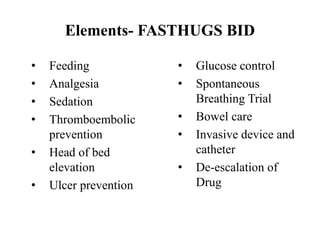
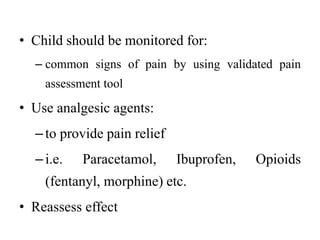
Routine care in the PICU is important for several reasons: it facilitates the identification of clinical issues, encourages patient-centered care, and helps prevent hospital-acquired infections. The key elements of routine care in the PICU are known by the acronym FASTHUGS BID, and include feeding, analgesia, sedation, thromboembolic prevention, head of bed elevation, ulcer prevention, glucose control, spontaneous breathing trials, bowel care, and catheter/line care. Providing this routine care is essential for all patients in the PICU.