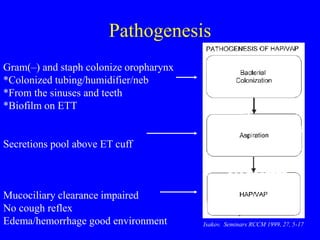
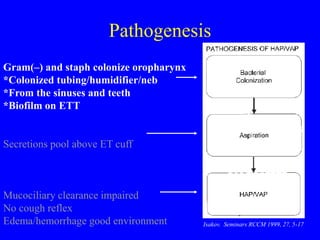
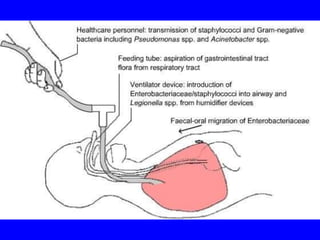
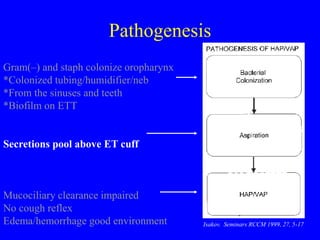
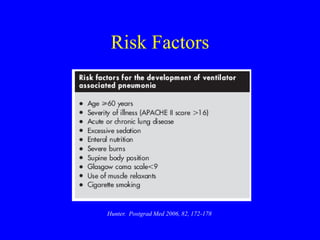
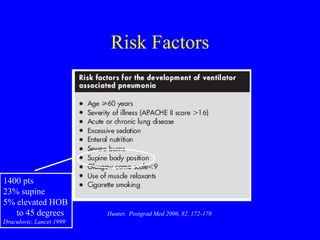
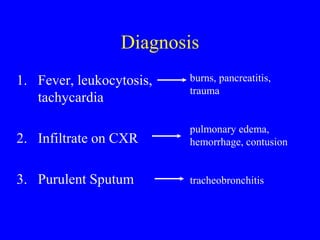
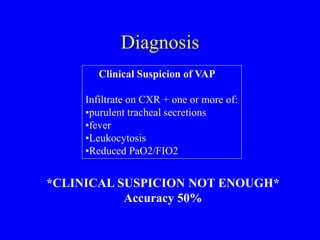
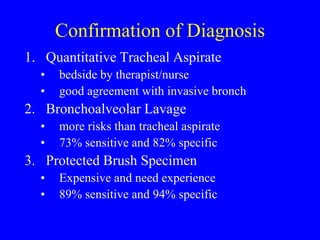
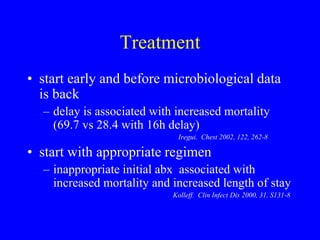
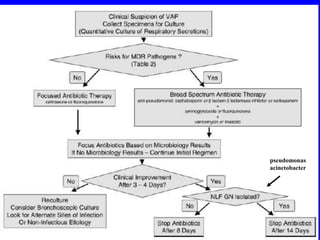
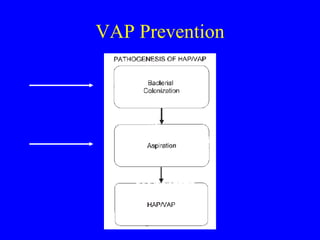
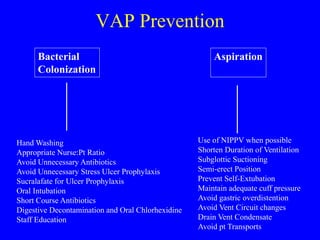
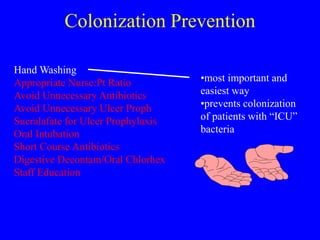
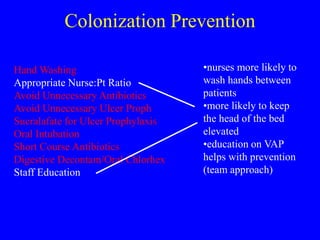
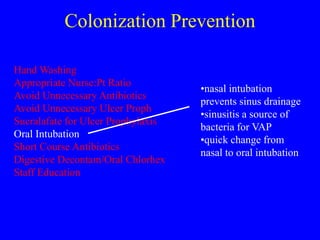
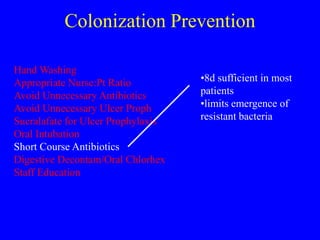
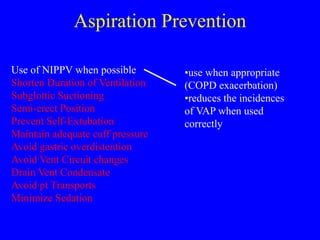
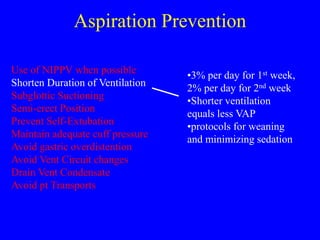
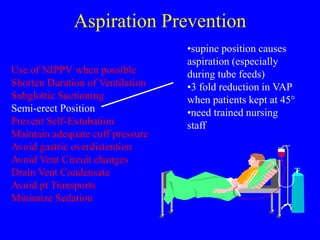
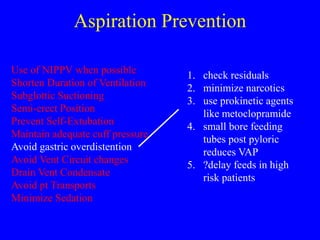
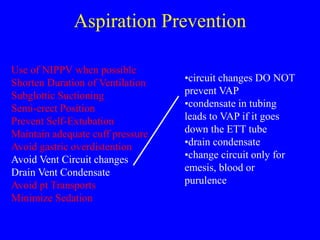
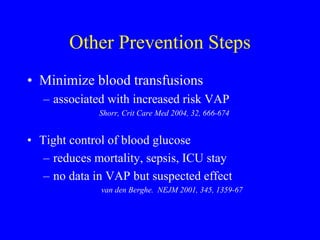
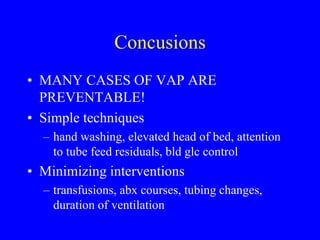
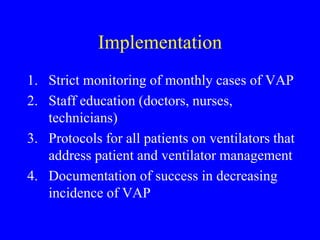
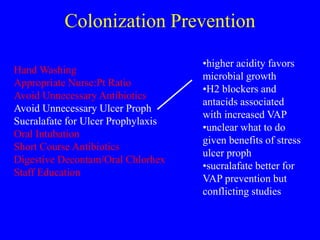
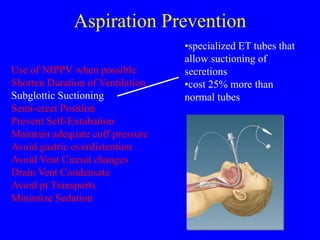
Ventilator-associated pneumonia (VAP) is difficult to diagnose and treat, prolongs hospital stays, increases mortality, and is expensive to manage. While up to 28% of ventilated patients may develop VAP, many cases are preventable through measures like hand hygiene, keeping patients semi-erect, minimizing sedation and intubation duration, and using specialized endotracheal tubes that allow subglottic suctioning of secretions. Proper diagnosis and early, targeted antibiotic treatment can improve outcomes for patients who do develop VAP.