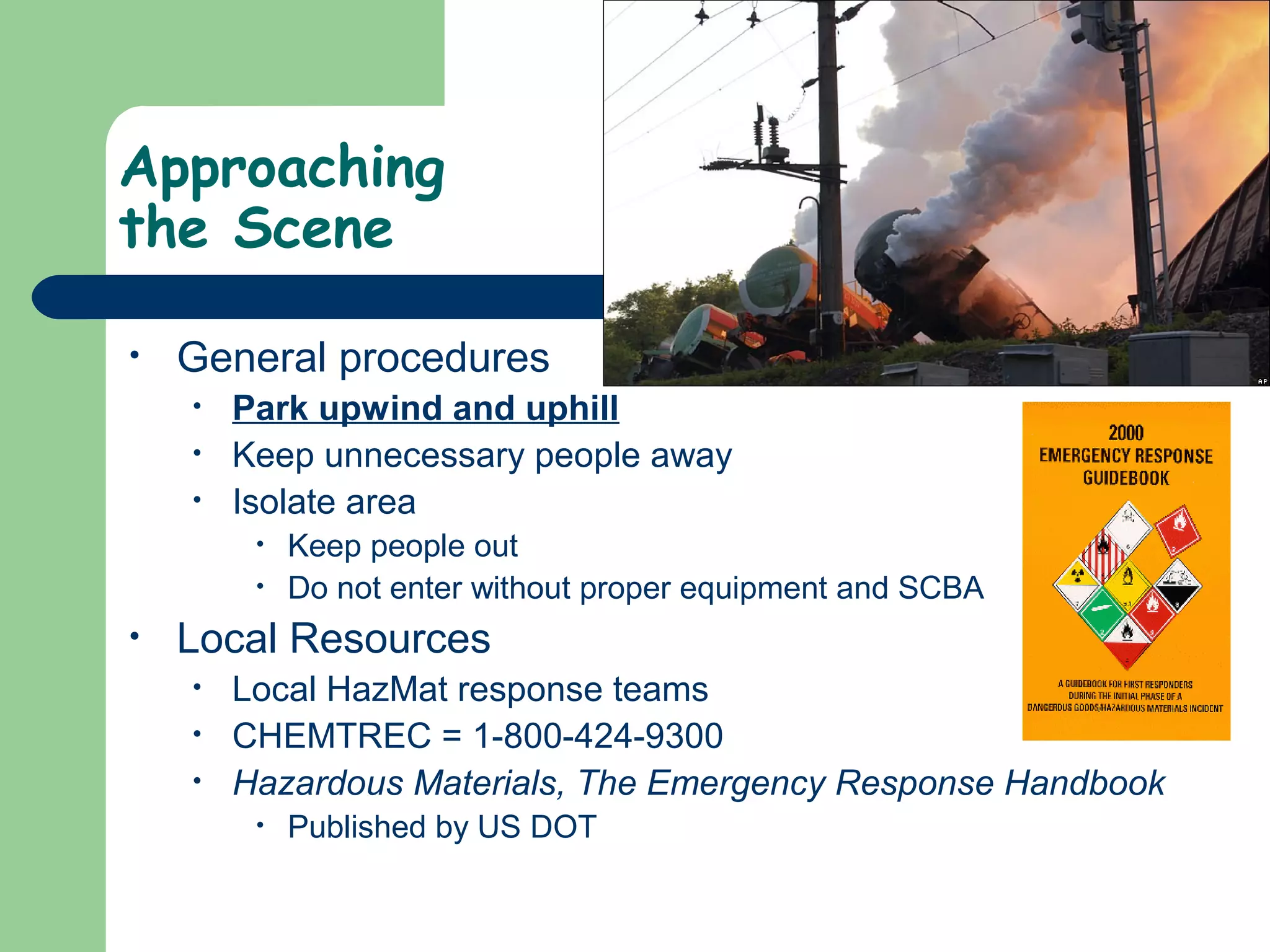
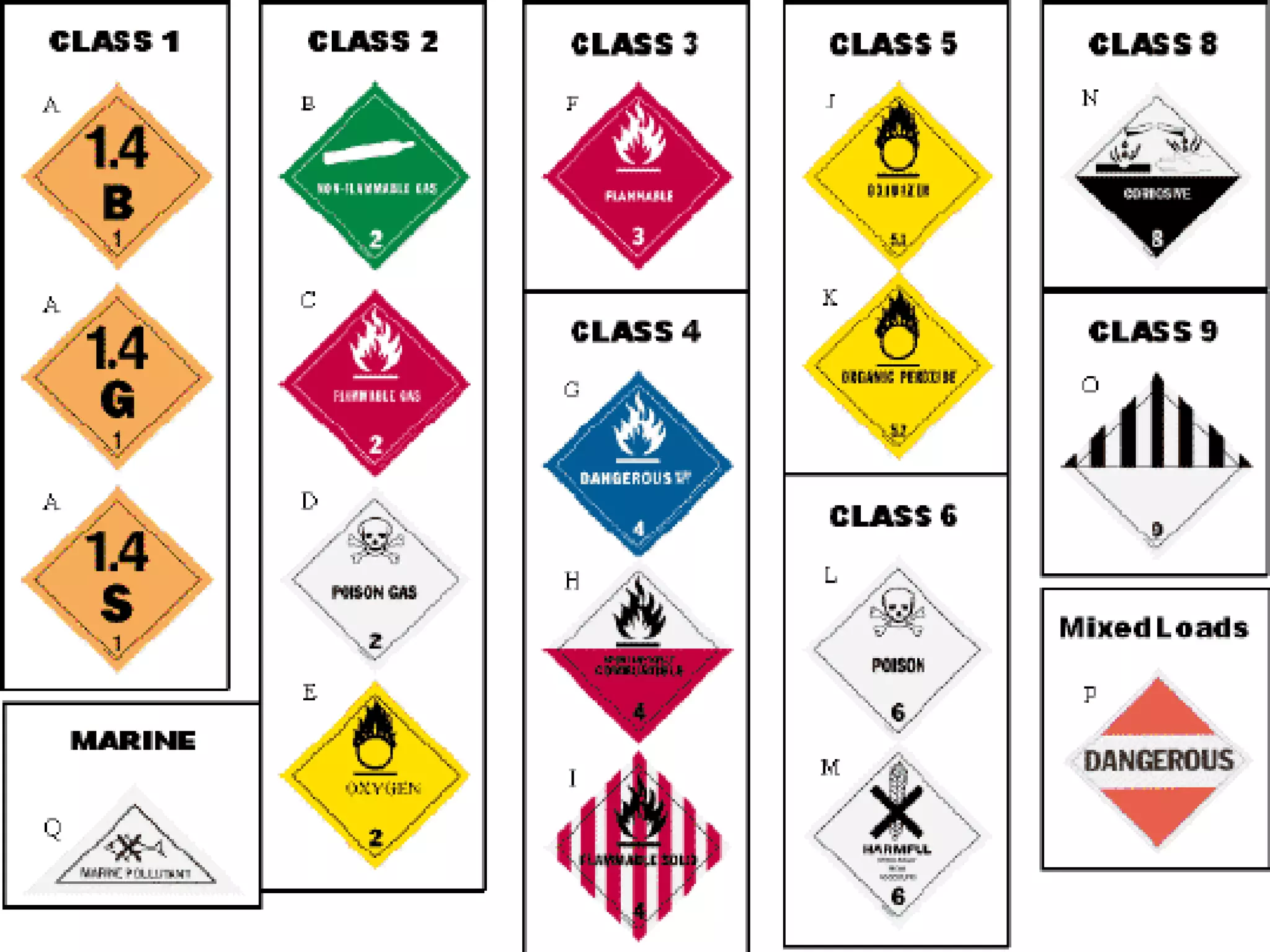
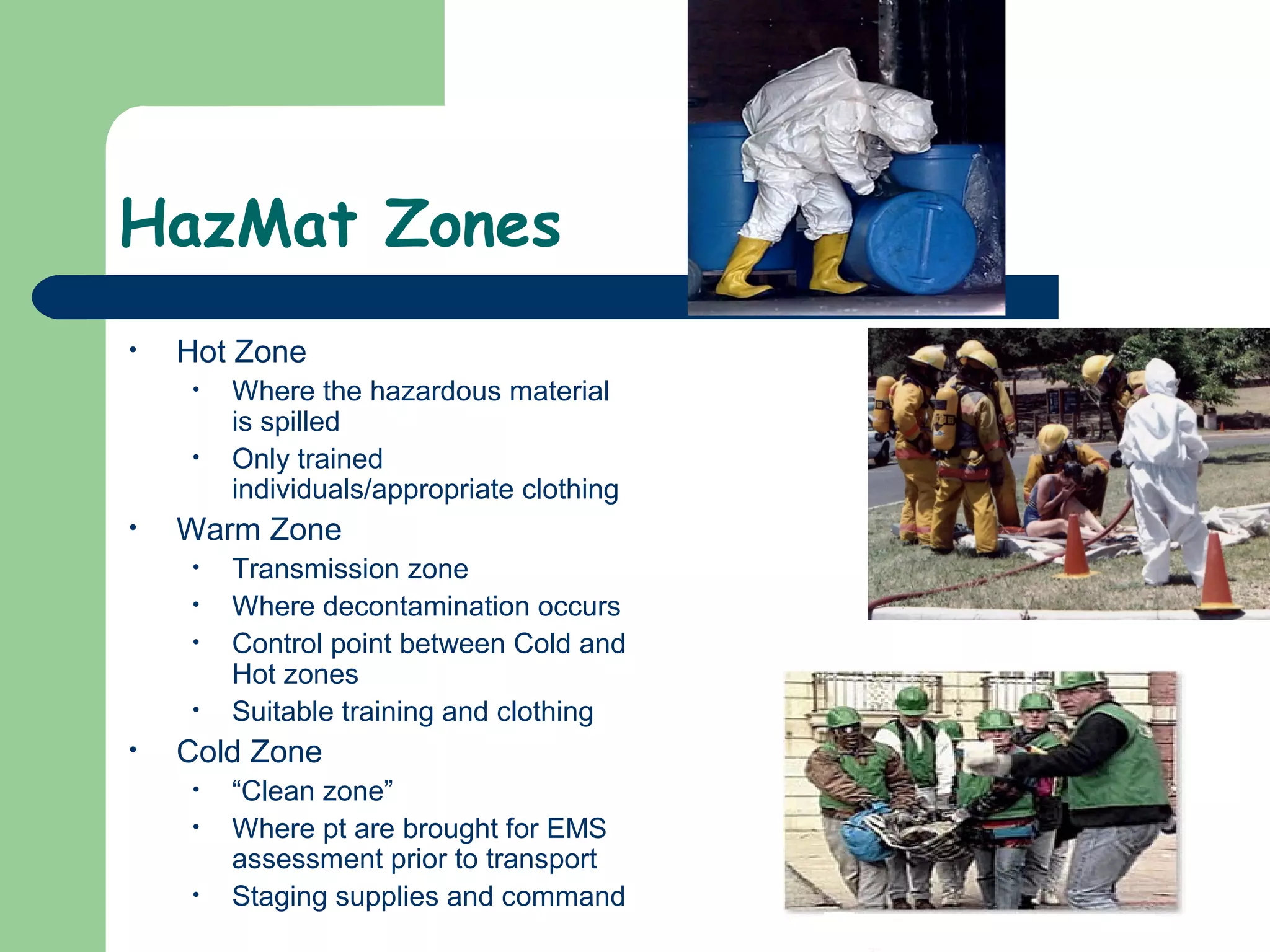
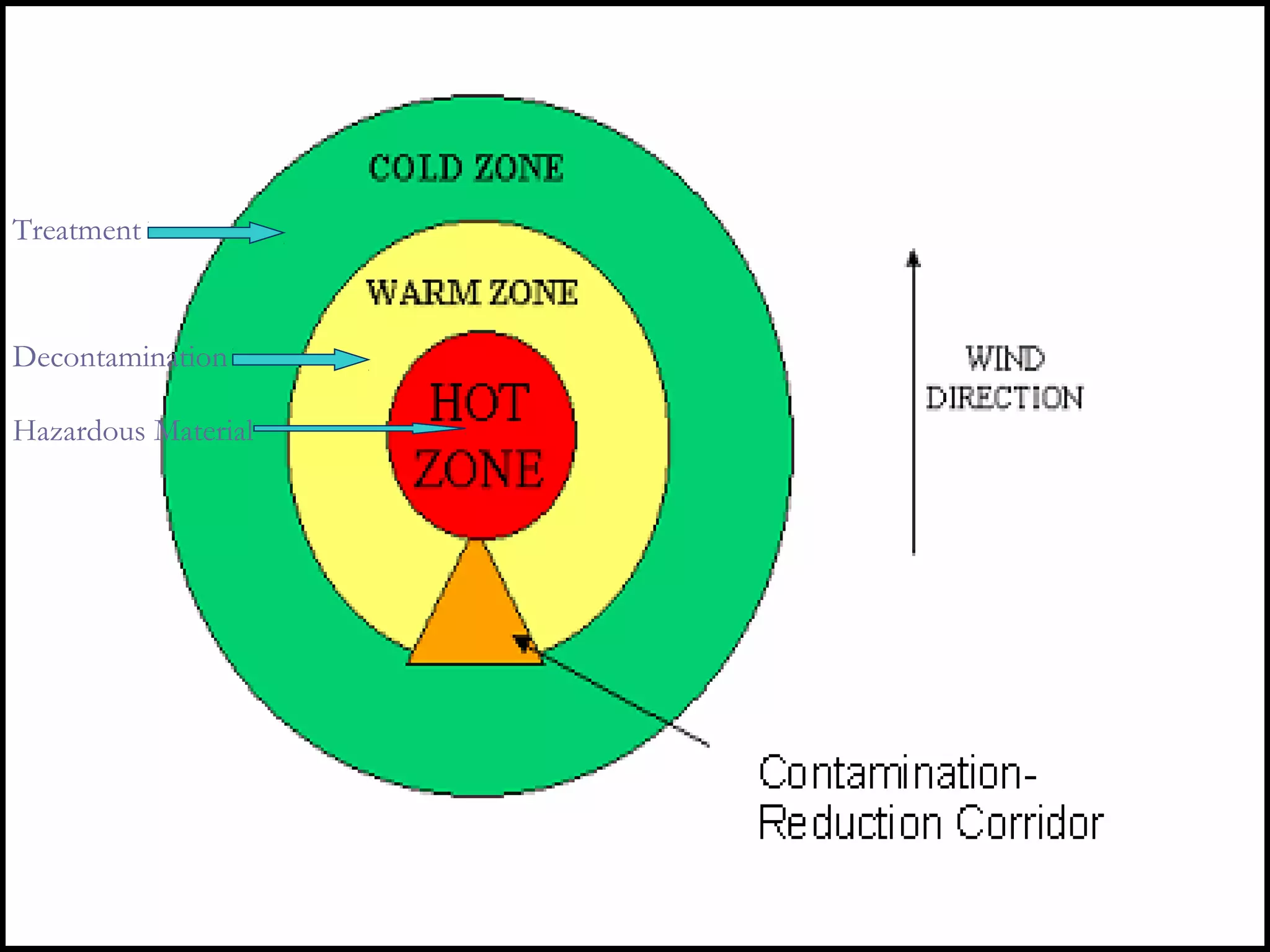
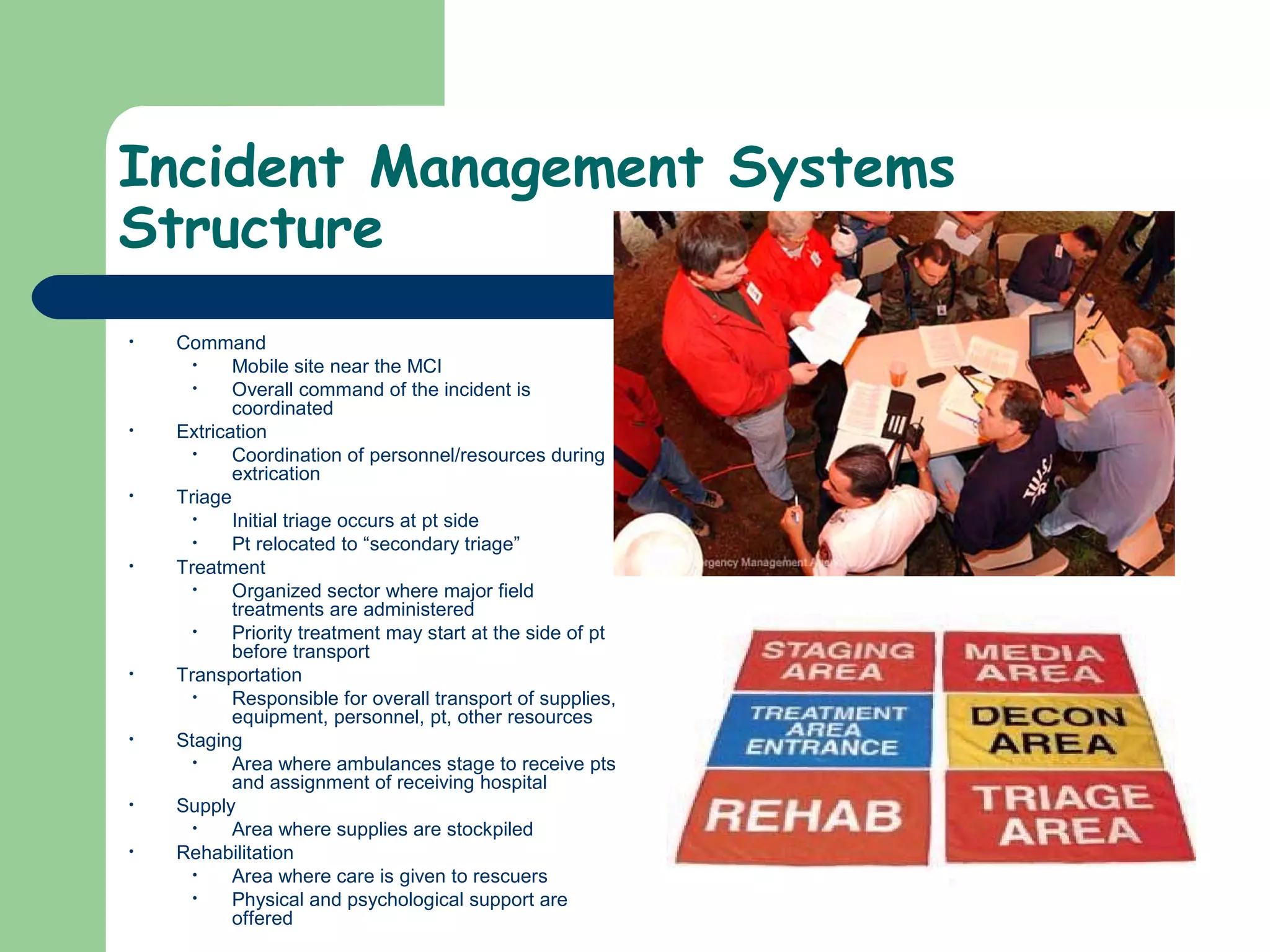
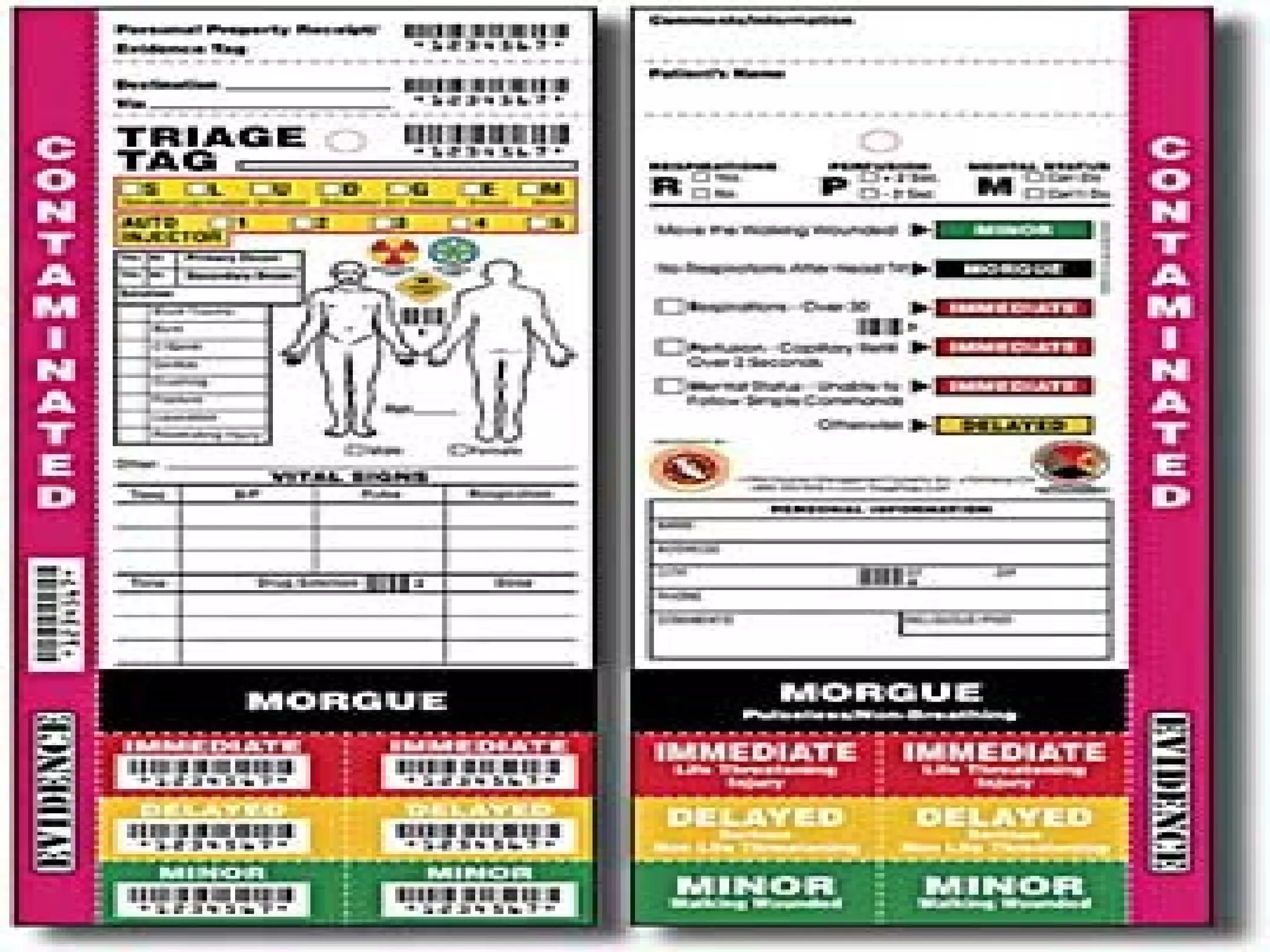
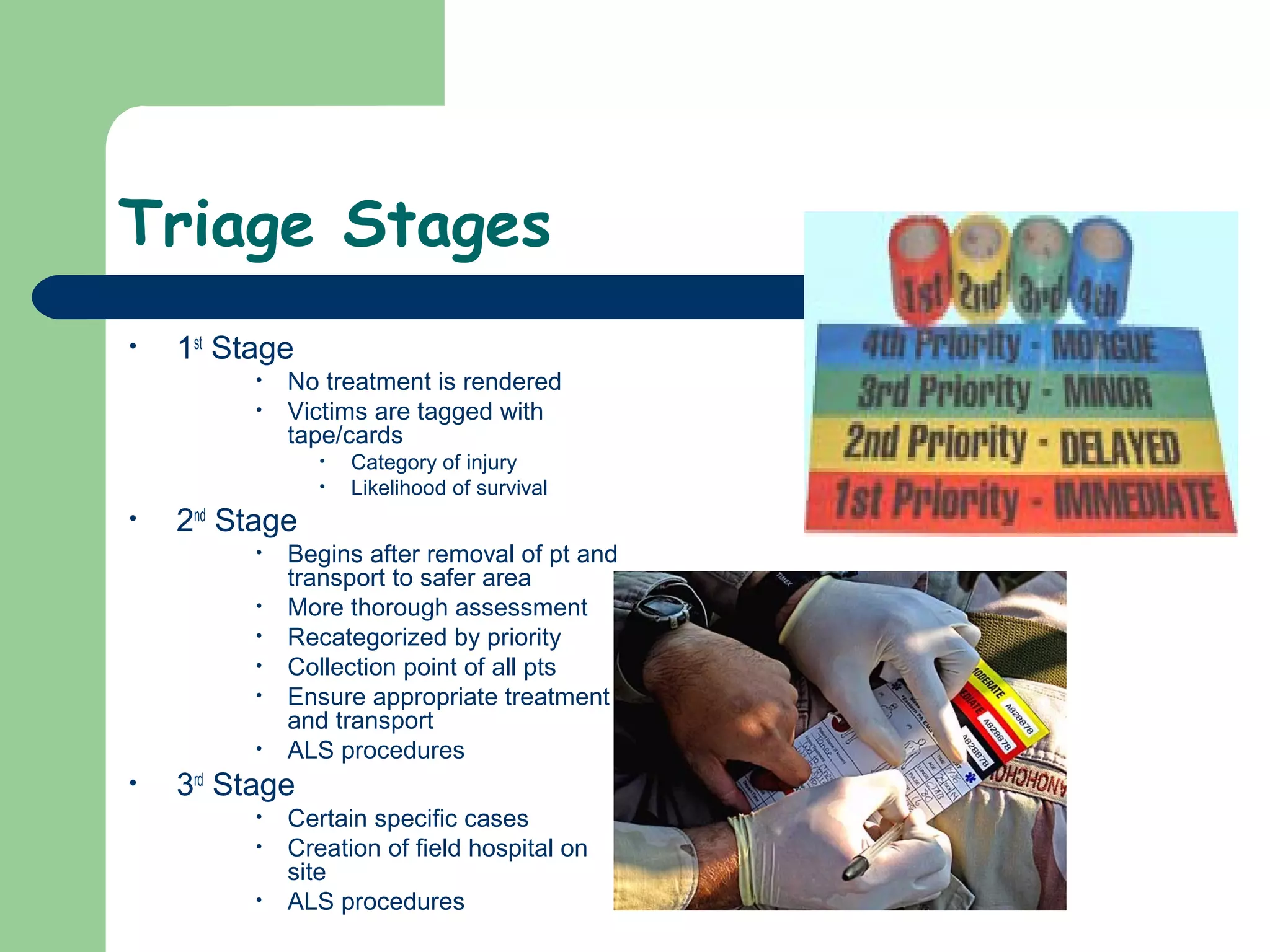
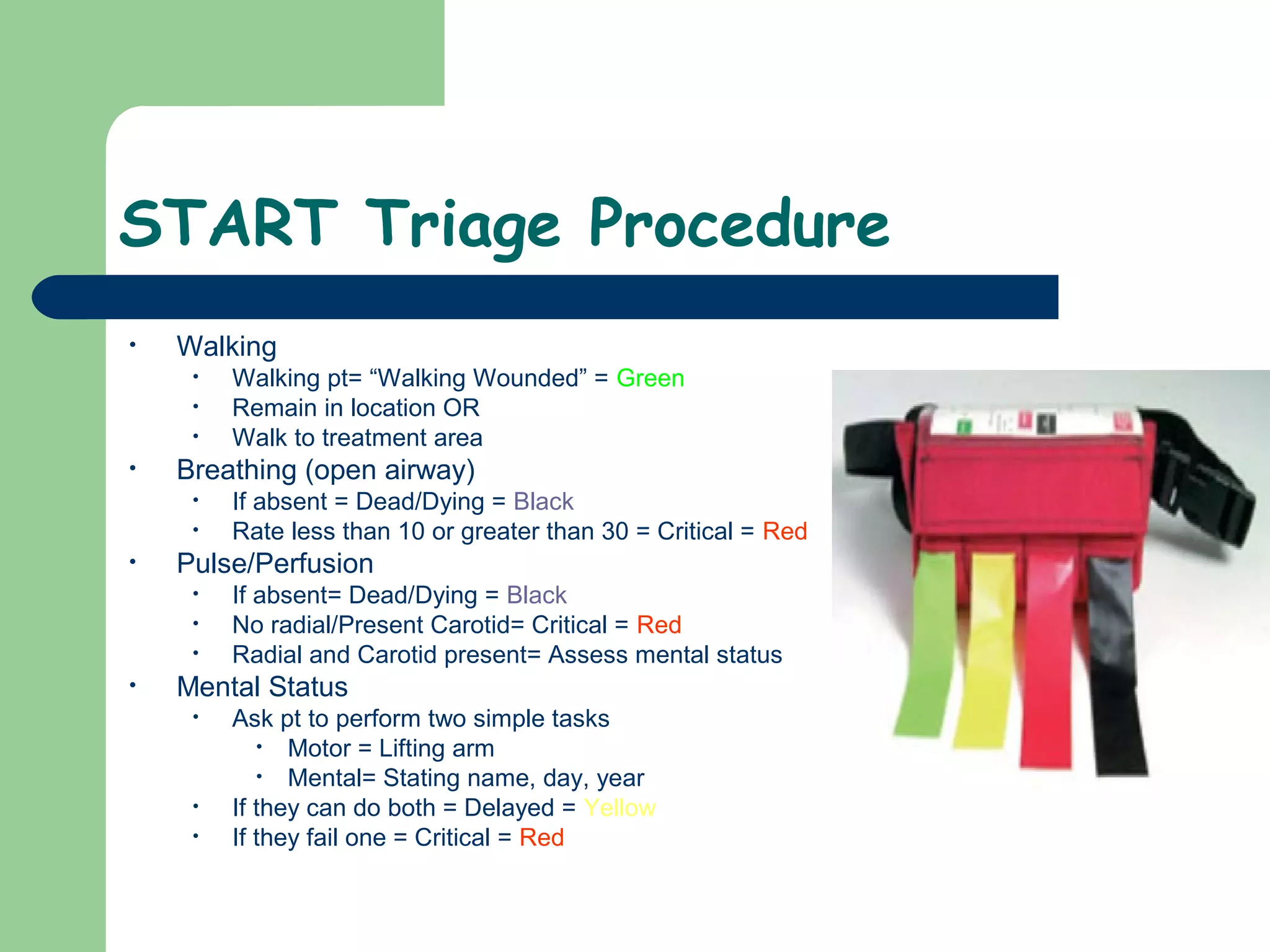
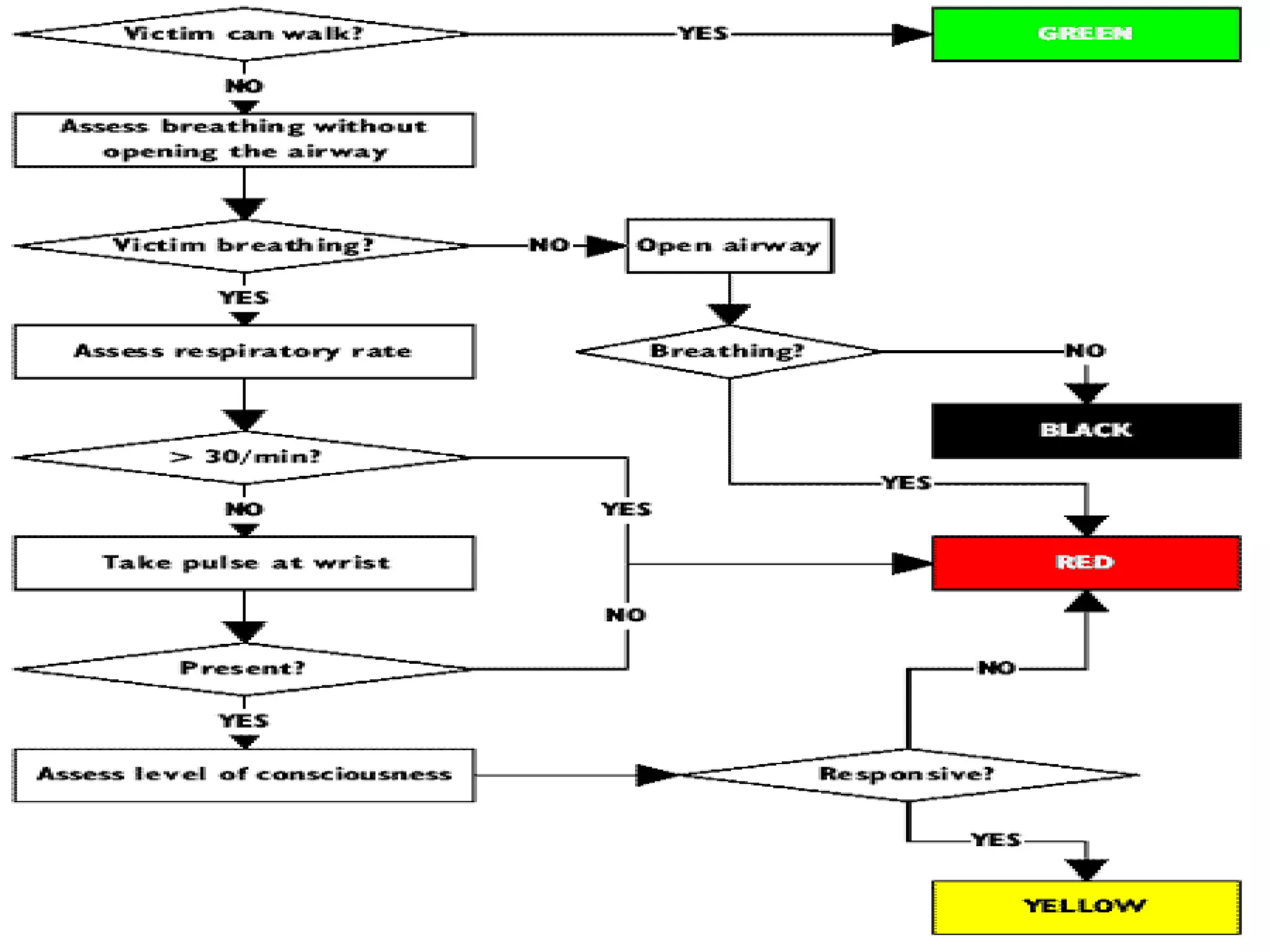
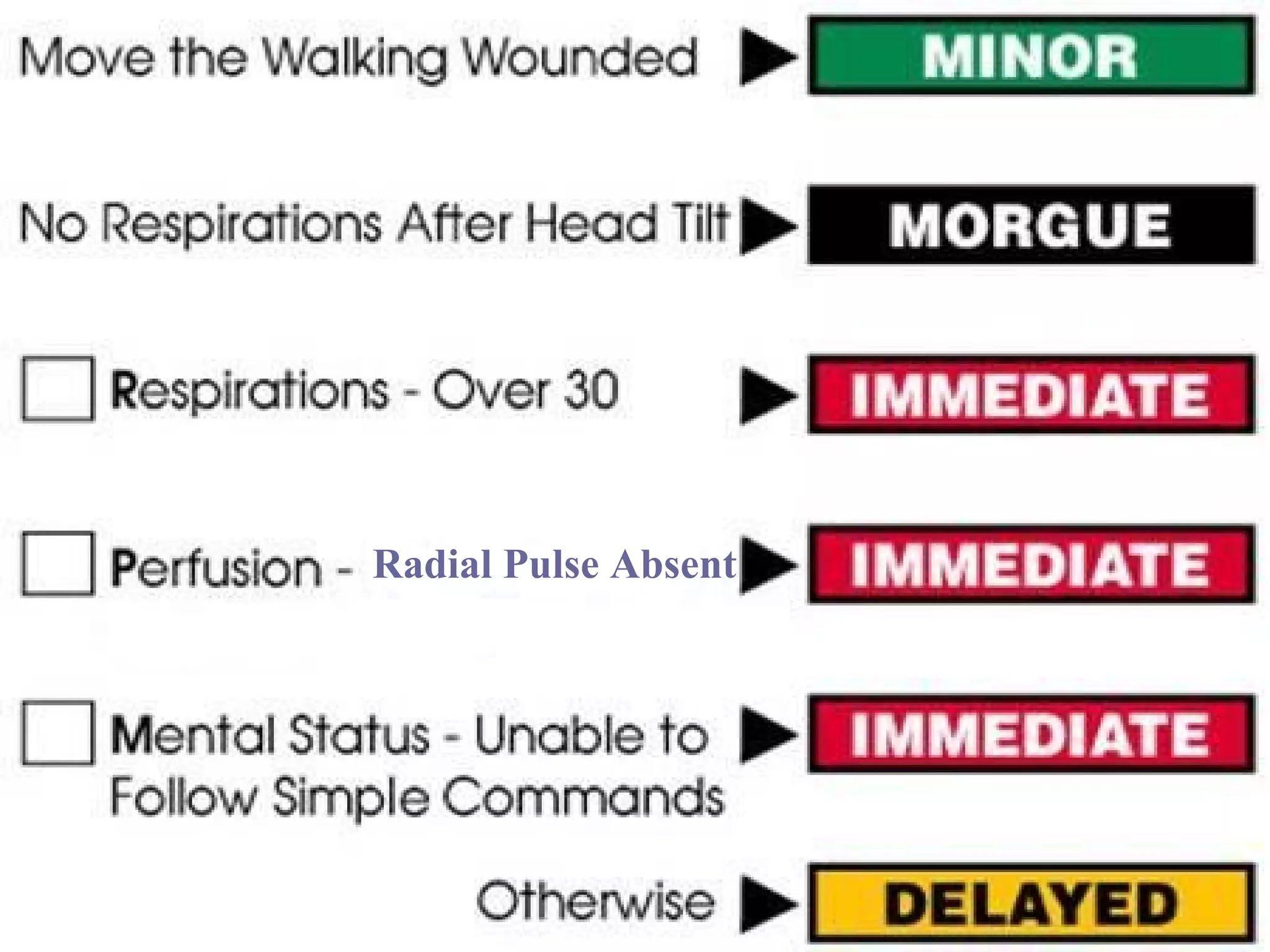
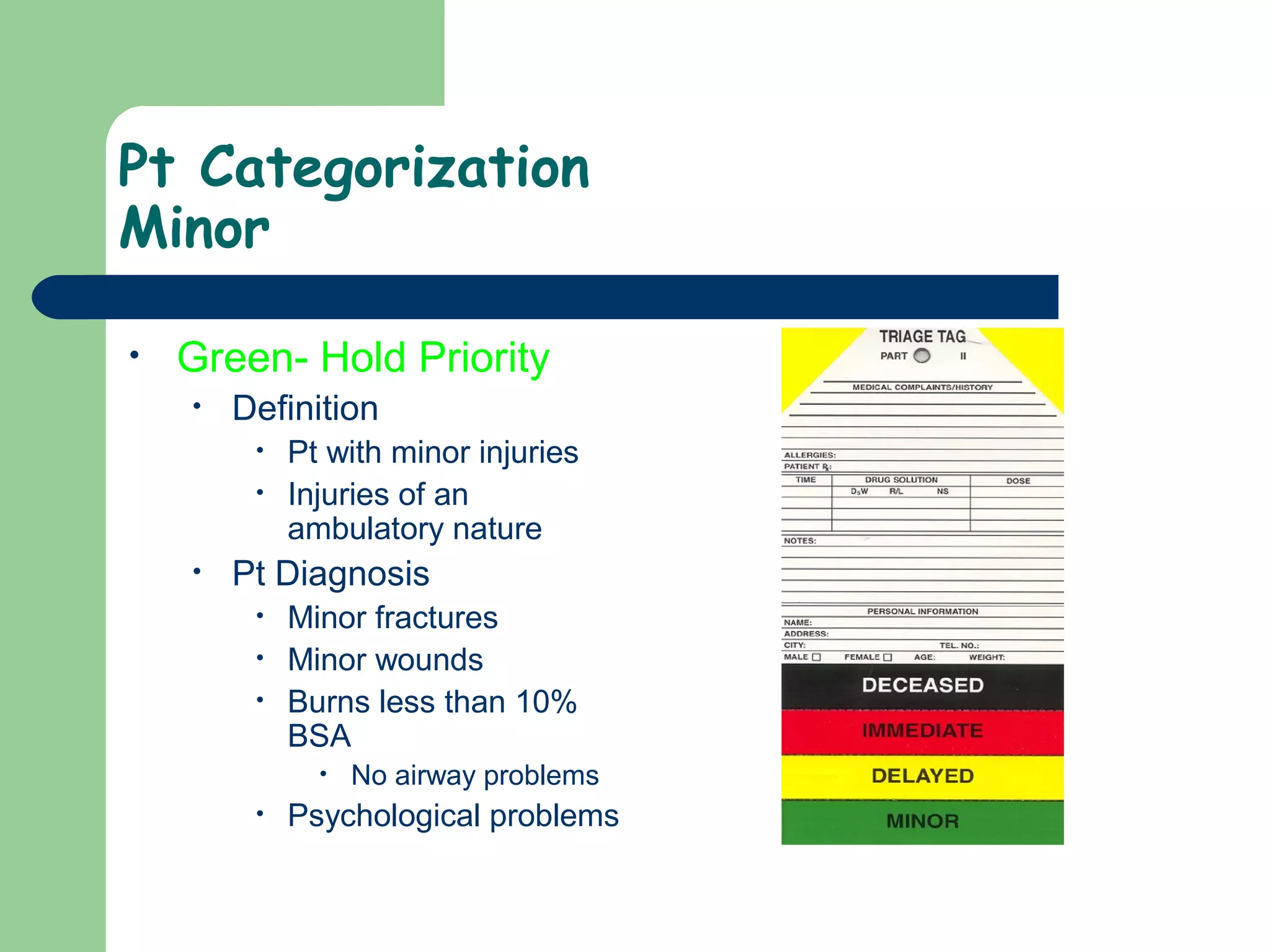
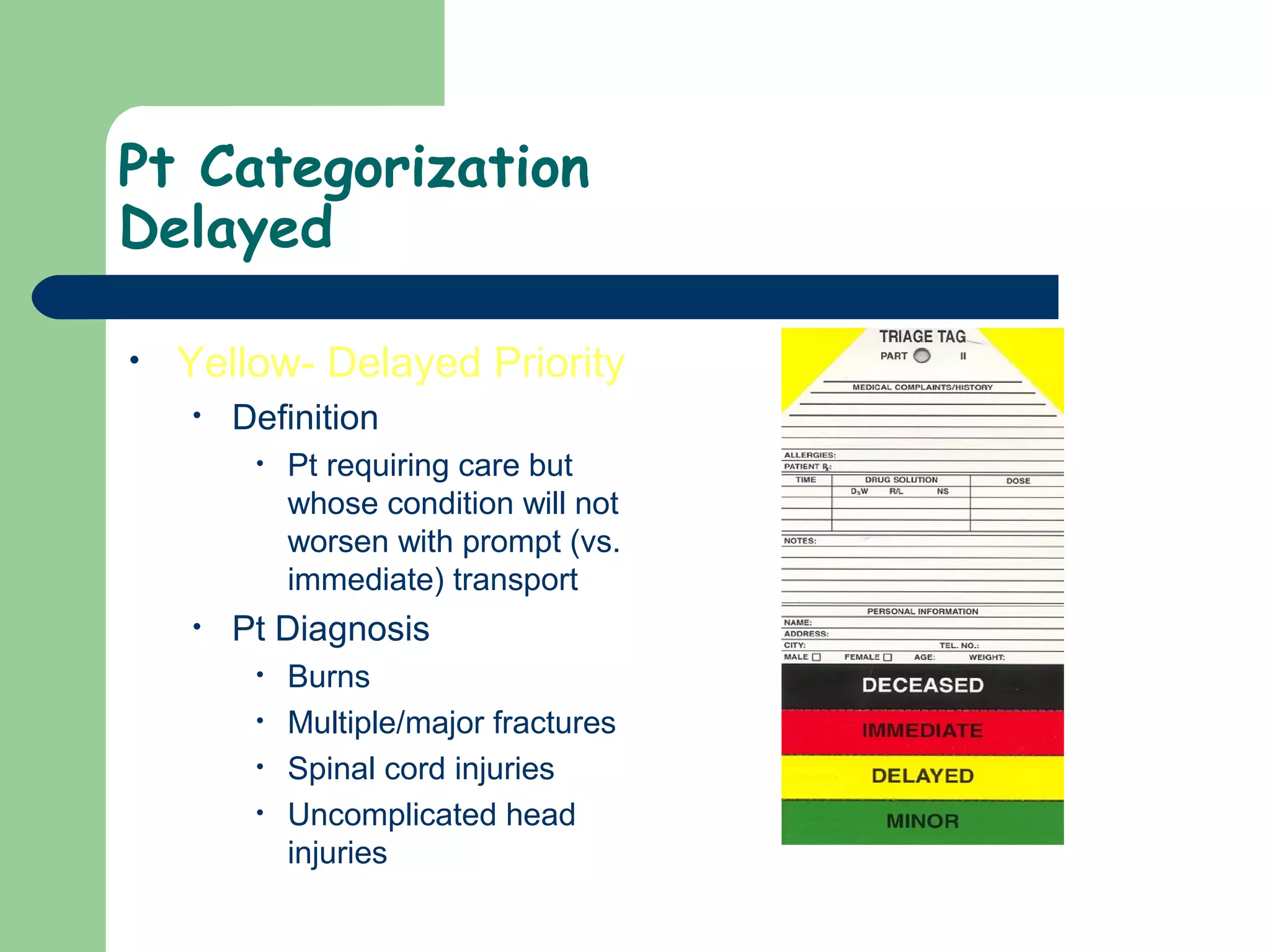
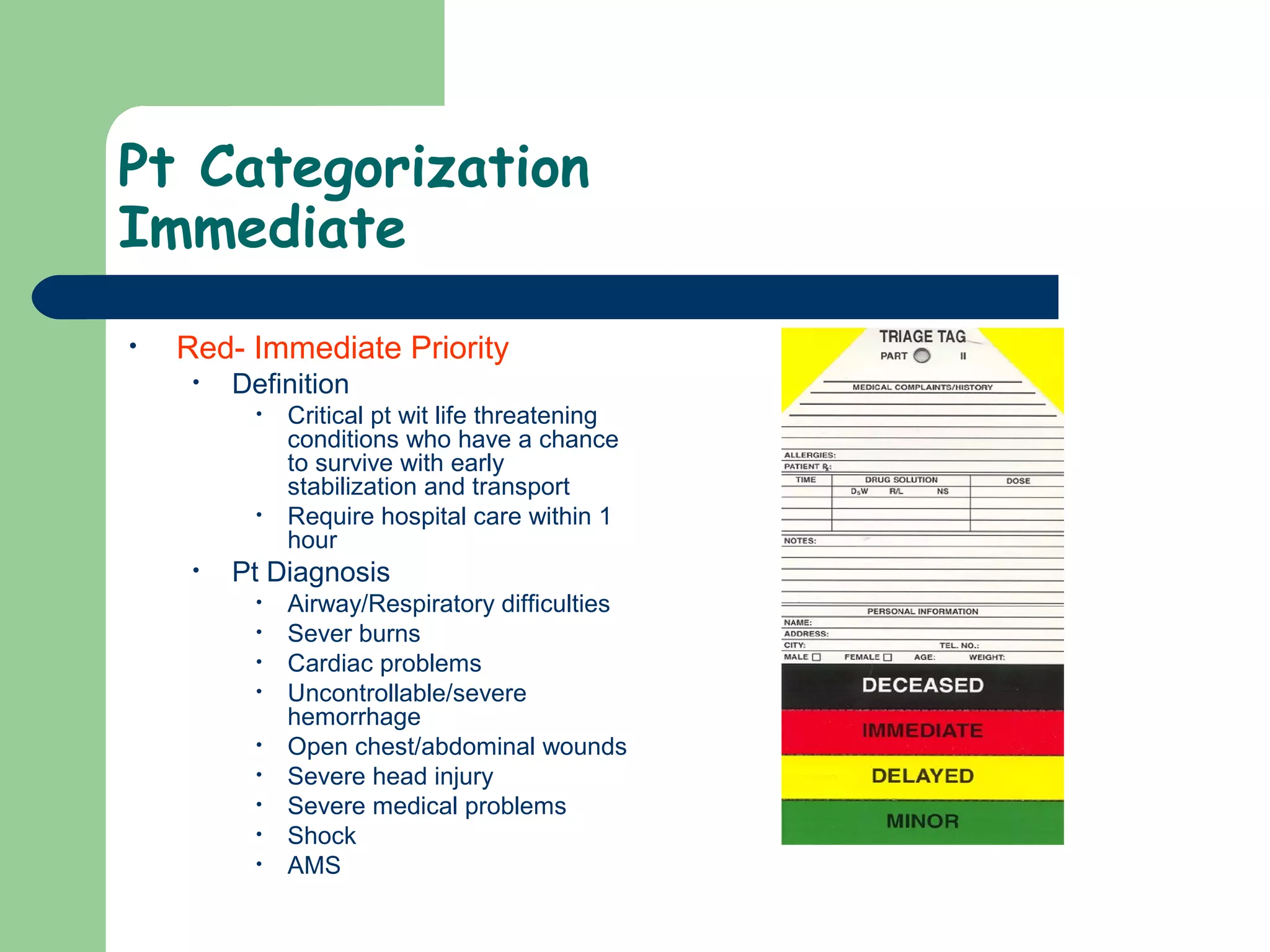
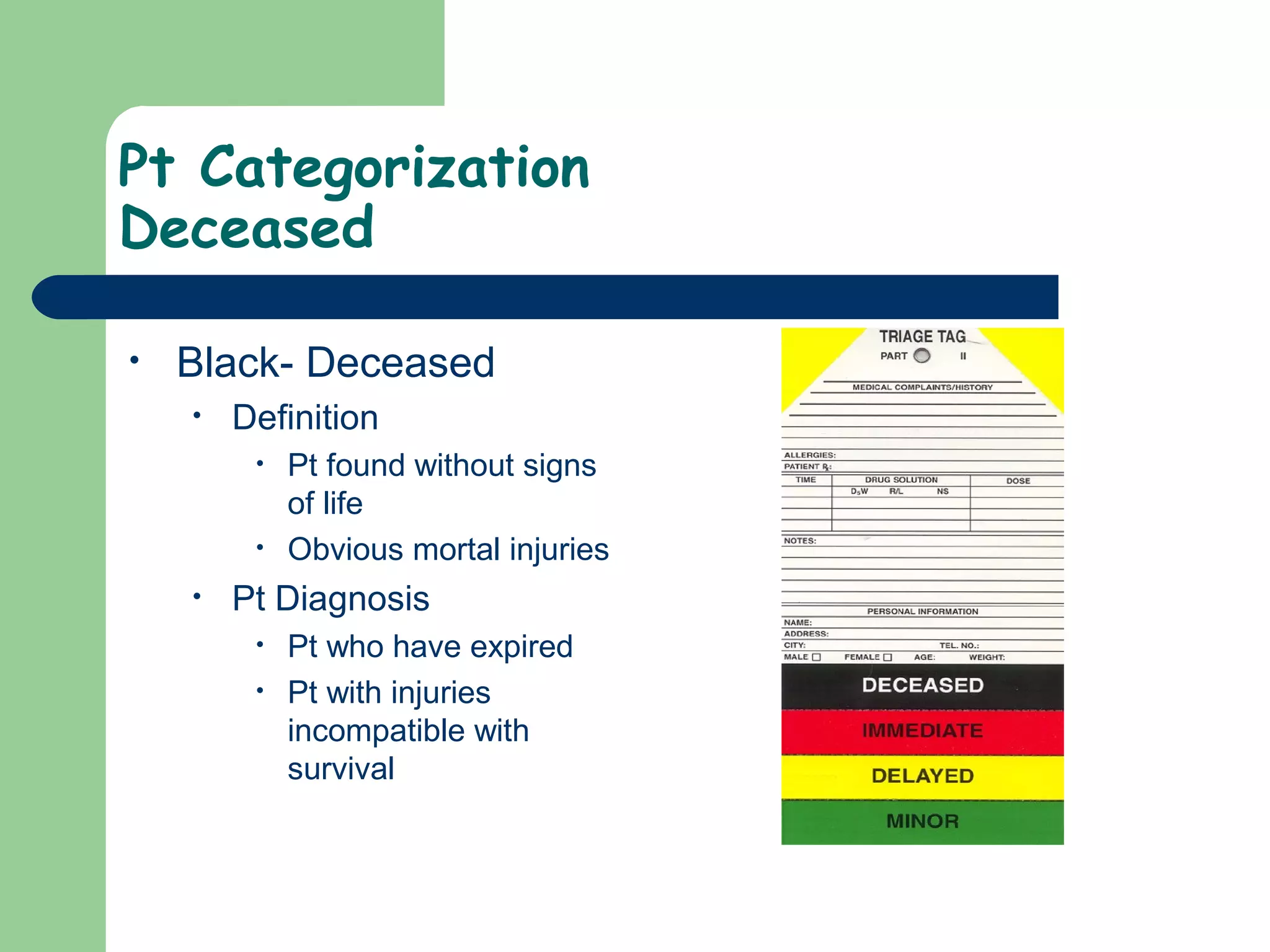
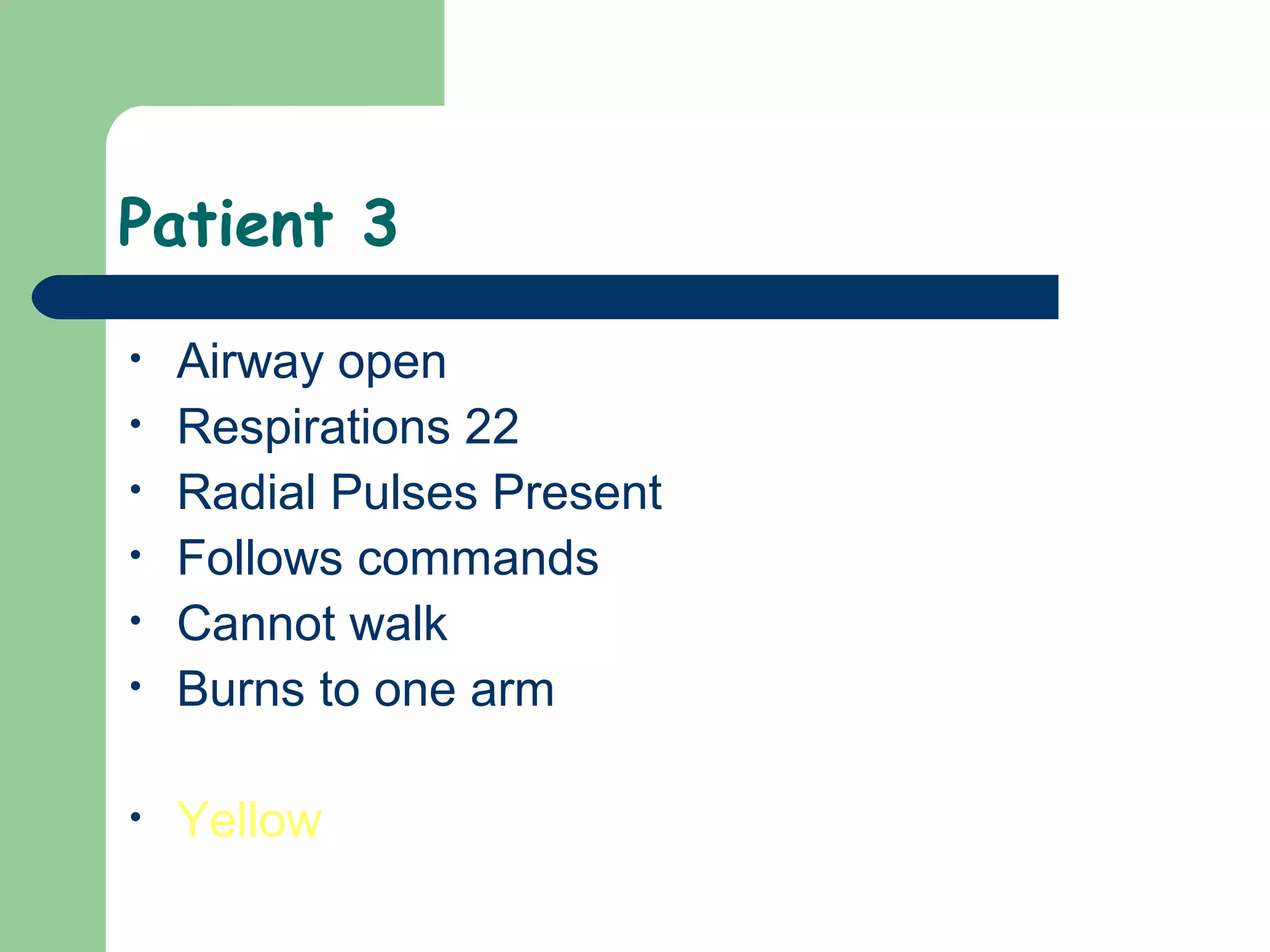
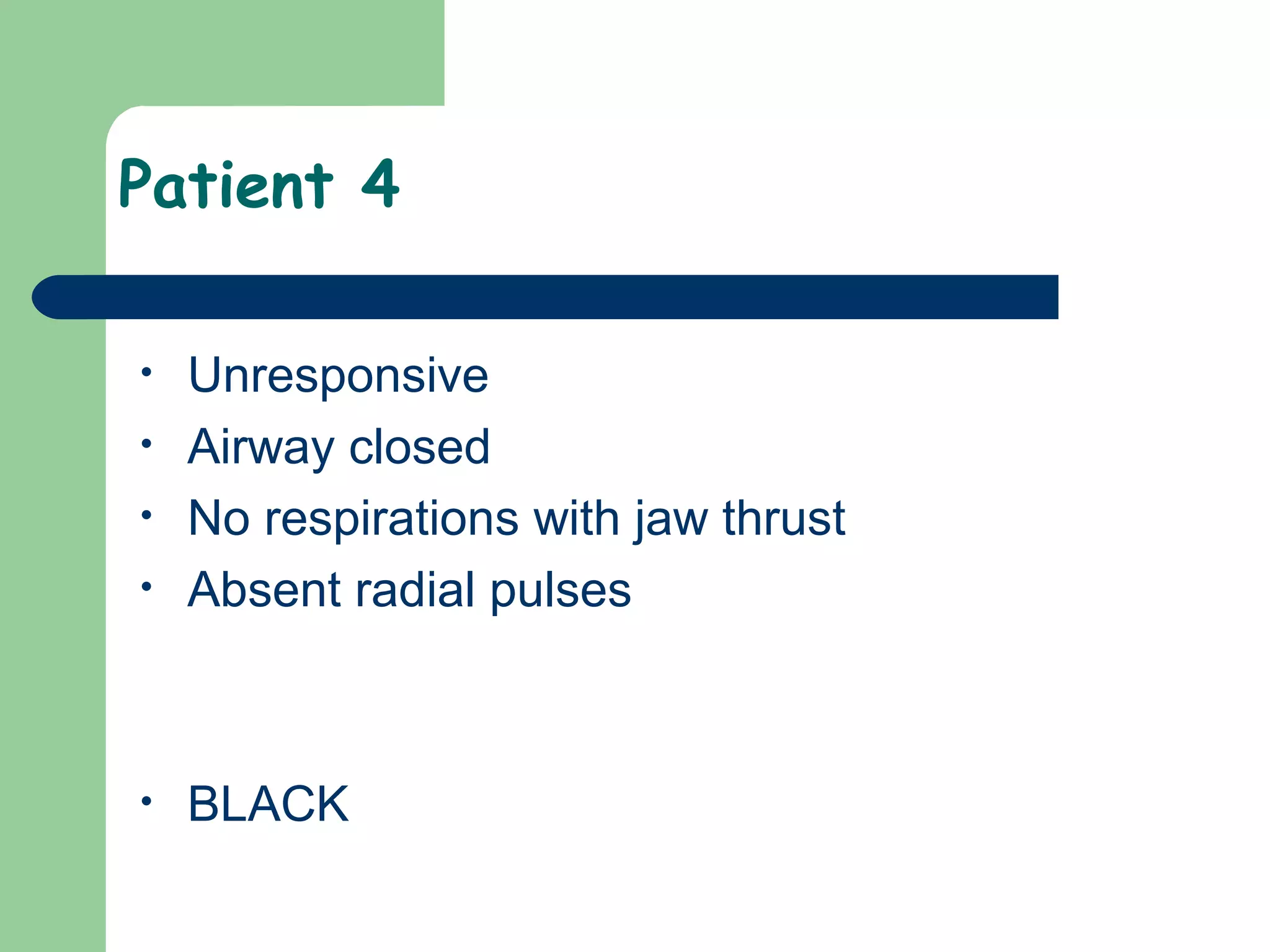
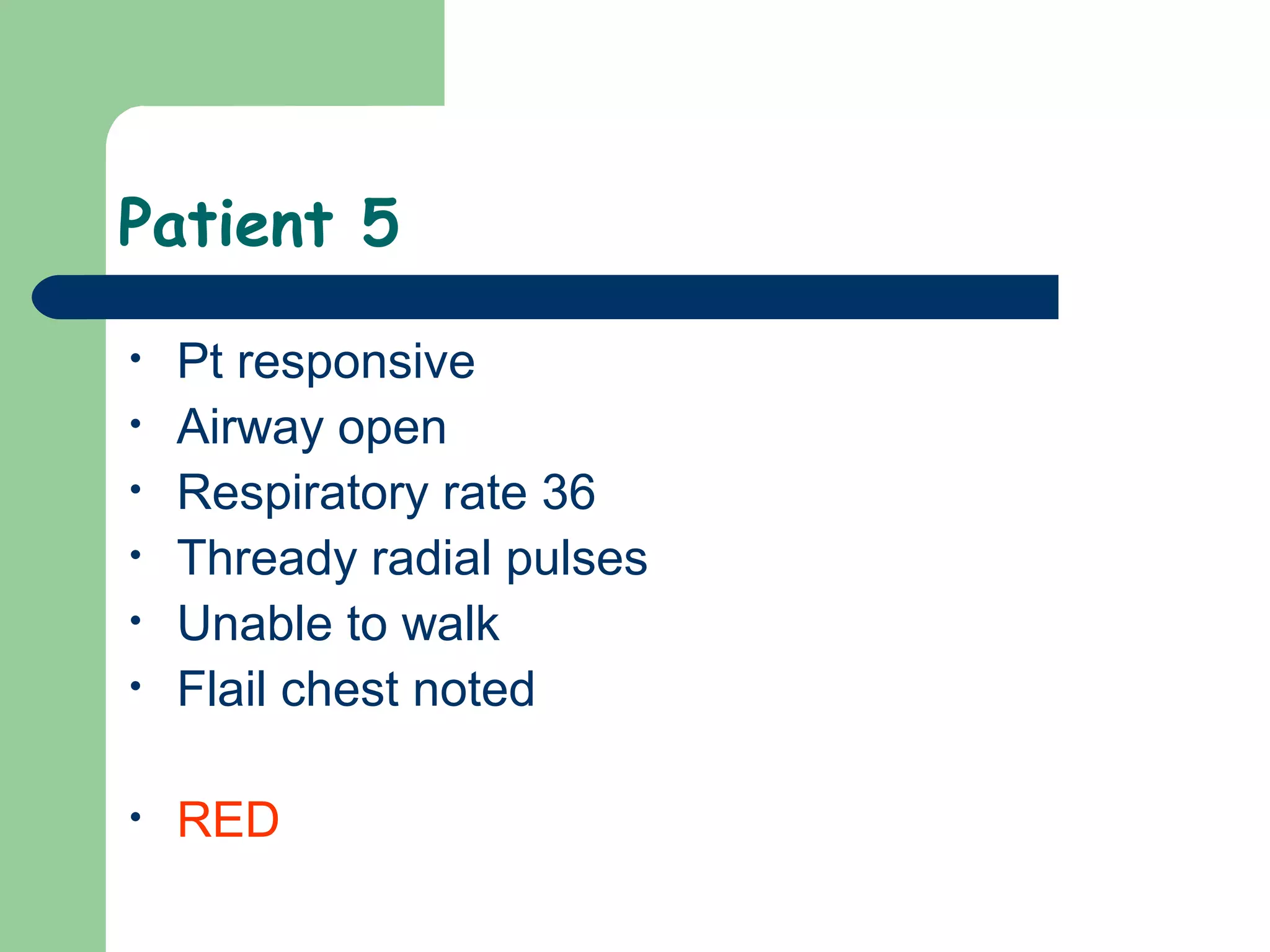
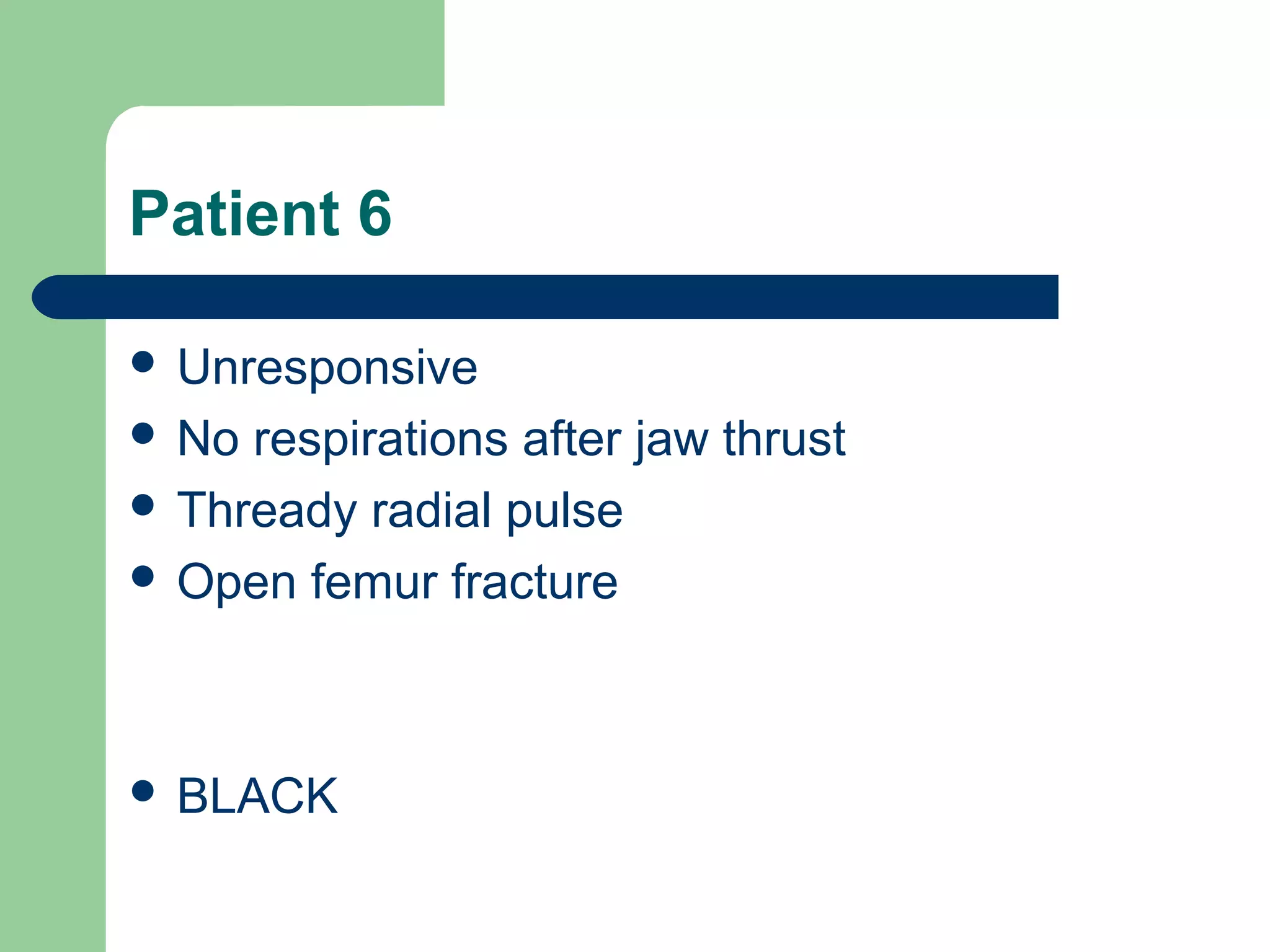
This document provides an overview of hazardous materials (HazMat) incidents and mass casualty incidents (MCI). It describes the types of HazMat, general safety procedures for approaching a HazMat scene, and establishing hazard zones. It also outlines the START triage method and categories for prioritizing patients (green, yellow, red, black). For MCIs, it discusses incident classification and management systems used to coordinate response. The document concludes with descriptions of initial responder roles and procedures for documenting and transporting patients from an MCI.