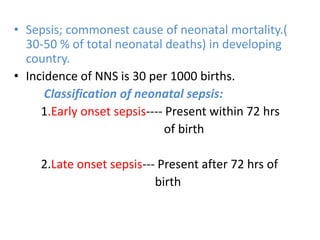
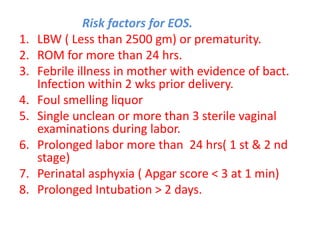
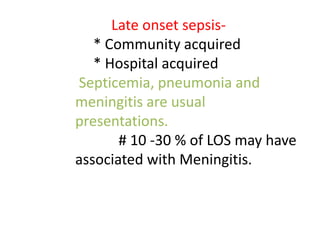
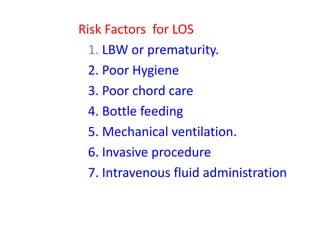
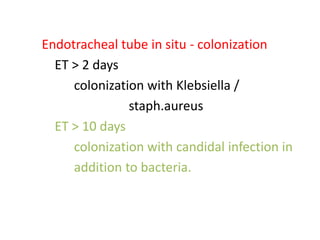
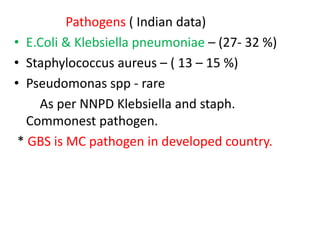
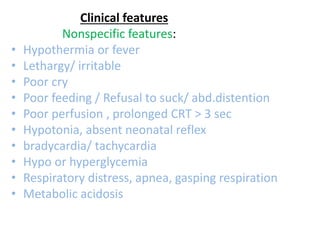
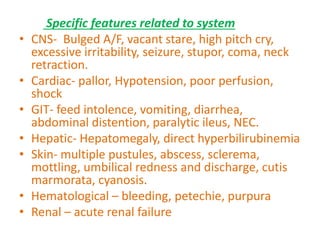
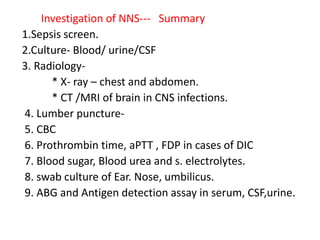
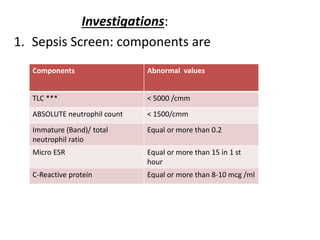
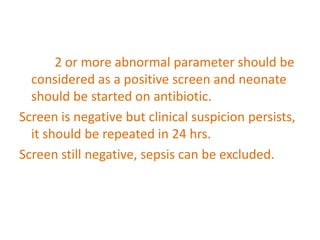
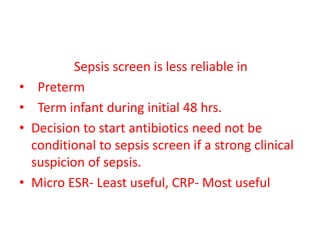
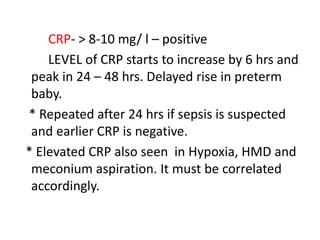
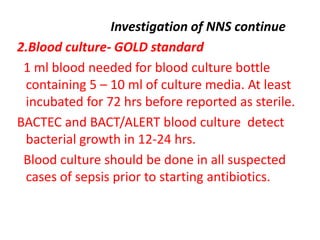
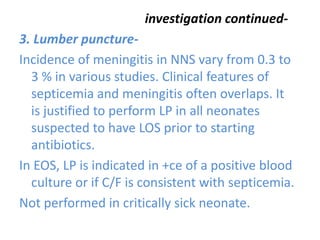
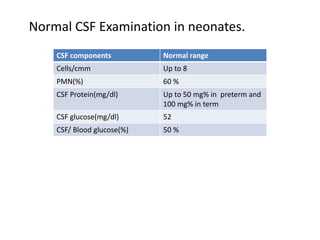
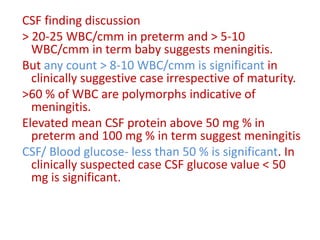
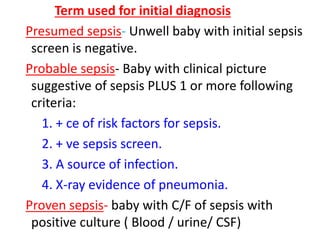
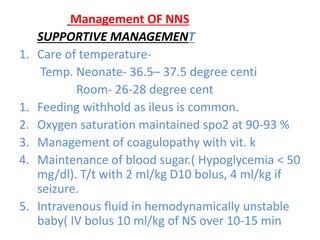
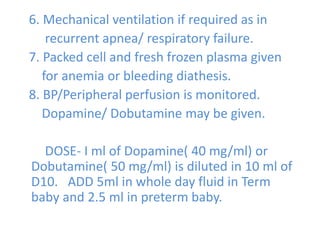
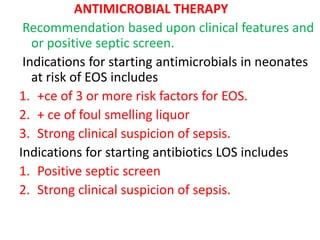
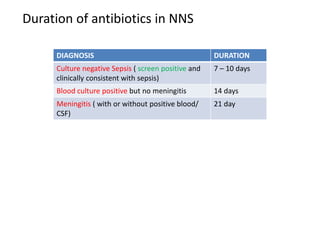
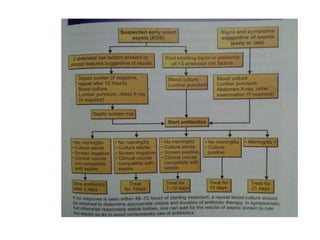
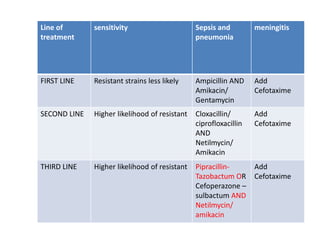
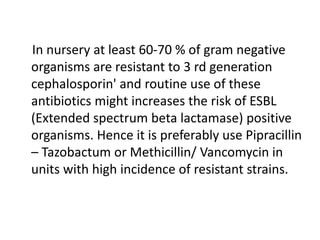
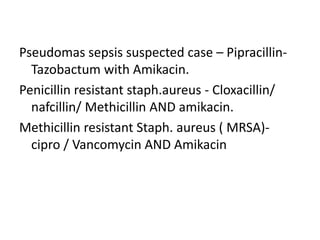
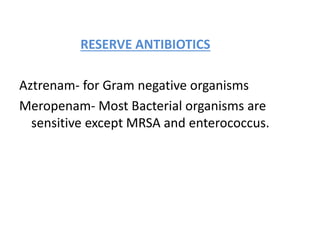
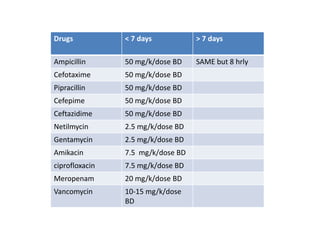
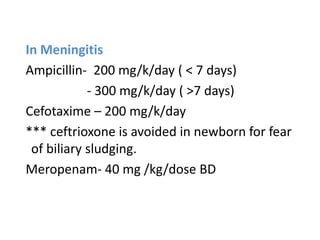
Neonatal sepsis is a clinical syndrome characterized by signs and symptoms of infection in the first month of life. It can involve sepsis, meningitis, pneumonia and other infections. The document discusses the definition, classification, risk factors, clinical features, investigations and management of neonatal sepsis. Key points include that sepsis is a leading cause of neonatal mortality, the importance of sepsis screening and blood cultures, and that initial empirical antibiotic therapy typically involves ampicillin and an aminoglycoside.