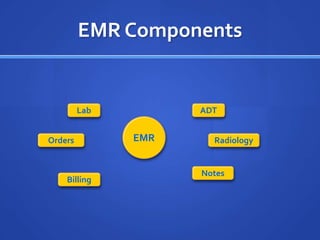
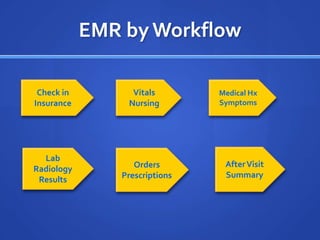
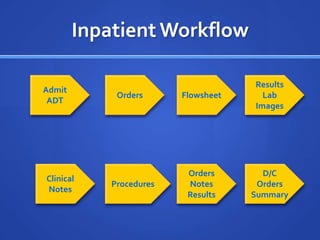
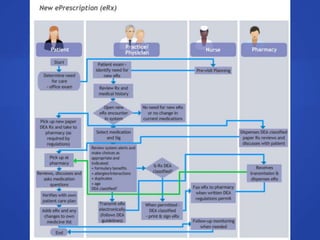
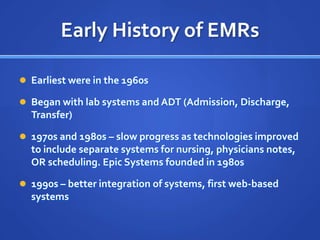
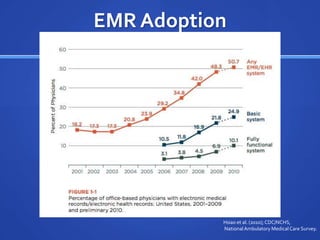
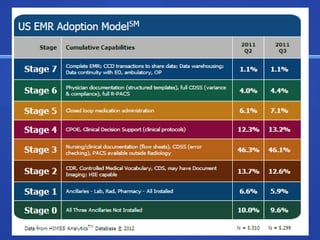
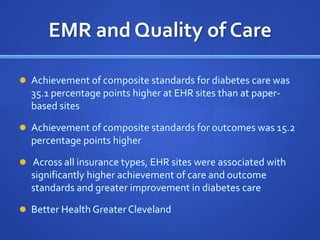
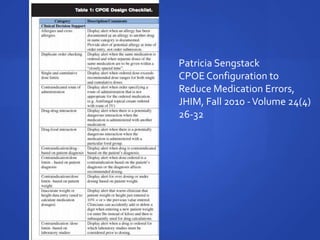
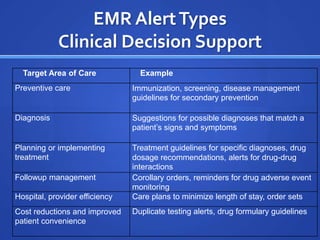
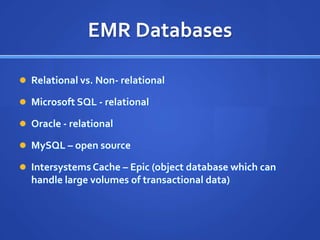
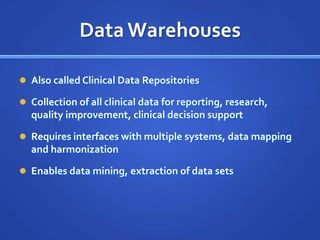
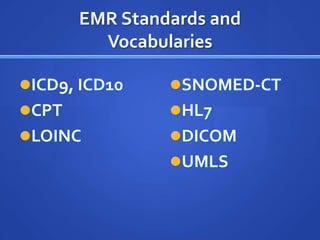
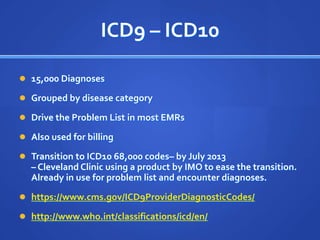
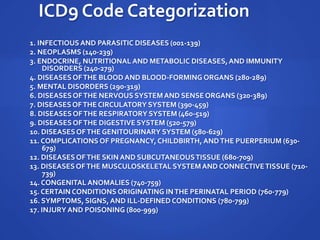
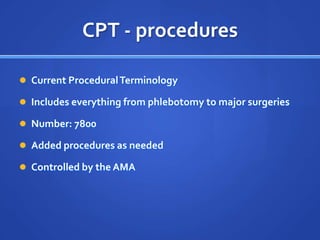
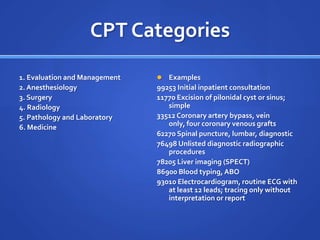
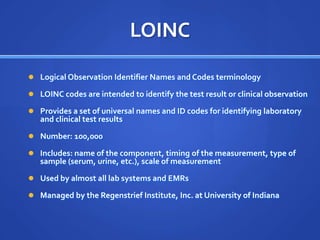
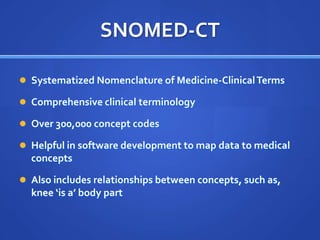
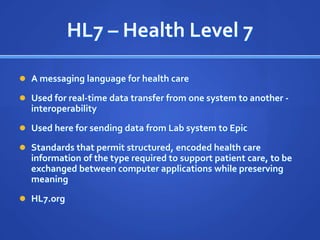
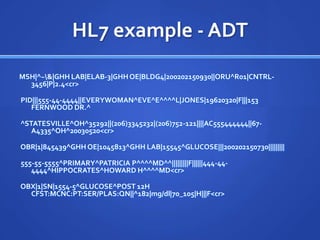
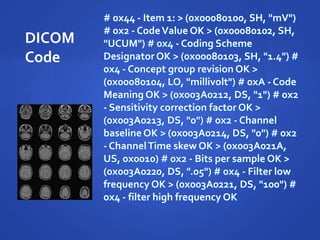
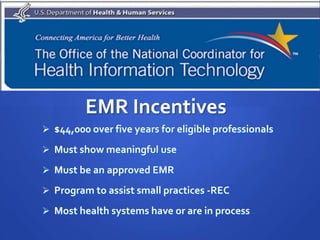
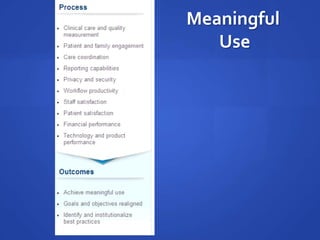
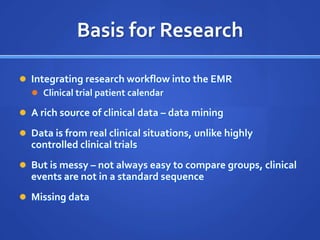
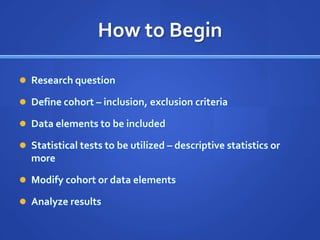
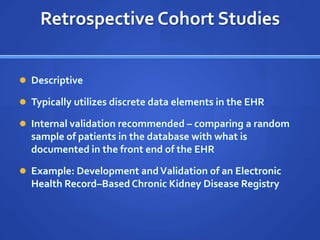
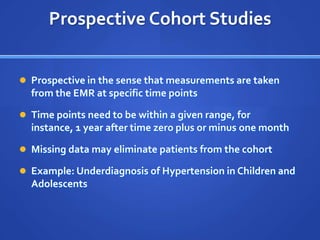
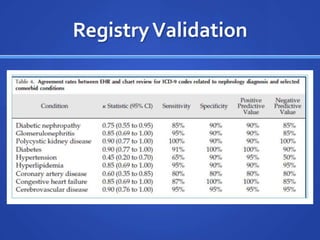
This document provides an outline for a presentation on electronic medical records (EMRs). It begins with defining the components of an EMR, including labs, admissions/discharge/transfer data, orders, radiology, notes, and billing. It then discusses the history and adoption of EMRs from the 1960s to present. The document reviews studies showing the effectiveness of EMRs in improving quality of care and achieving treatment standards. It also outlines how EMR data is structured in databases and data warehouses and describes common health data standards like ICD, CPT, LOINC, SNOMED, and HL7. The presentation covers meaningful use incentives and provides examples of using EMR data for research studies.