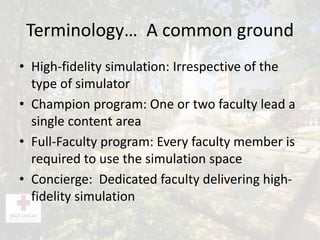
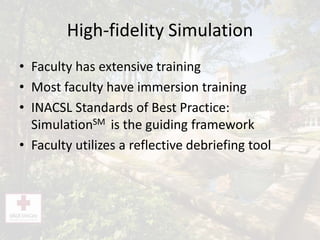
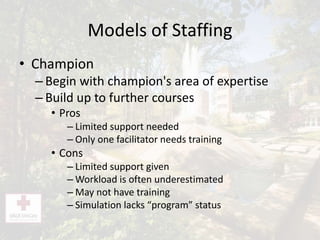
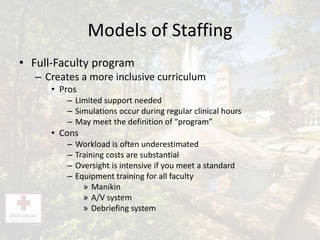
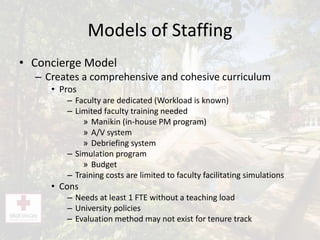
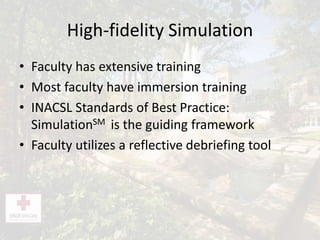
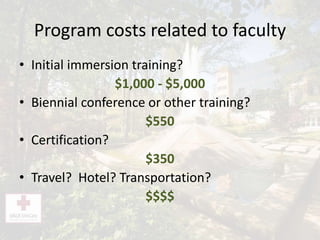
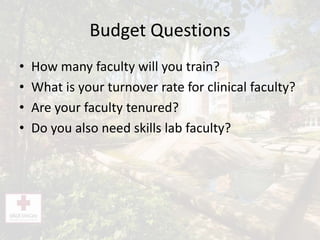
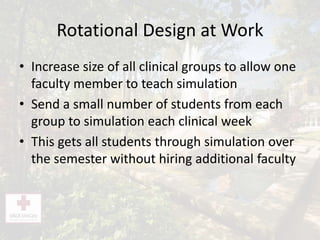
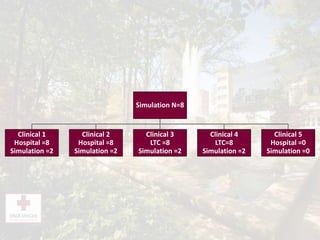
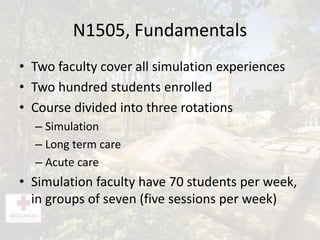
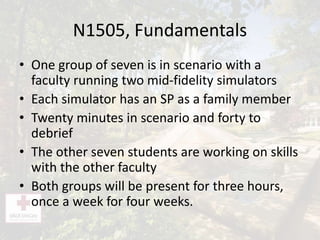
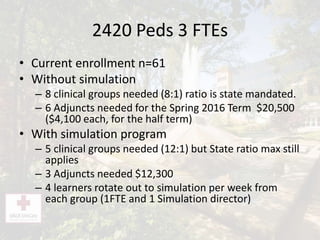
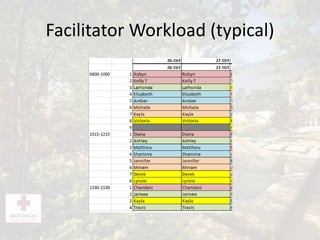
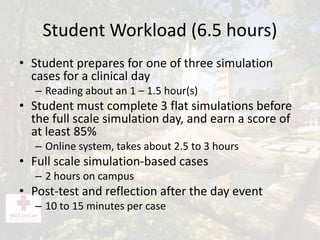
This document discusses different models for integrating simulation-based learning experiences across nursing school curricula. It describes the champion, full-faculty, and concierge models and compares their pros and cons. The concierge model, where dedicated faculty deliver simulations, allows for a more comprehensive curriculum while limiting training costs compared to the full-faculty model. The document also provides examples of how a rotational design can be used to schedule students for simulations without increasing faculty needs. This design increases clinical group sizes so that small numbers of students from each group attend simulations each week.