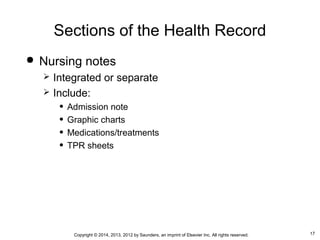
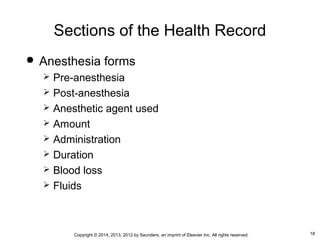
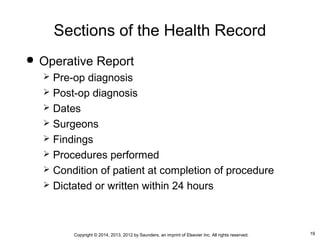
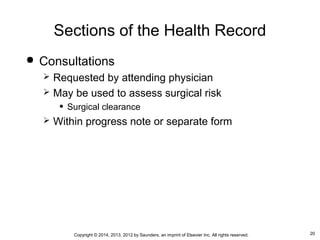
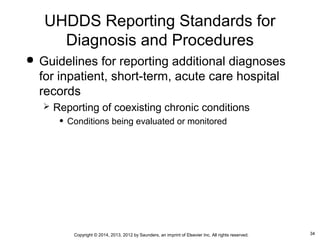
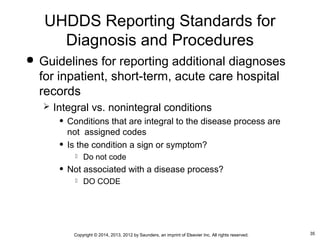
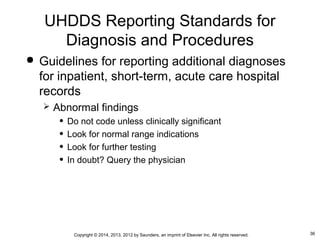
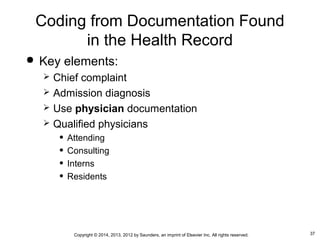
This document discusses the health record as the foundation of medical coding. It describes the various sections and forms that make up a health record, including administrative data, clinical reports, diagnostic testing results, and discharge summaries. It also outlines standards for reporting diagnoses and procedures coded from the health record, including defining principal diagnosis and procedure and providing guidelines for coding additional secondary diagnoses. The importance of using documentation from qualified physicians in the health record and querying physicians when needed to clarify the clinical picture is also emphasized.