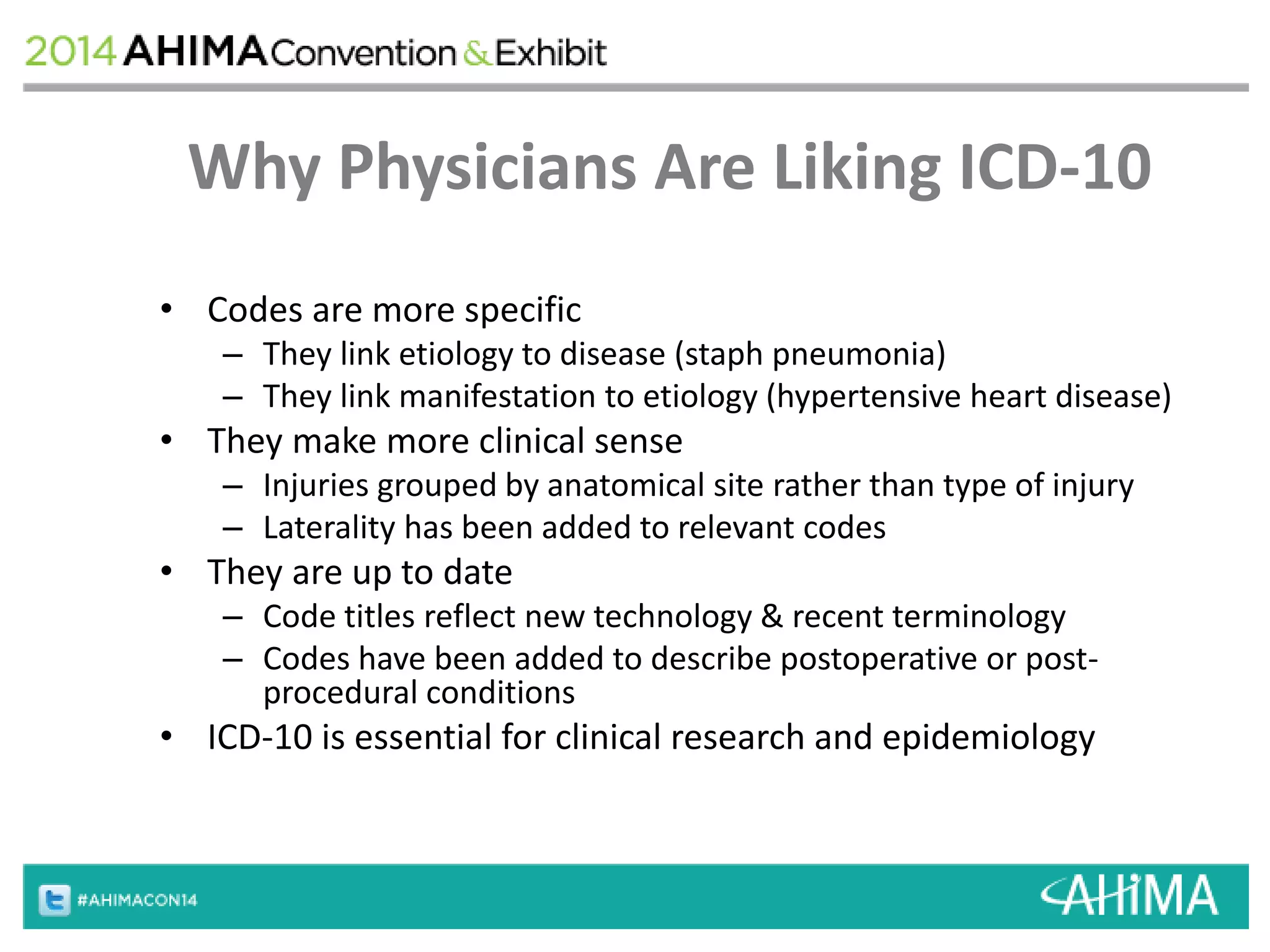
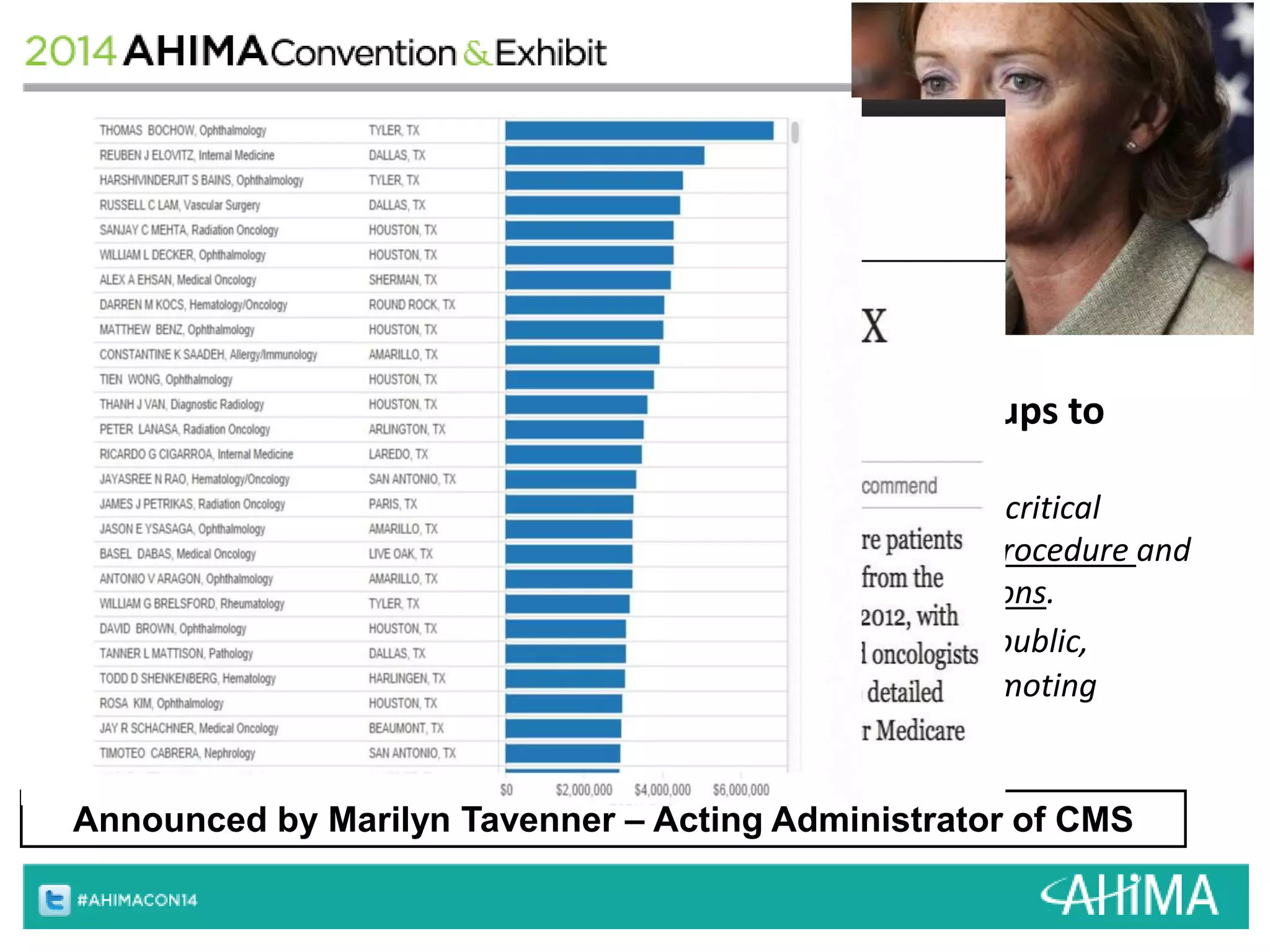
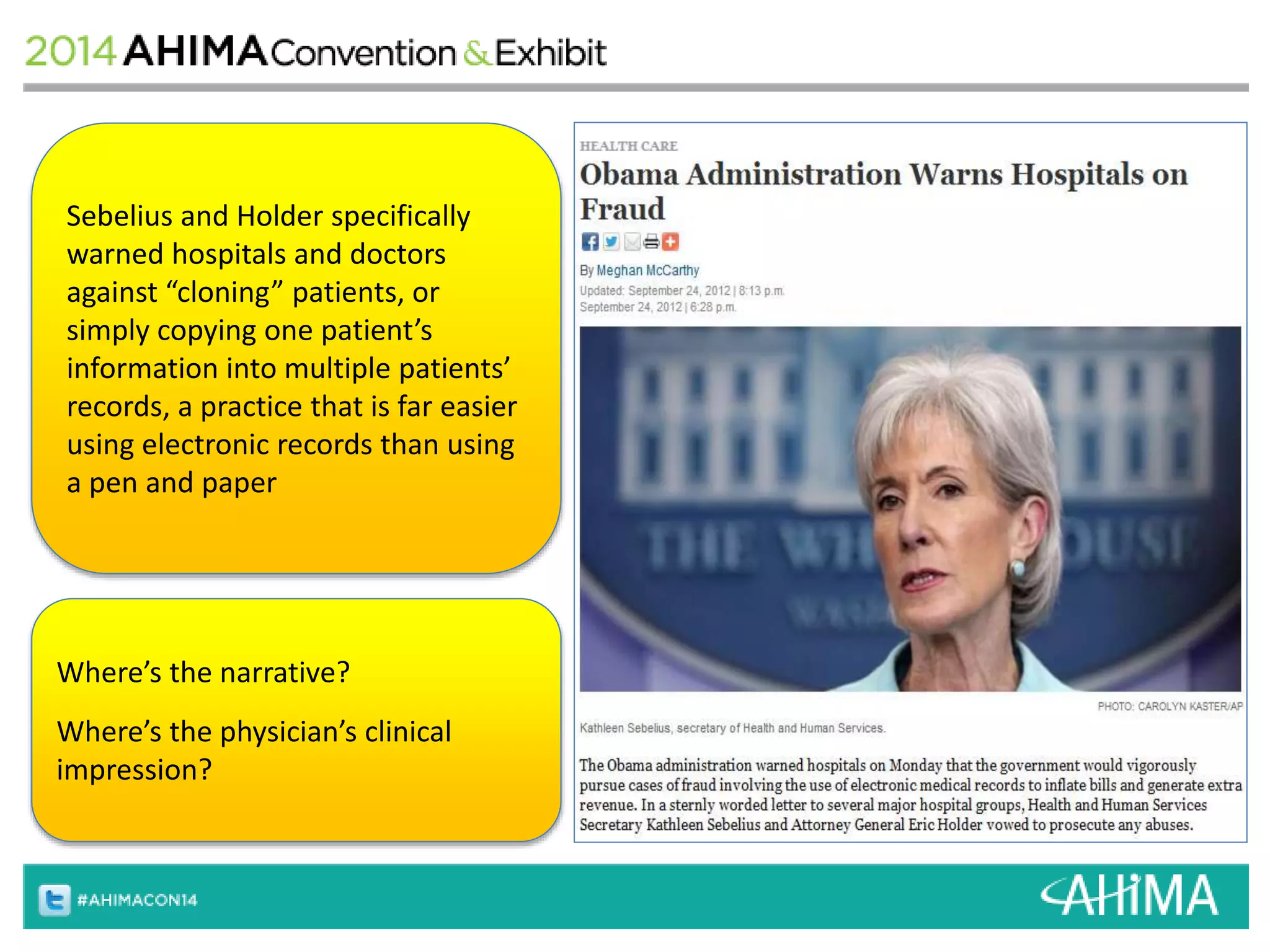
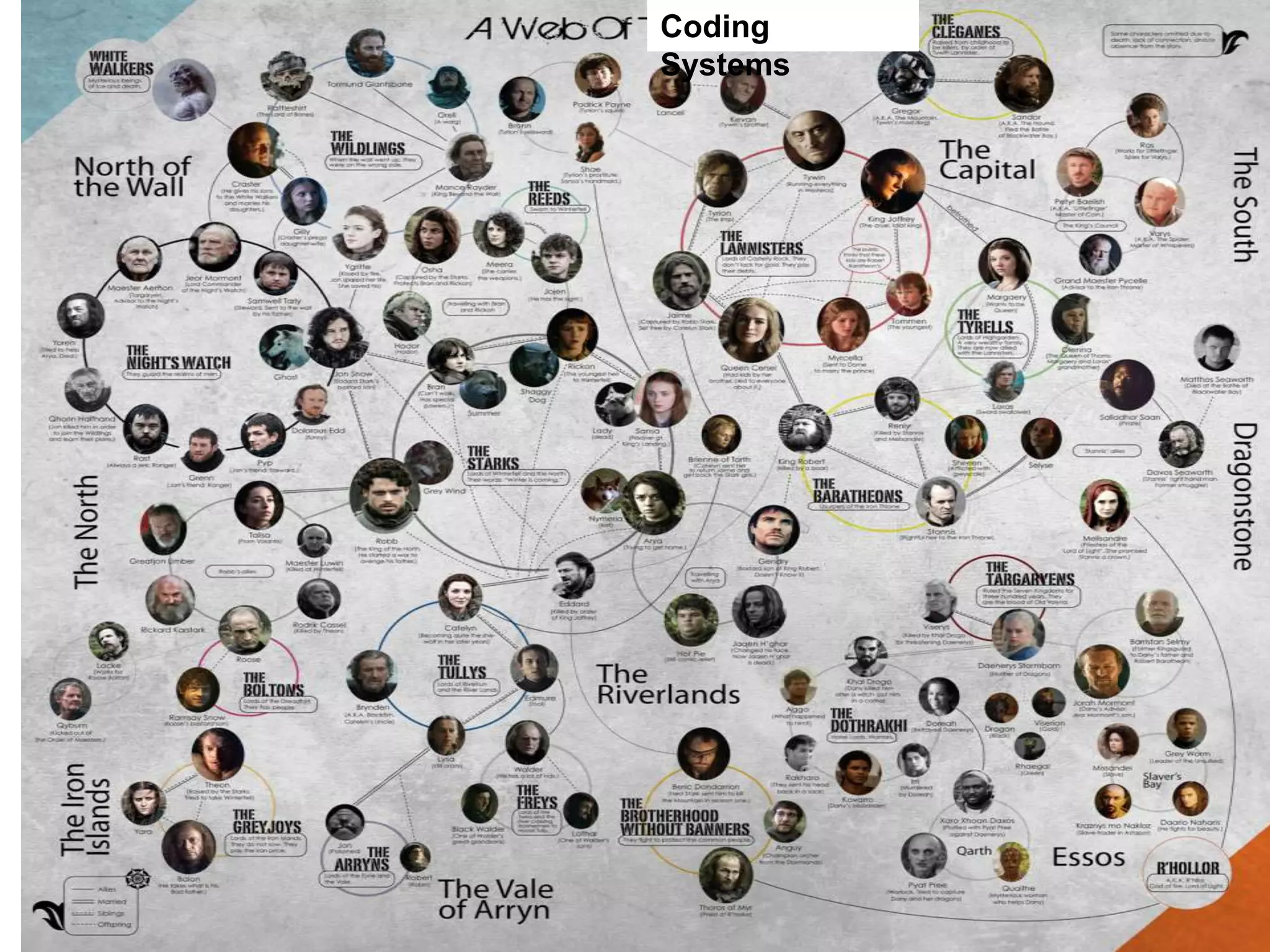
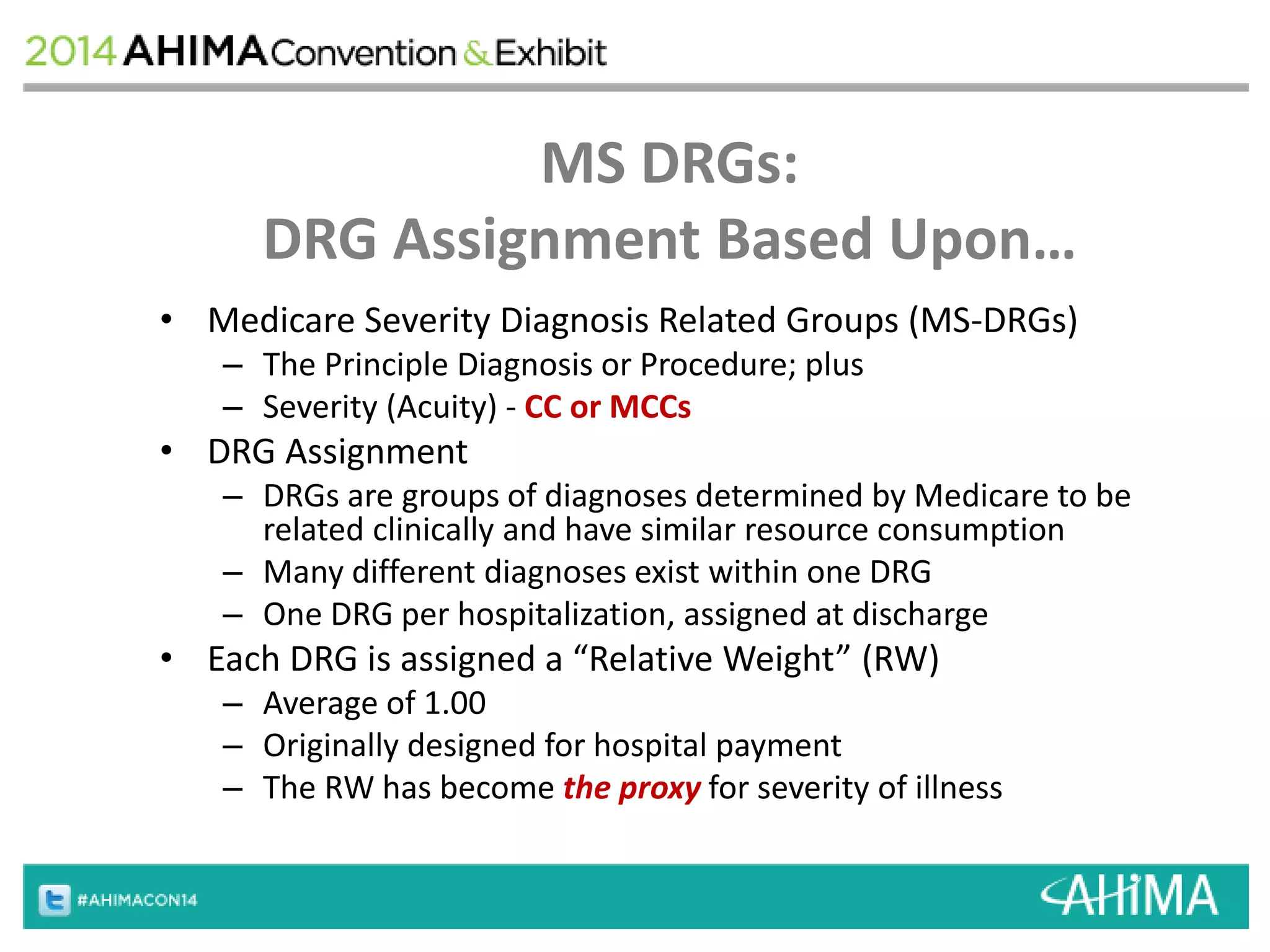
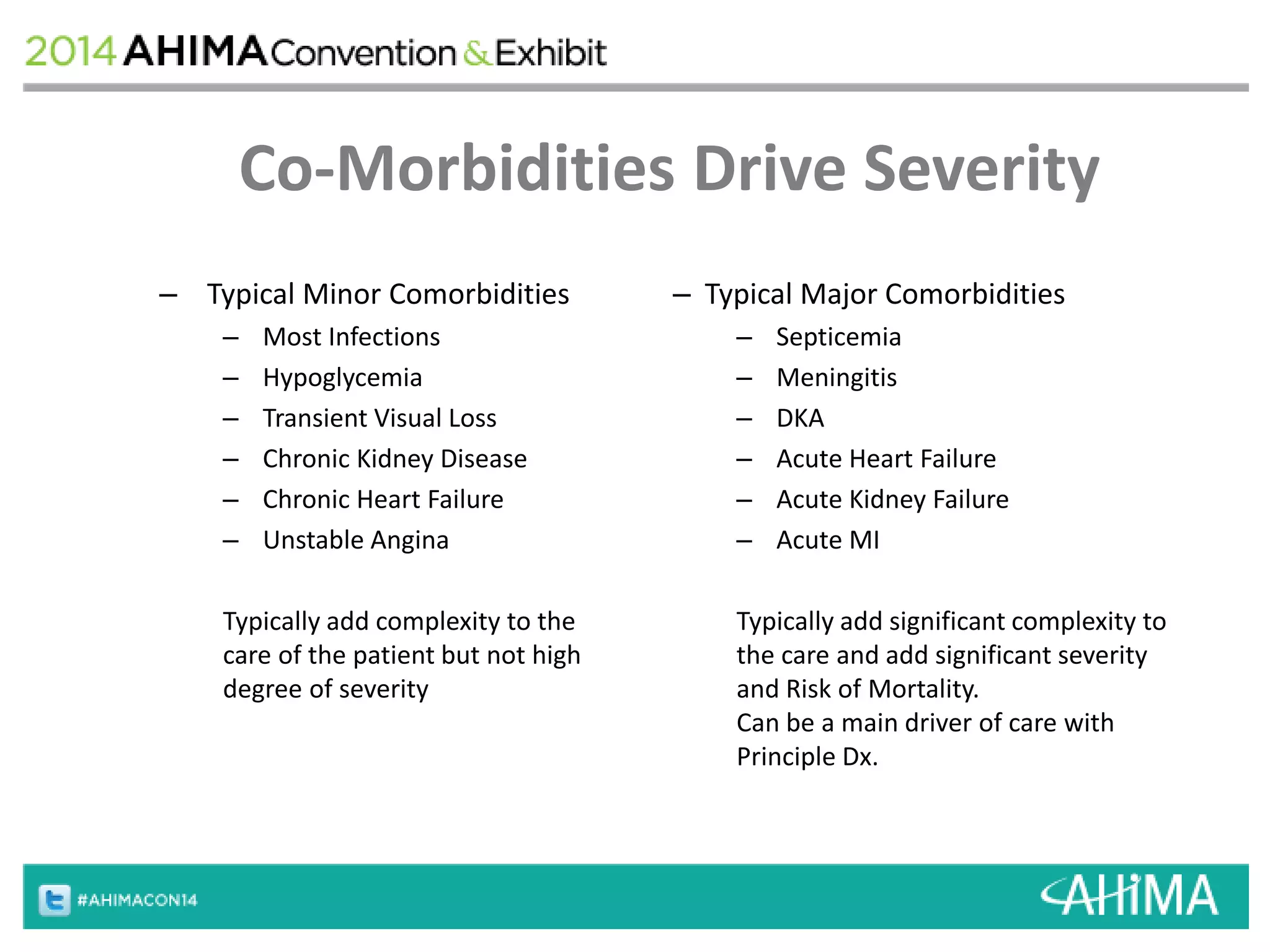
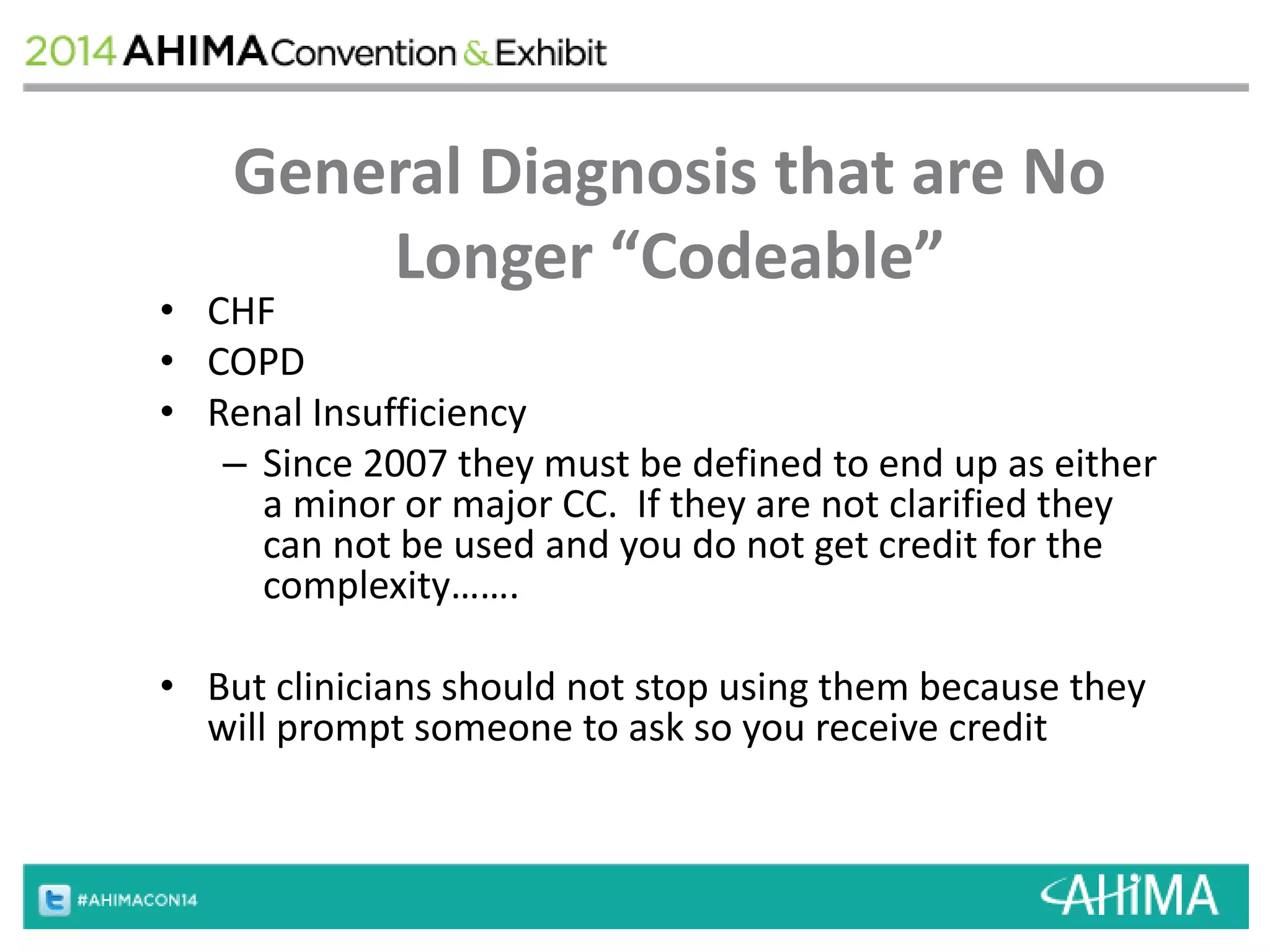
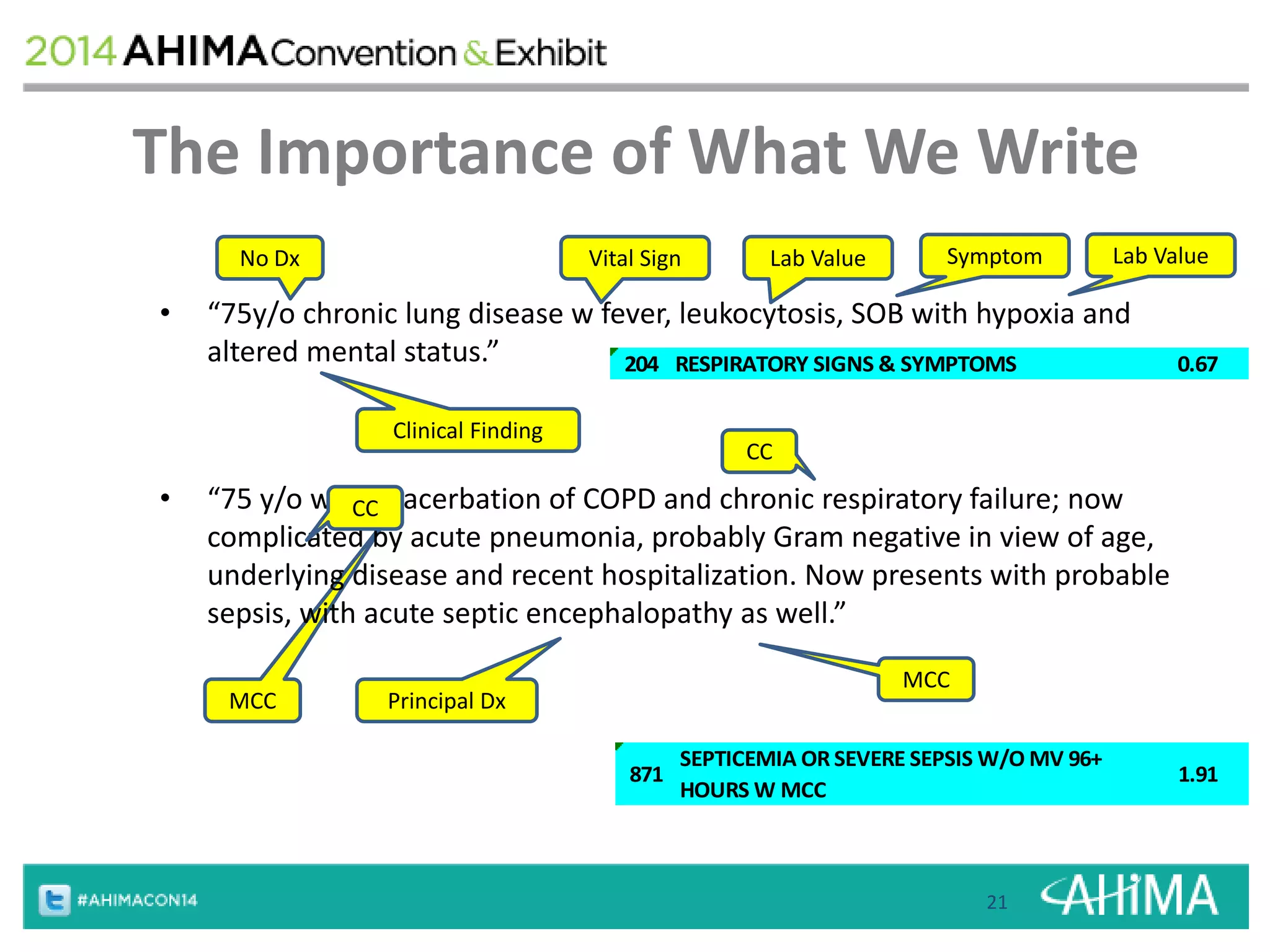
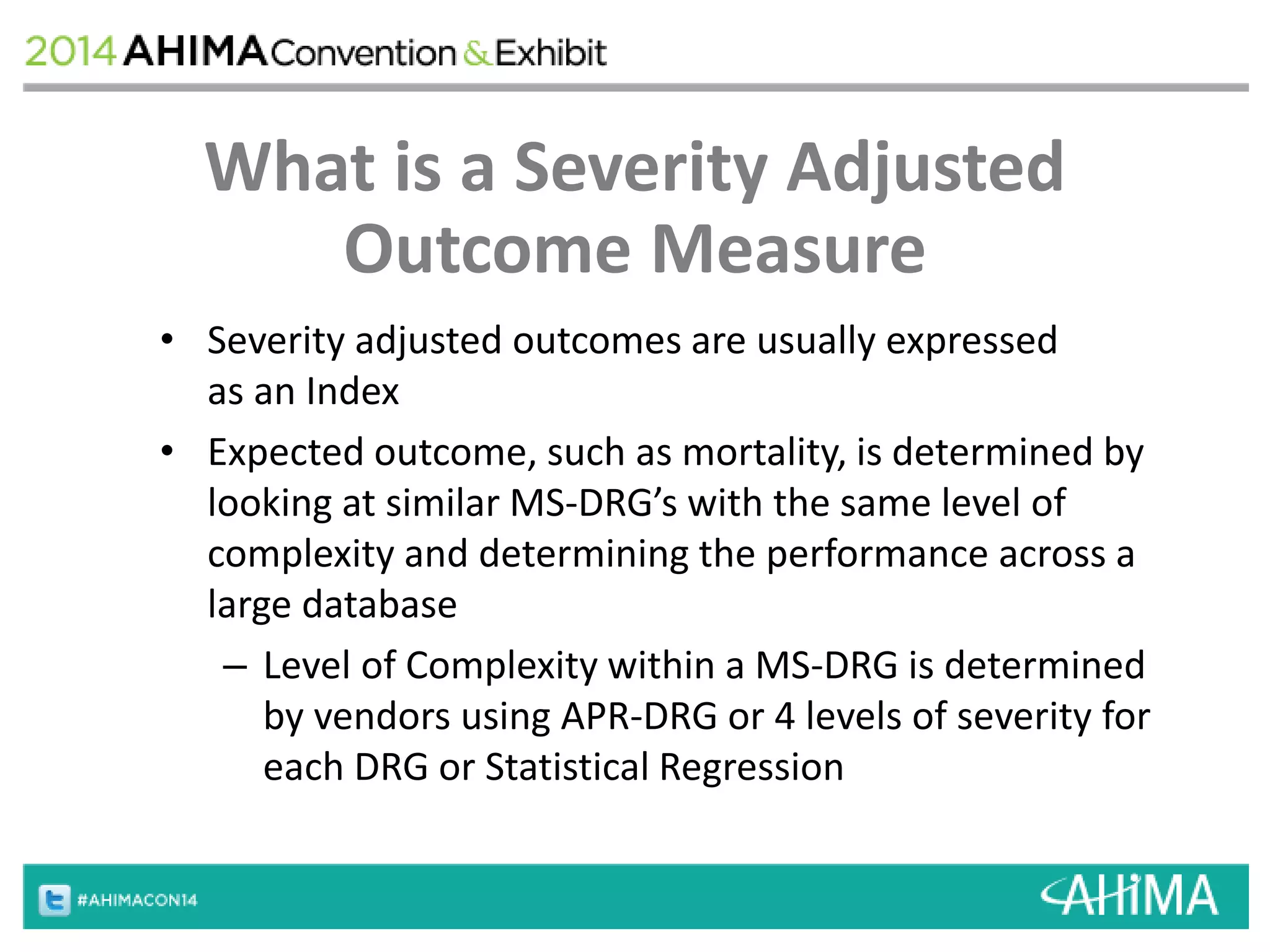
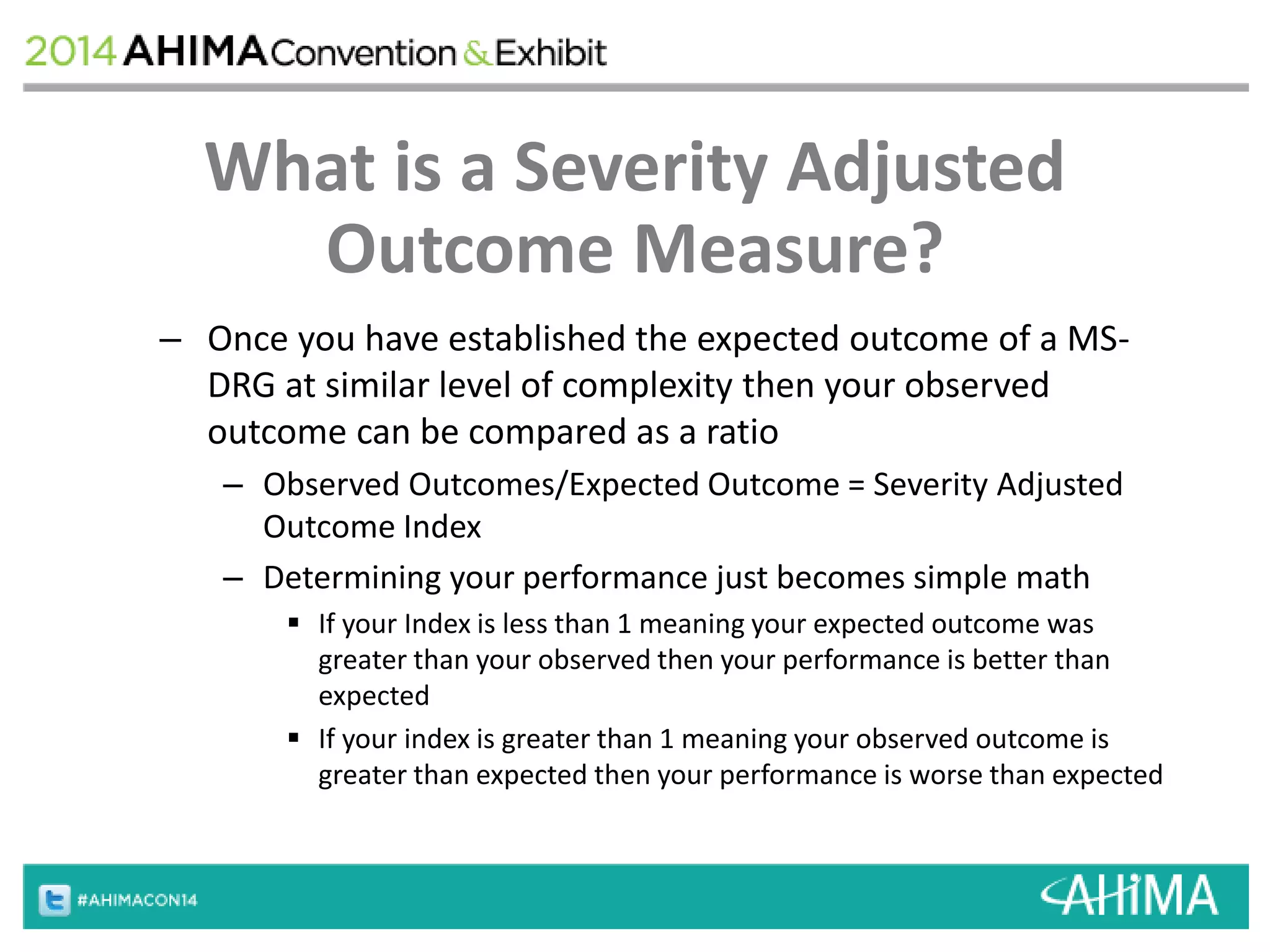
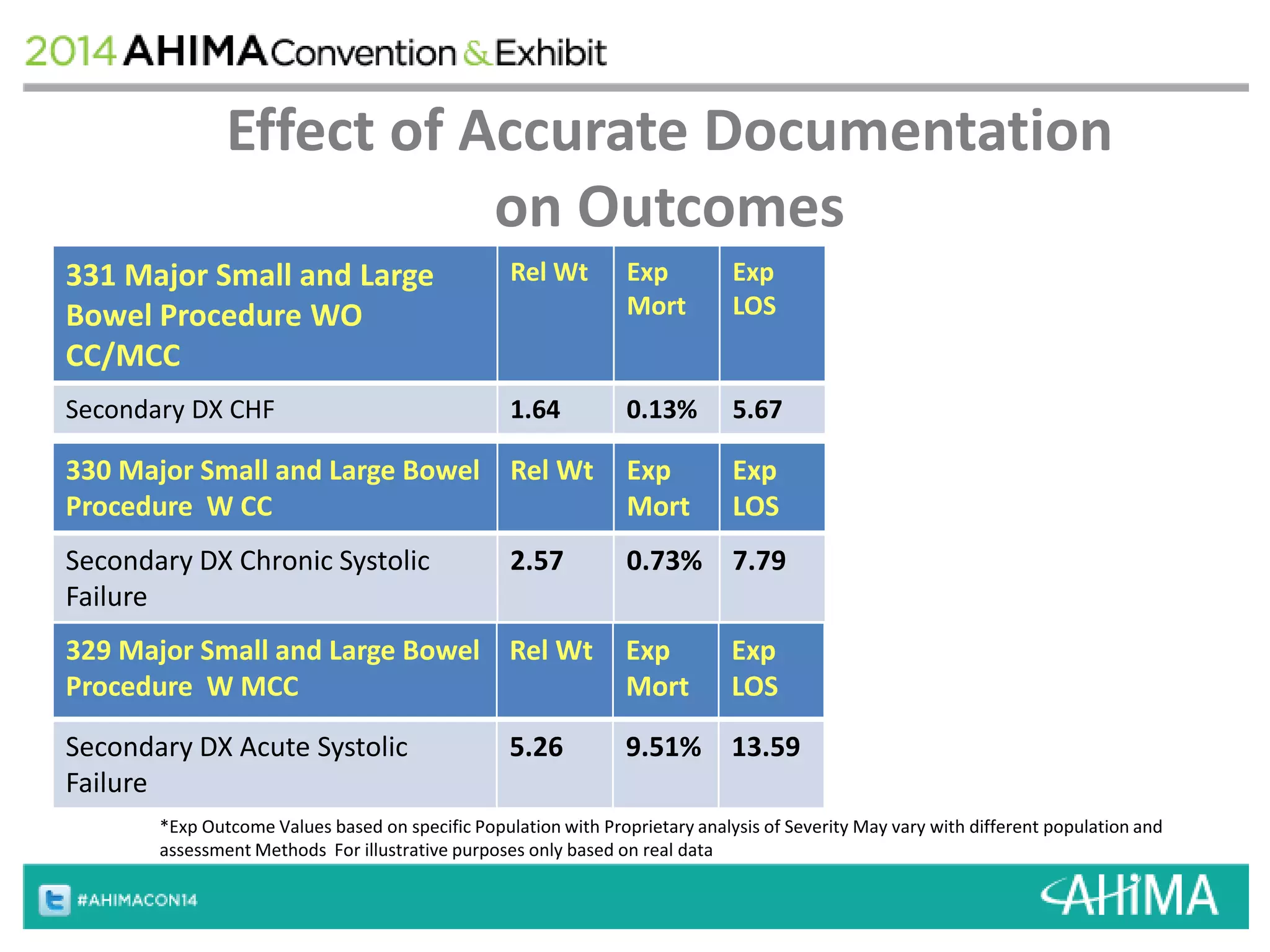
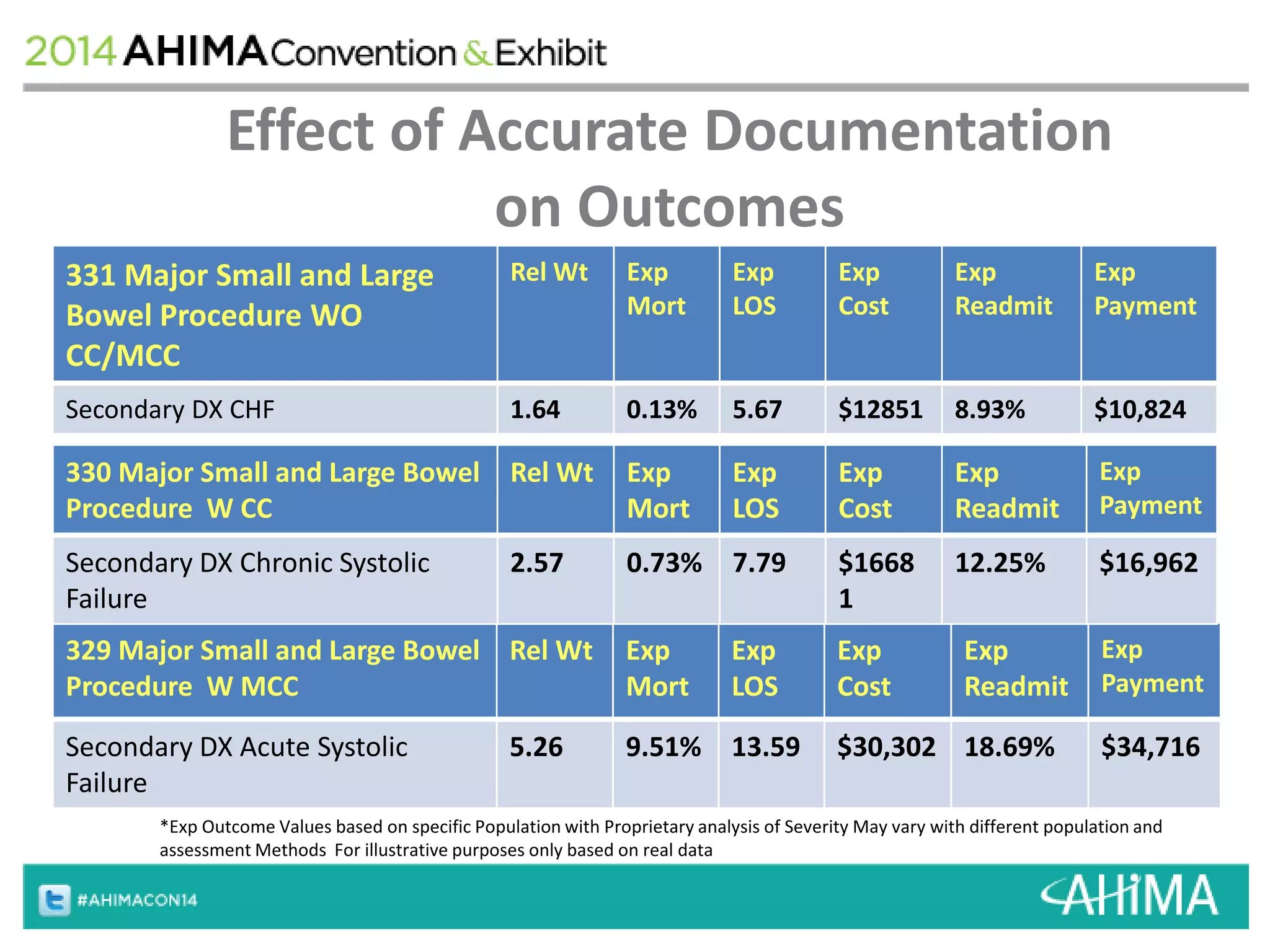
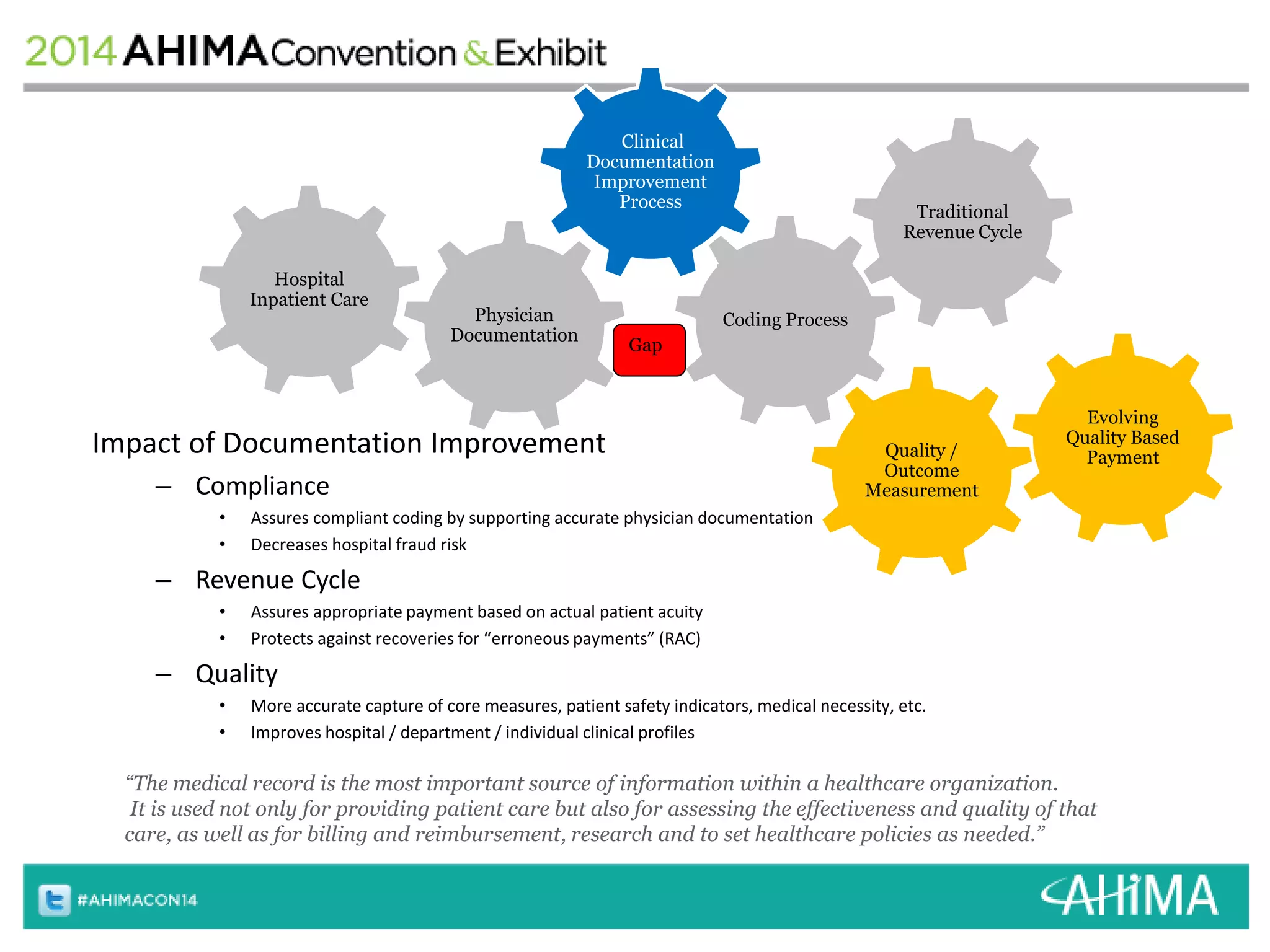
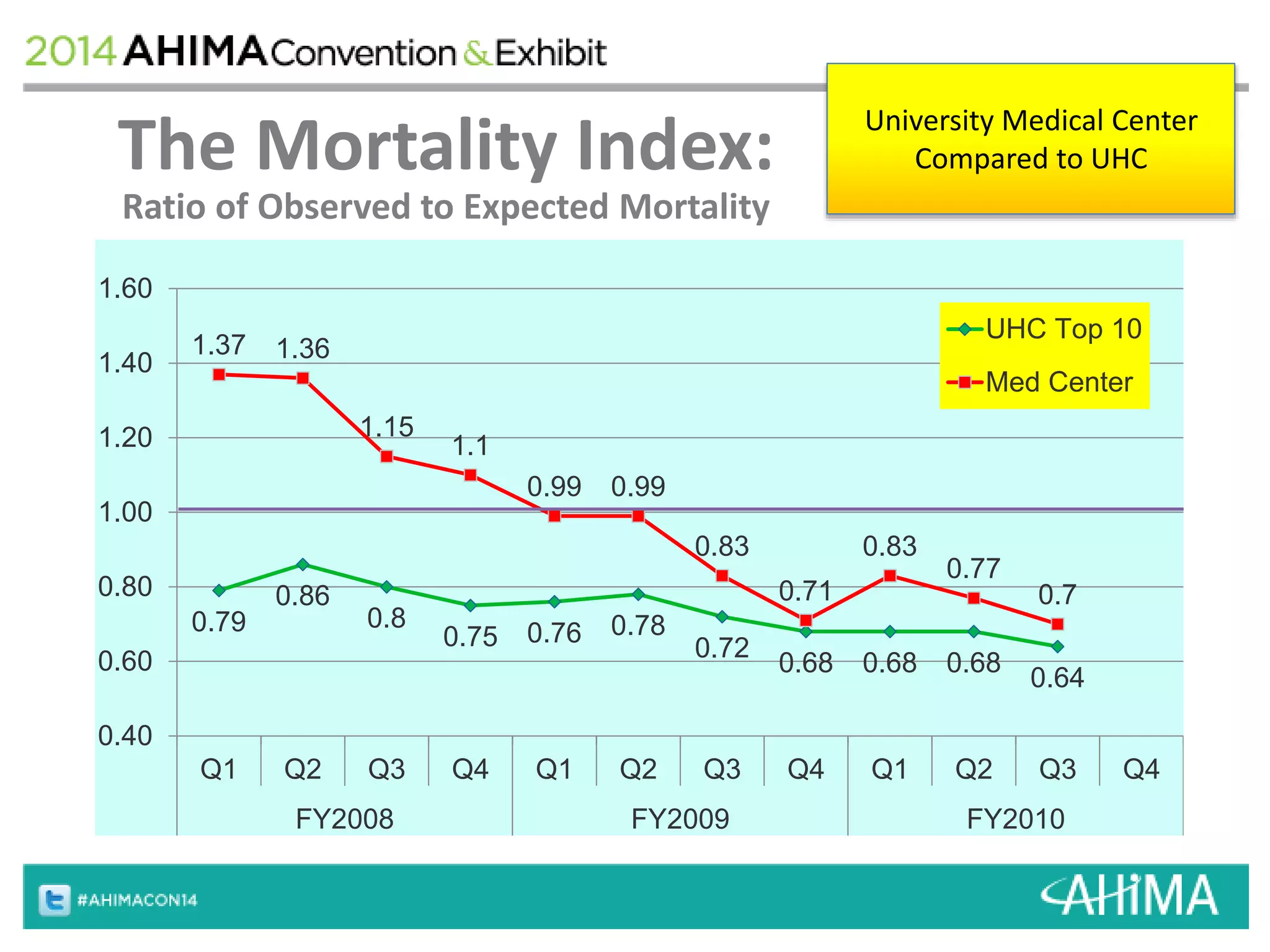
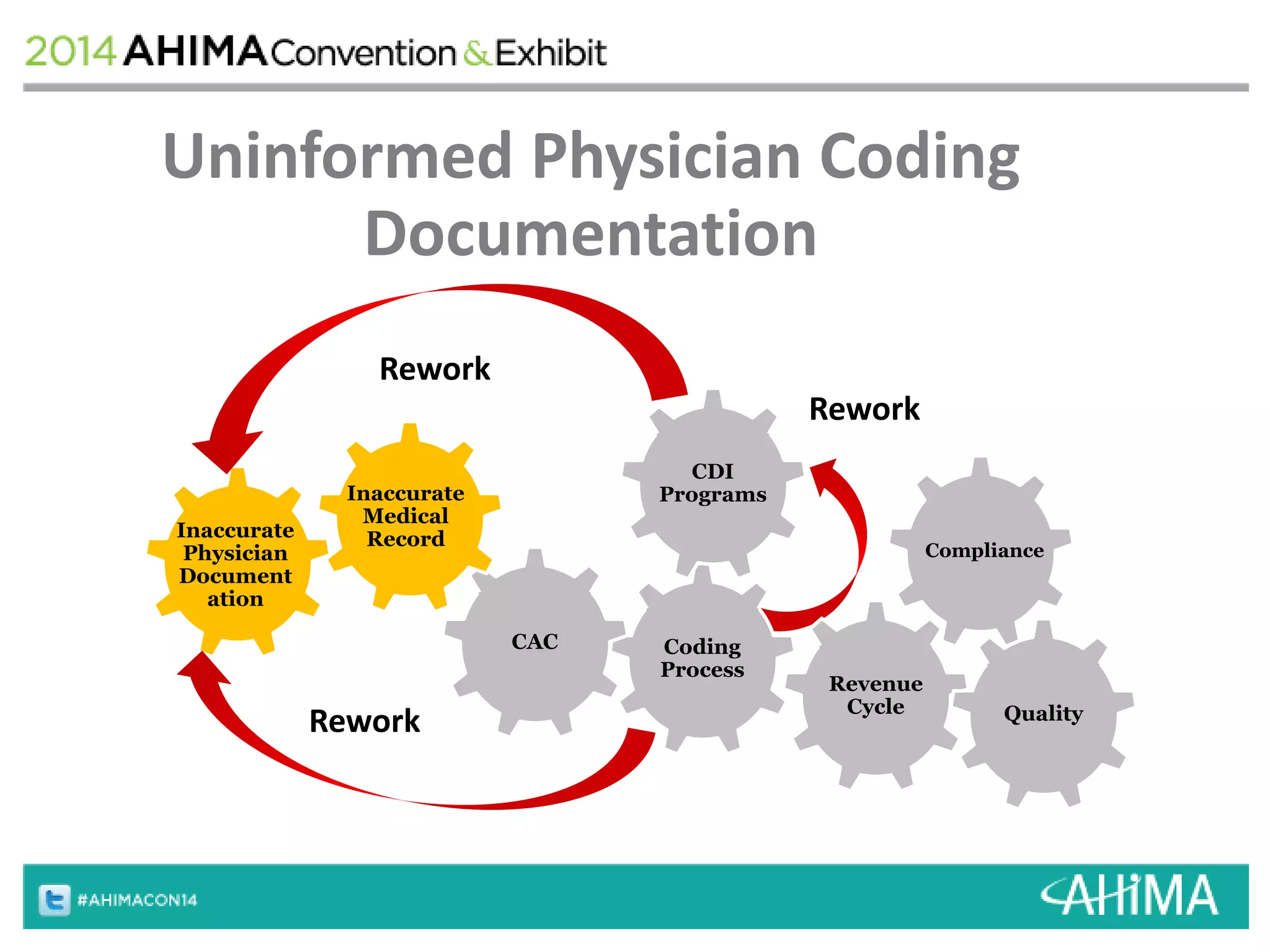
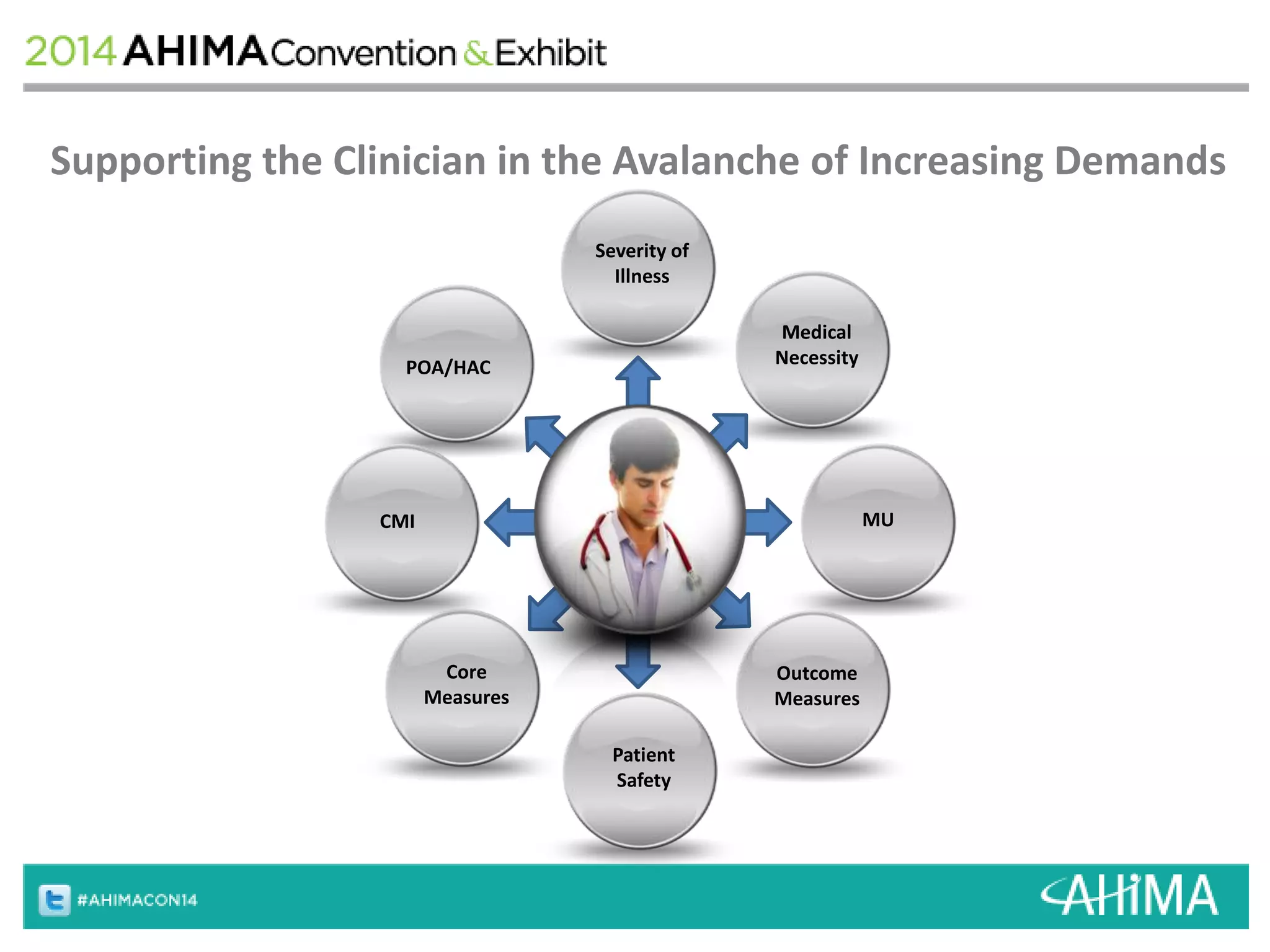
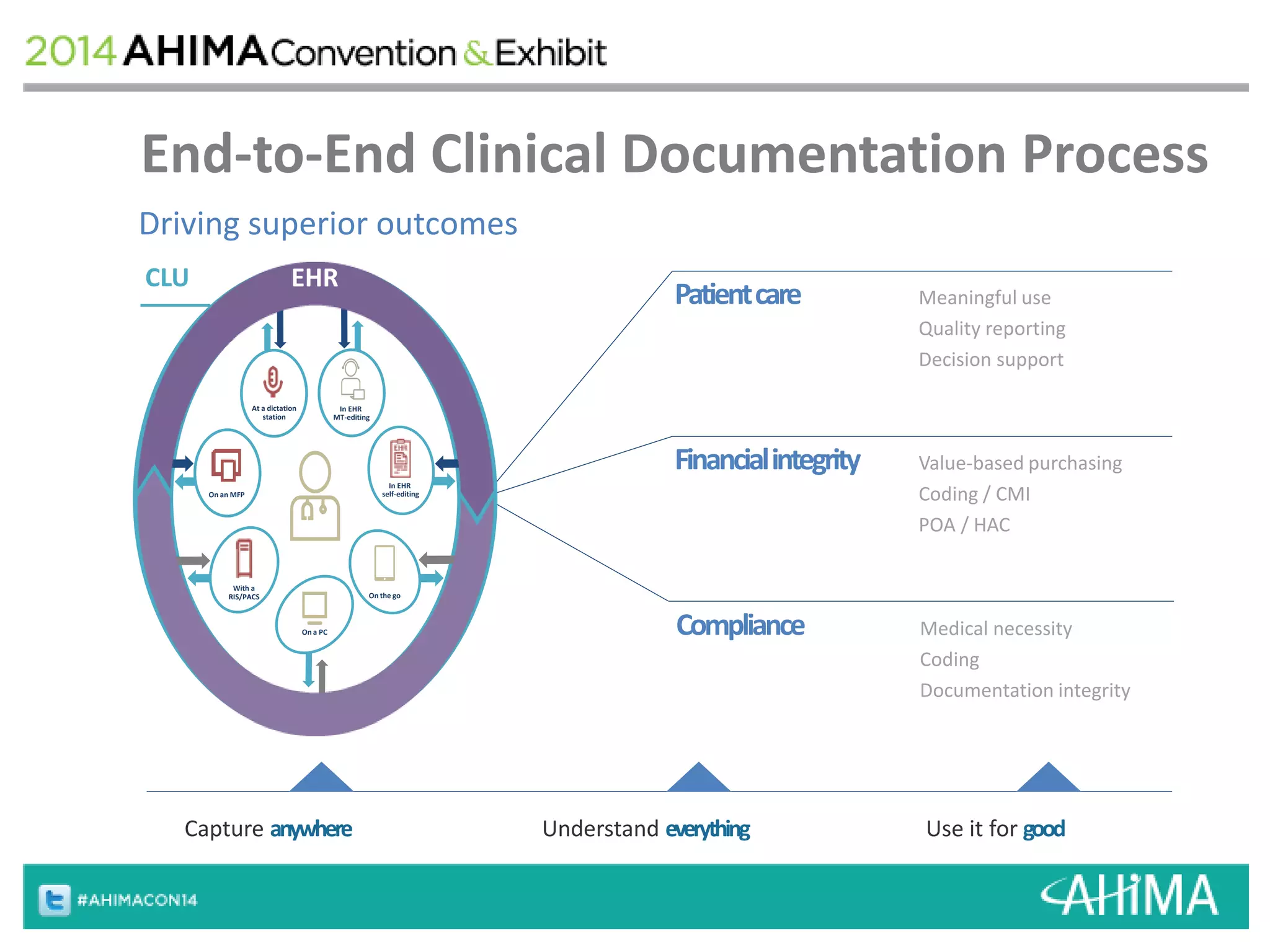
The document provides an overview of ICD-10 implementation and the impact of clinical documentation on outcomes and reimbursement. It discusses how accurate documentation is important for determining severity of illness and risk adjustment, which drives hospital reimbursement and quality metrics. It emphasizes that physicians need to fully document their clinical decision making to avoid issues like payment denials, penalties, or inaccurate performance assessments that could arise from incomplete records.
![ICD-10 History
• ICD-10 adopted by the World Health Organization in 1990
– Implemented in the United Kingdom in 1995
– Australian modification released in 1998
– Canadian version 2001
• US development
– US evaluation by the National Center for Health Statistics began 1994
– Numerous subsequent versions
– Final implementation date 10/01/14
• The official documents
– International Classification of Diseases, Tenth Revision, Clinical
Modification [ICD-10-CM]
– International Classification of Diseases, Tenth Revision, Procedure
Coding System [ICD-10-PCS]](https://image.slidesharecdn.com/jgb6losq8opwhinhnbfv-signature-05b9a2434b4f869f4865f601cf791672fde6c15bea64a132ce668658bb86c2e3-poli-140930204529-phpapp01/75/Game-of-documentation-Winter-is-coming-Surviving-ICD10-5-2048.jpg)