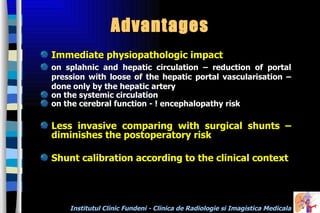
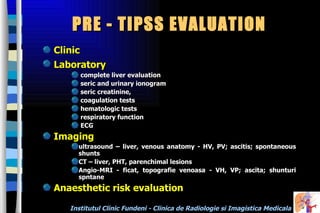
TIPSS is a procedure that creates a permanent connection between the portal and hepatic veins to reduce portal hypertension. It has several indications including uncontrolled variceal bleeding and refractory ascites. The procedure involves catheterization of the jugular vein and placement of a stent. Complications can include thrombosis, hemorrhage, and encephalopathy. Success rates are over 80% for variceal bleeding and 50% for ascites, but secondary dysfunction occurs in 40% after 1 year often requiring revision. TIPSS provides immediate reduction in portal pressure and is less invasive than surgical shunting.