Embed presentation

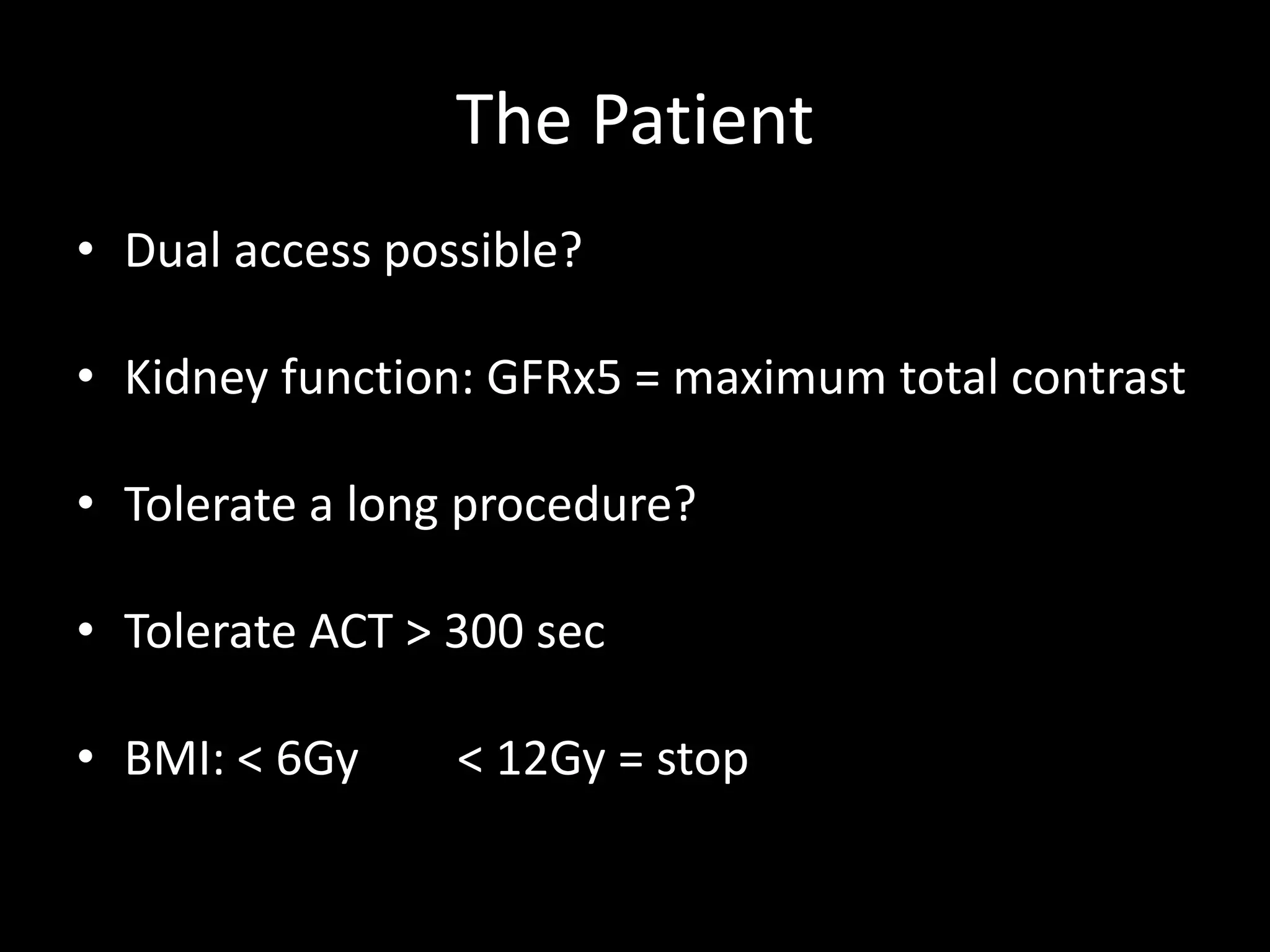
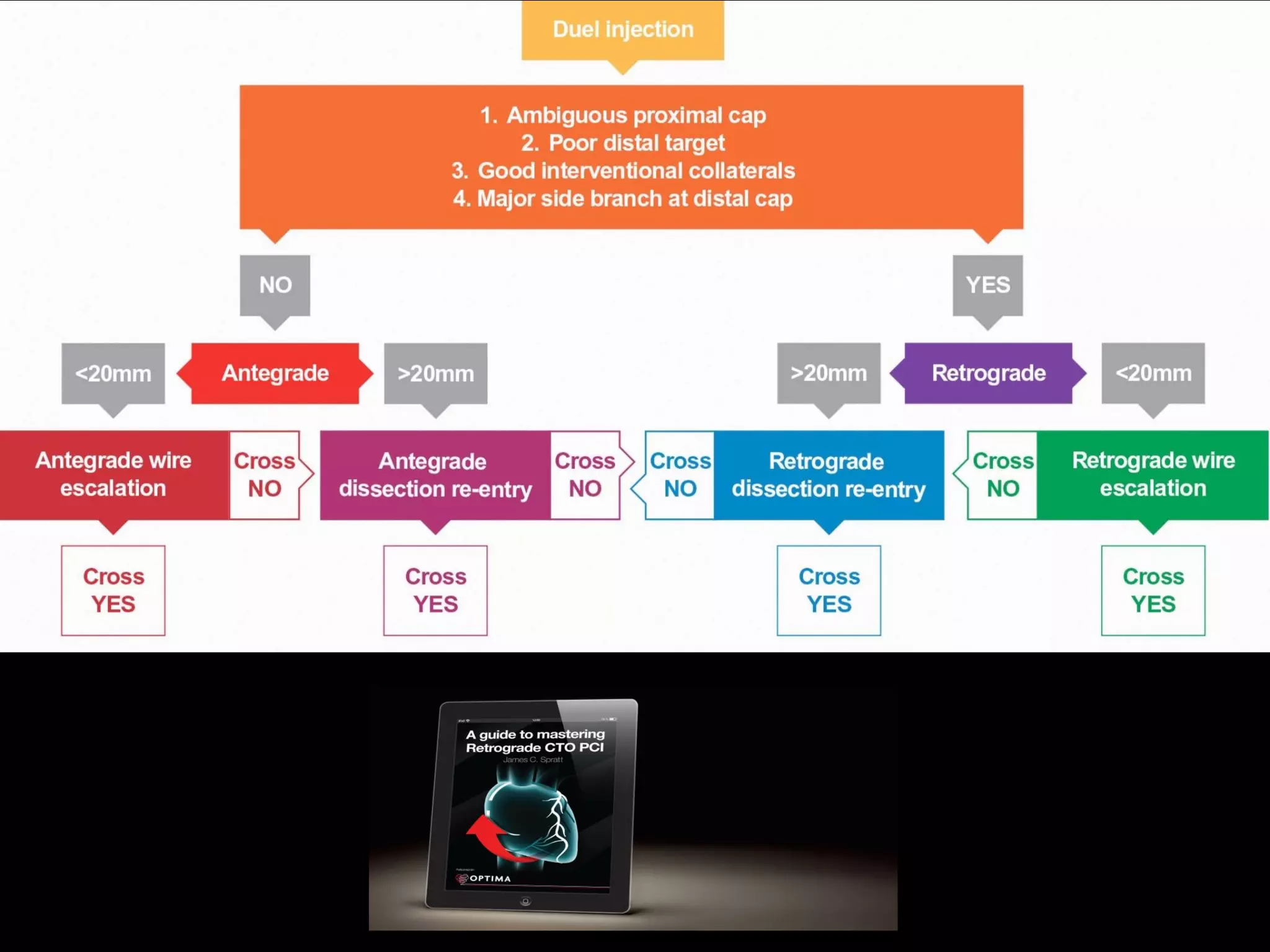
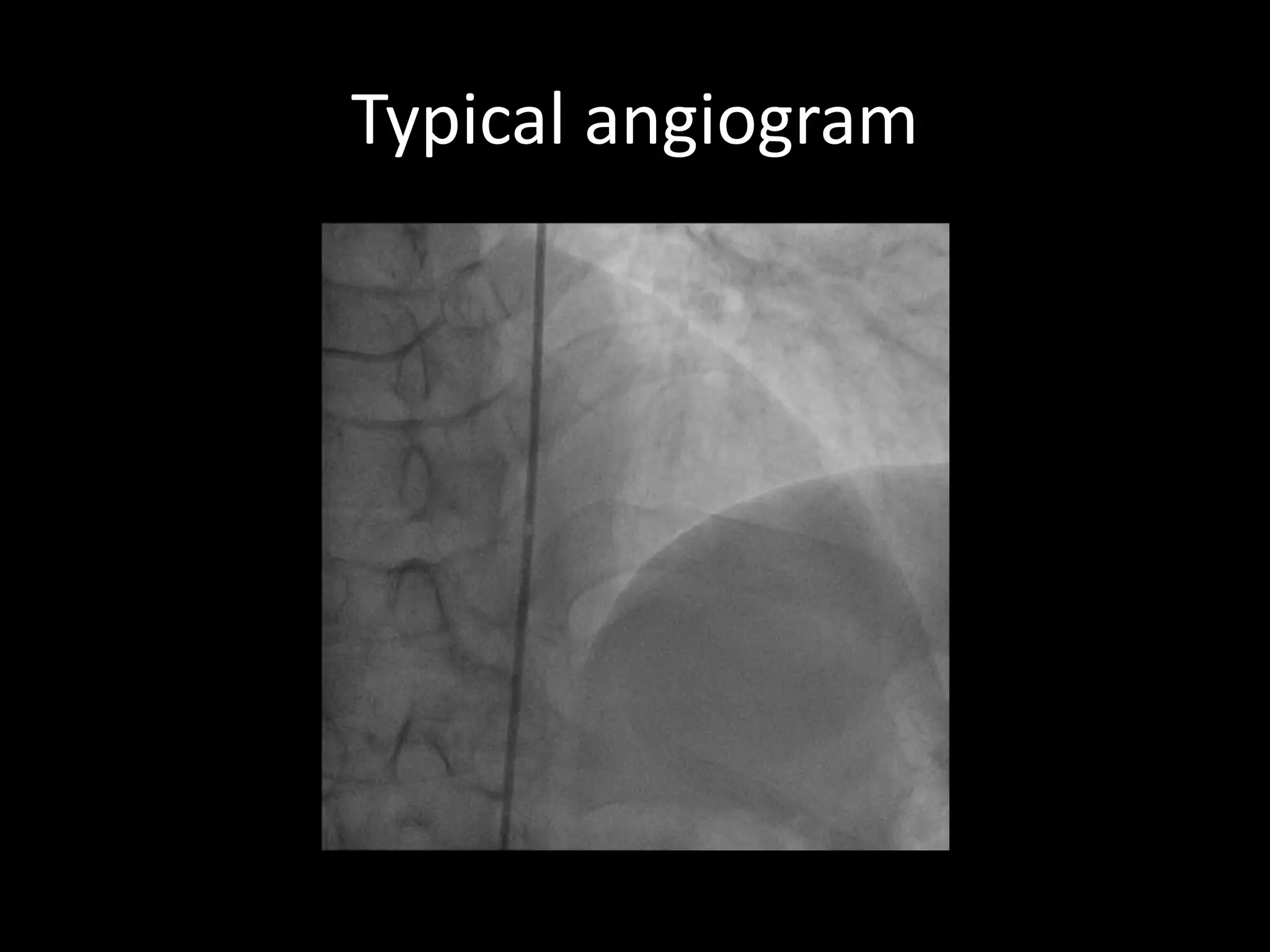
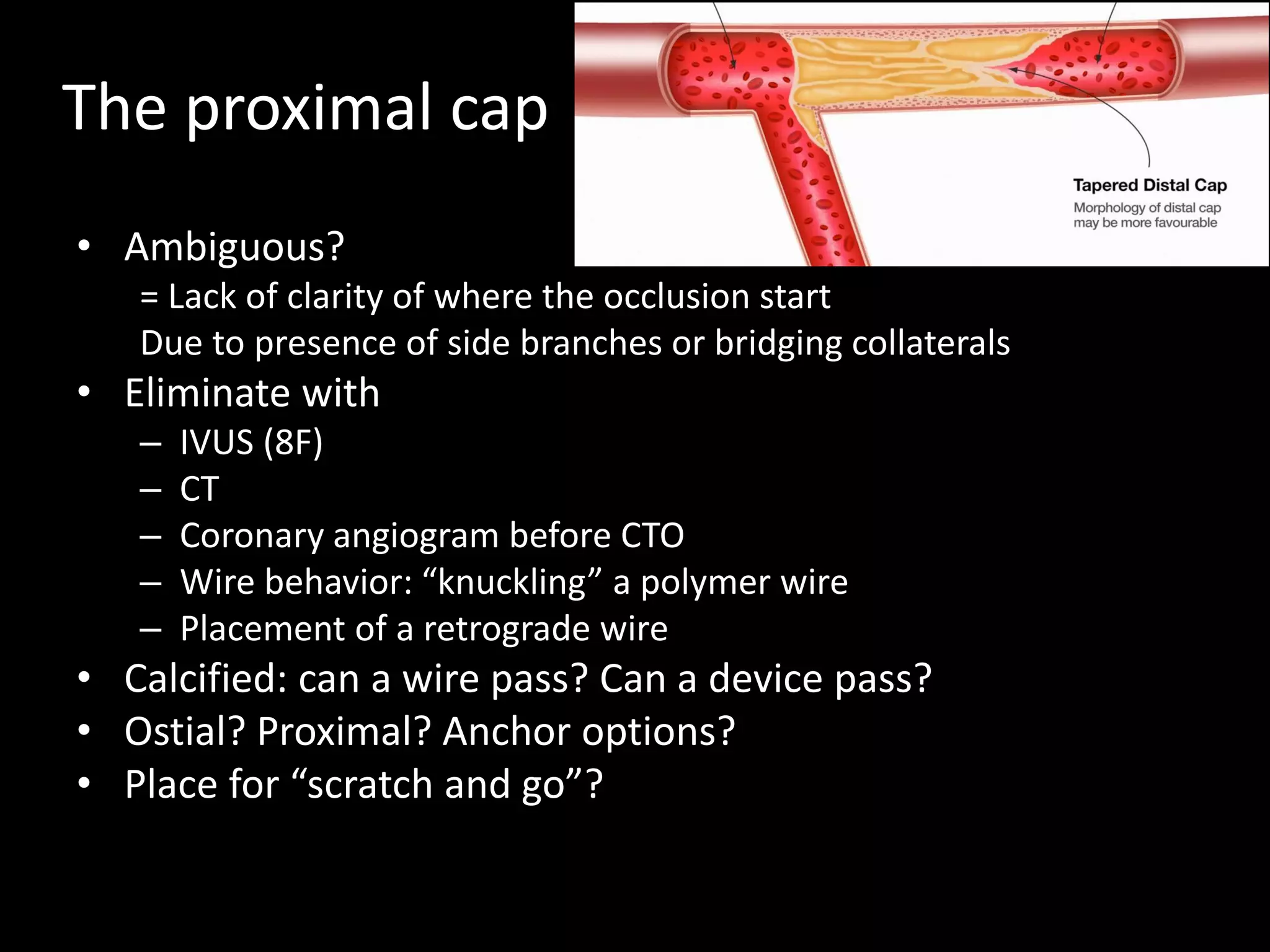
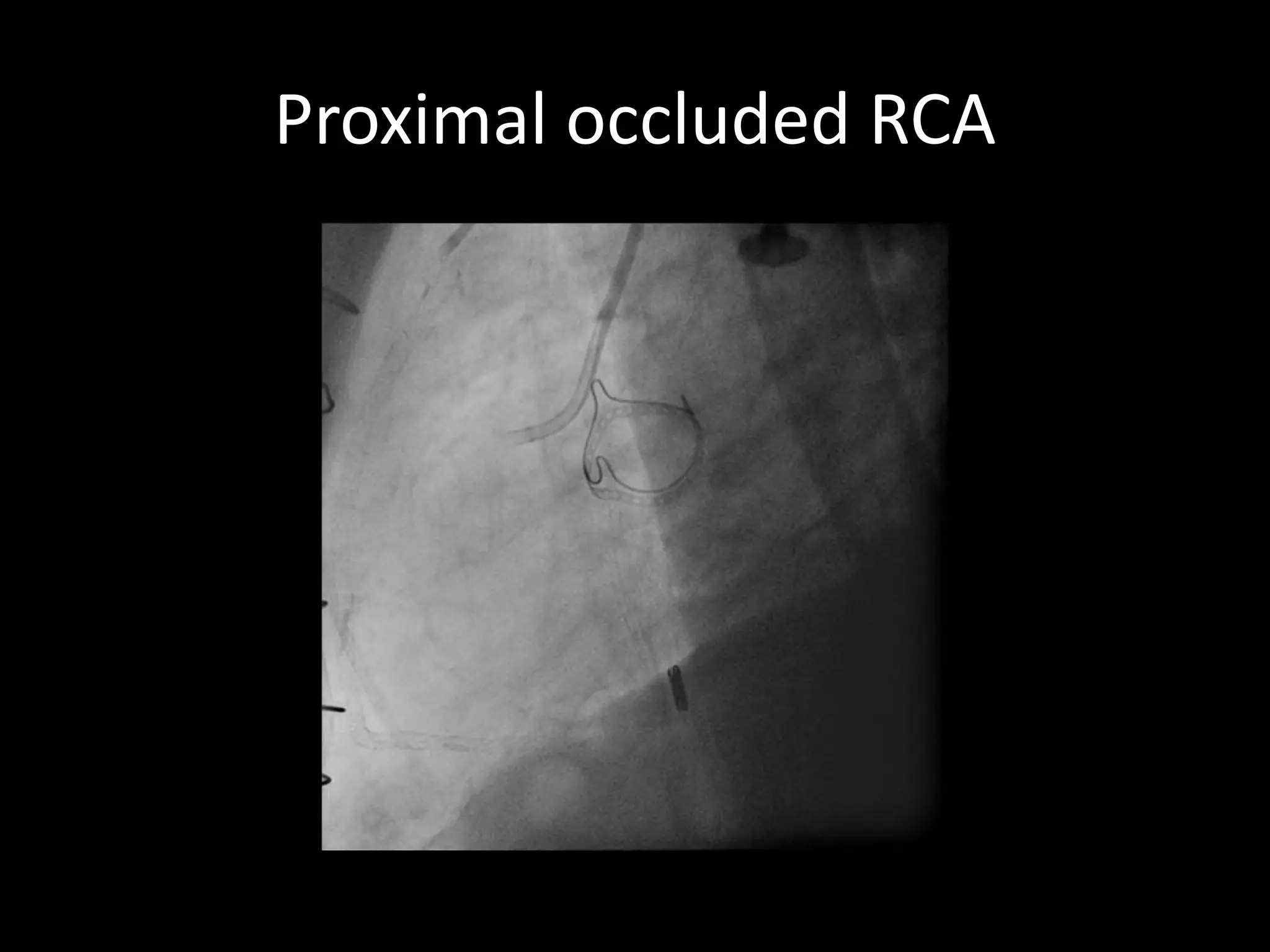
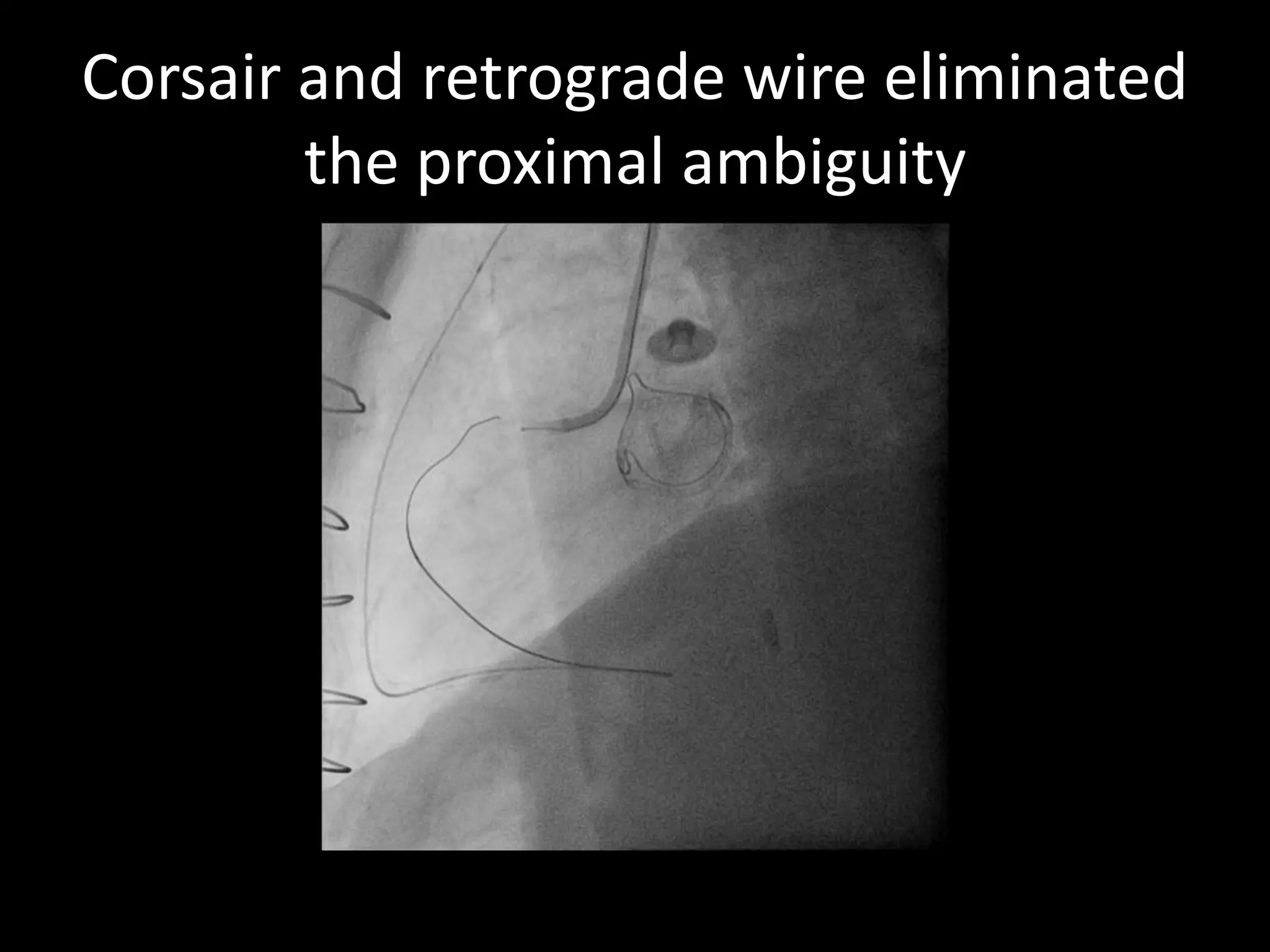
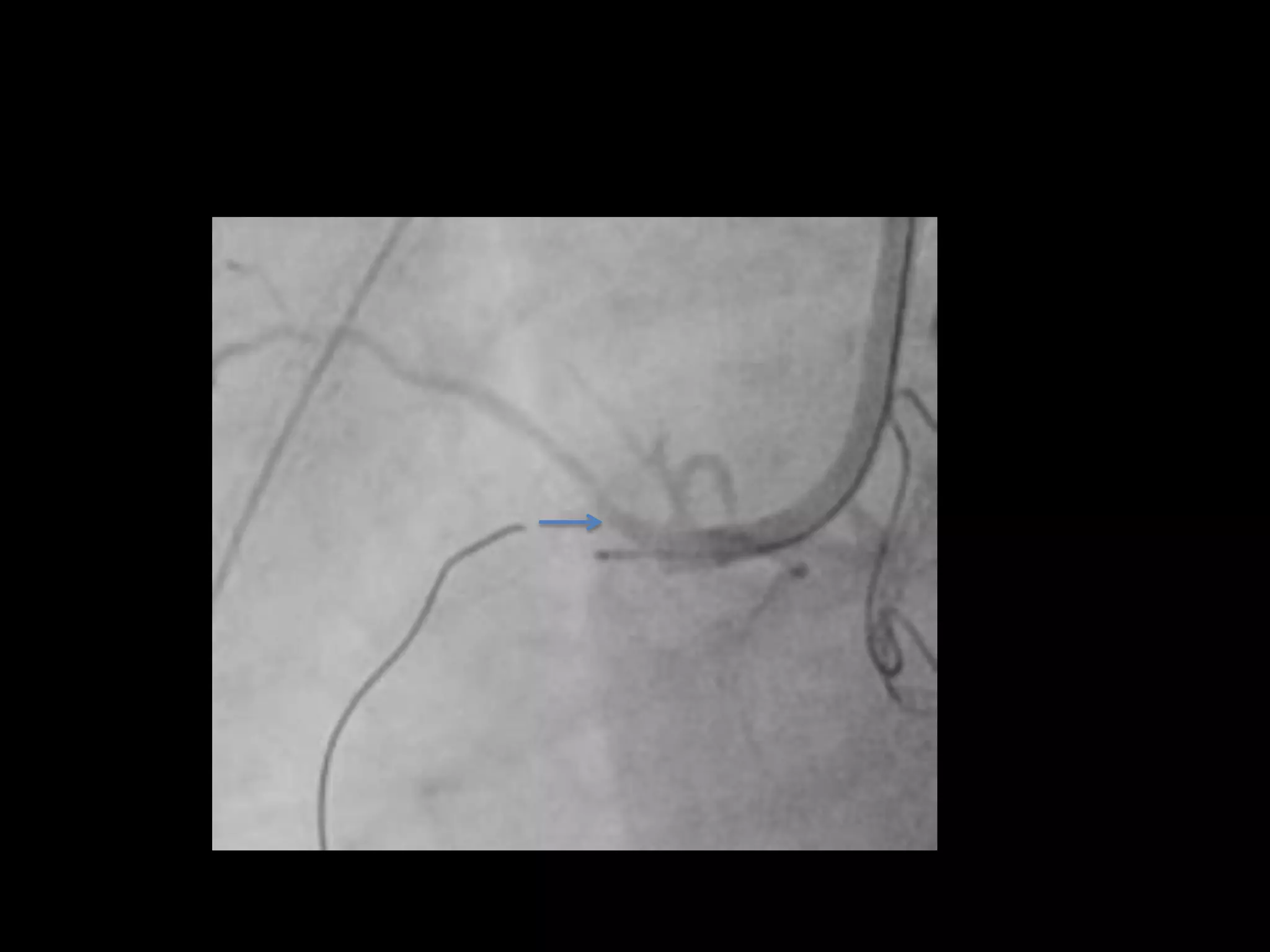
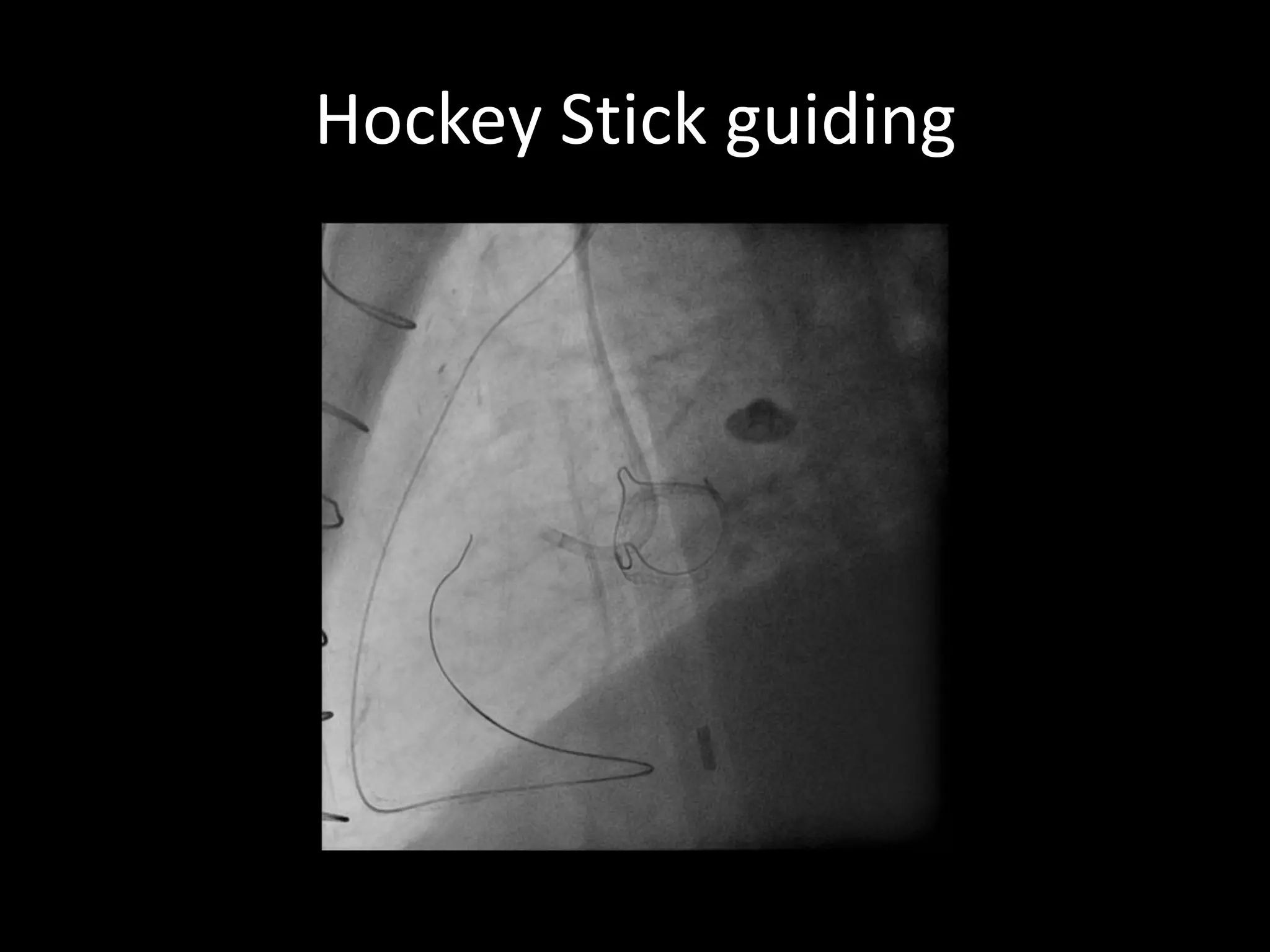
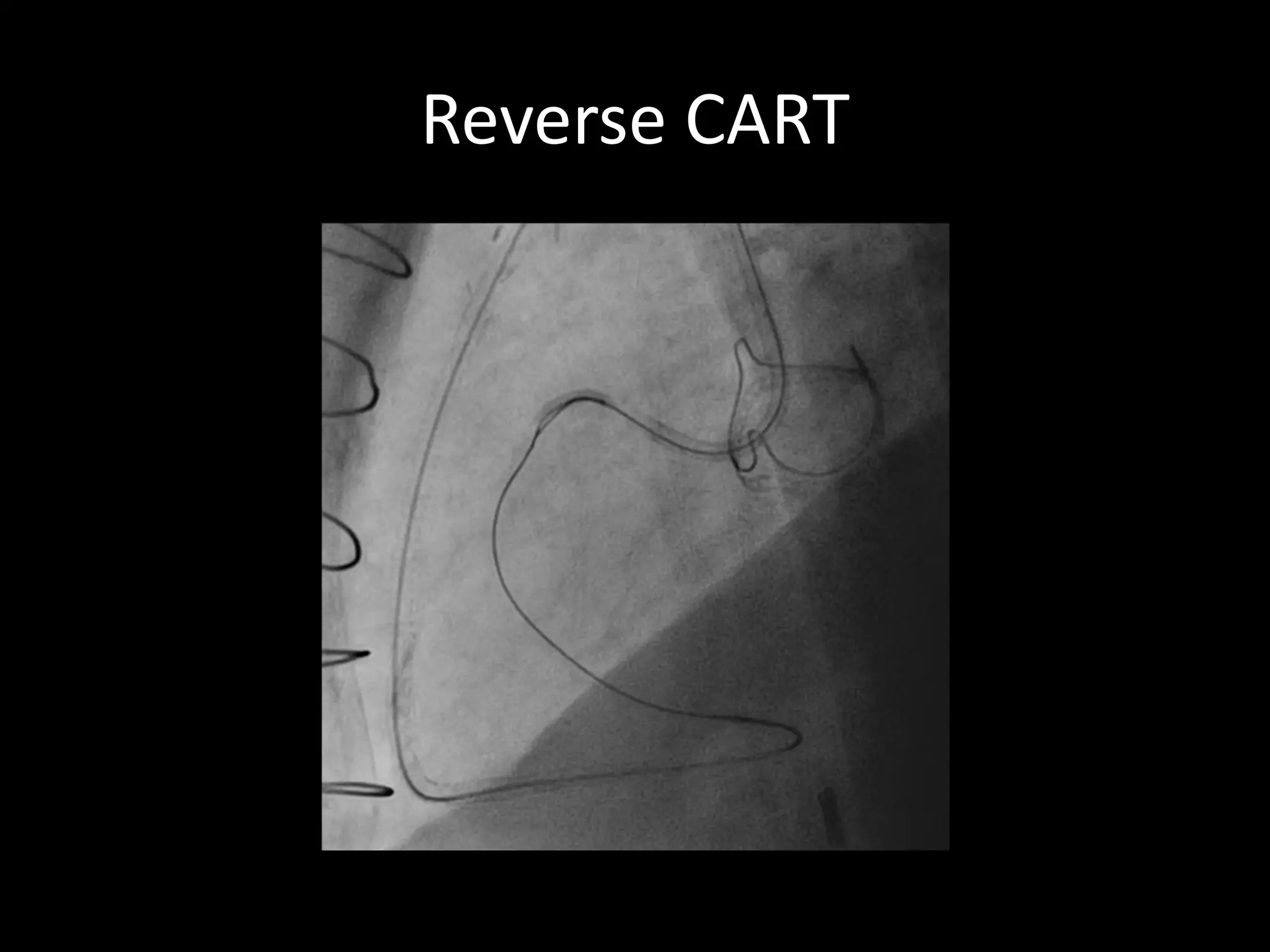
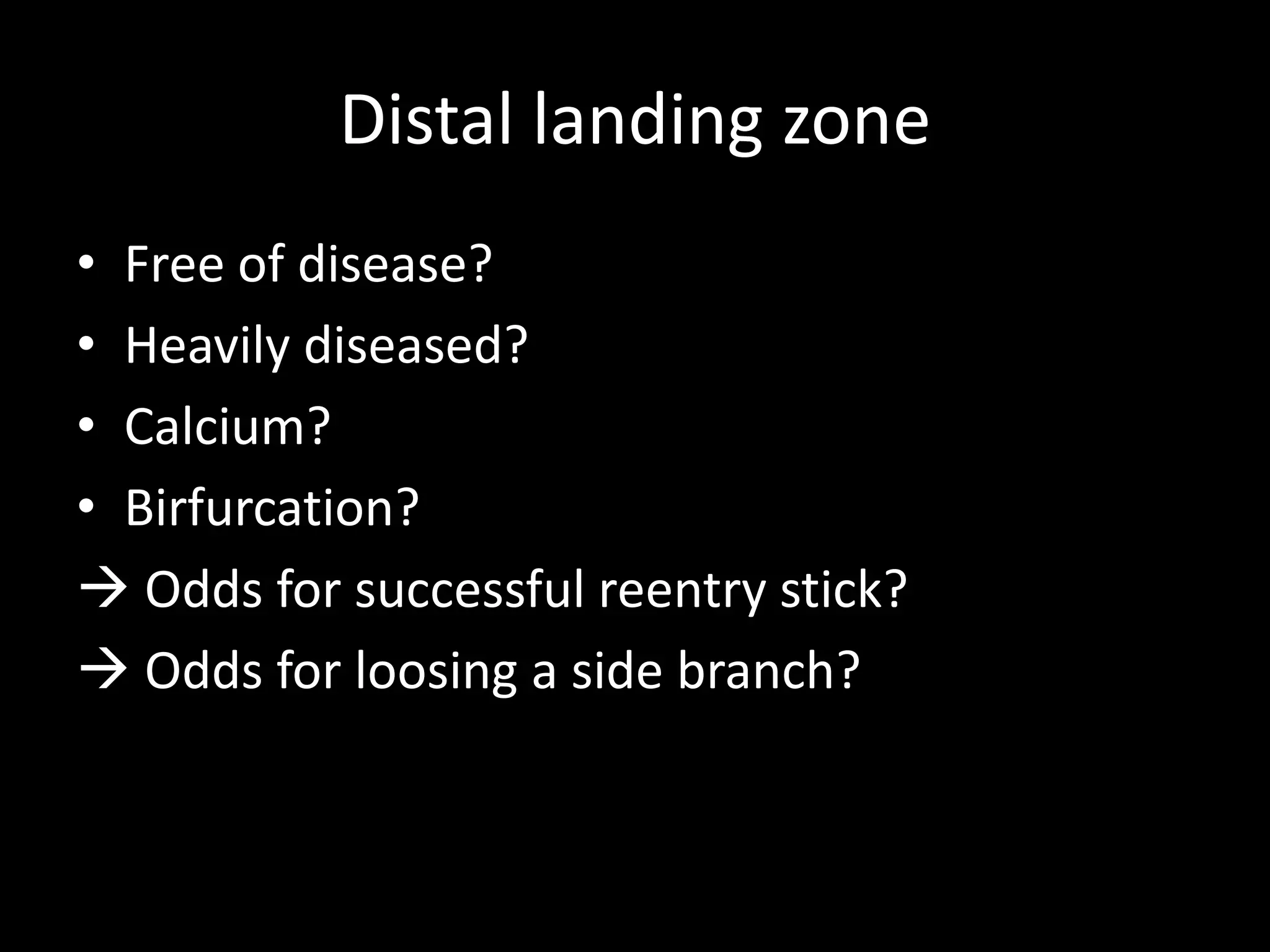
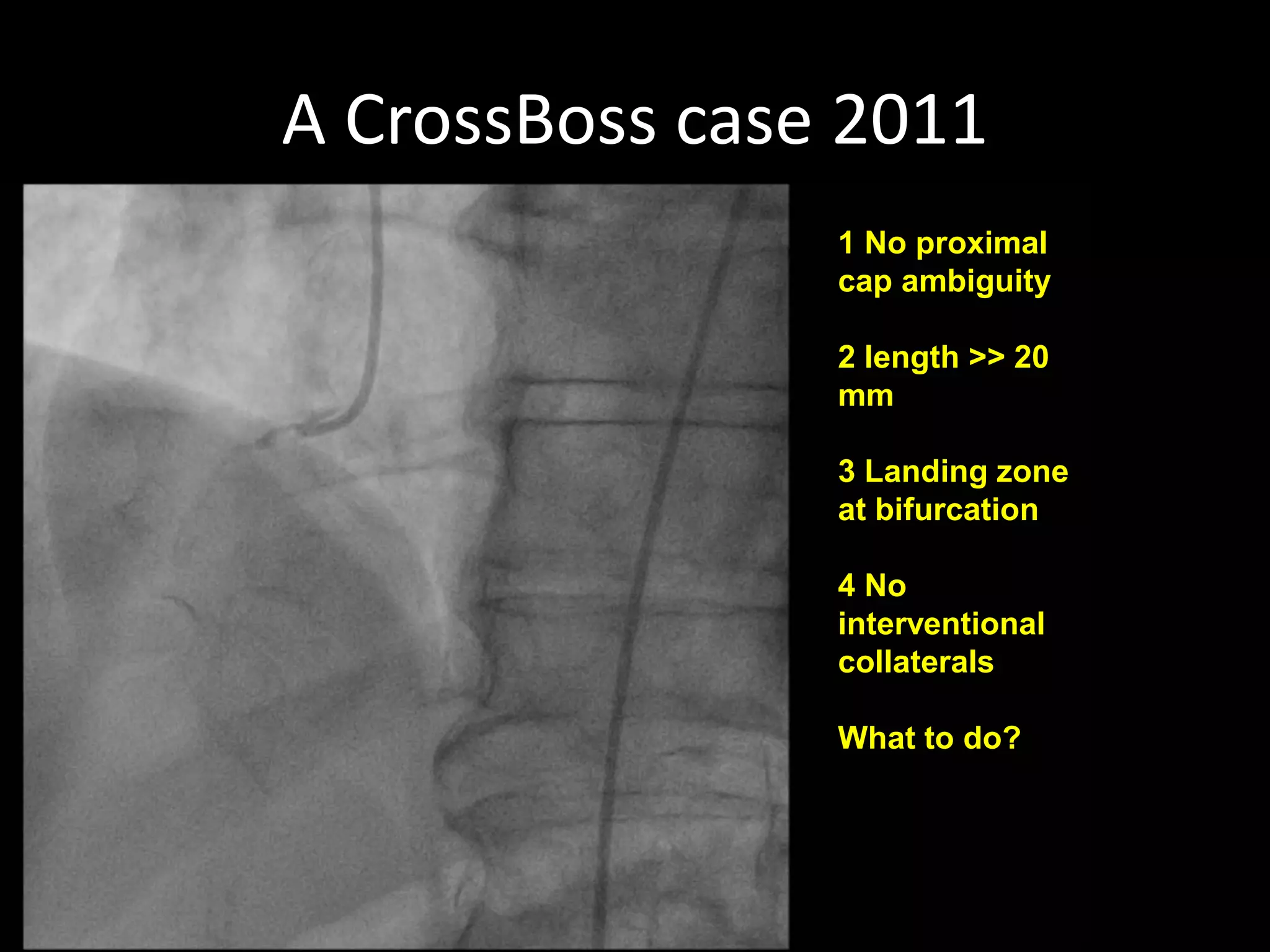
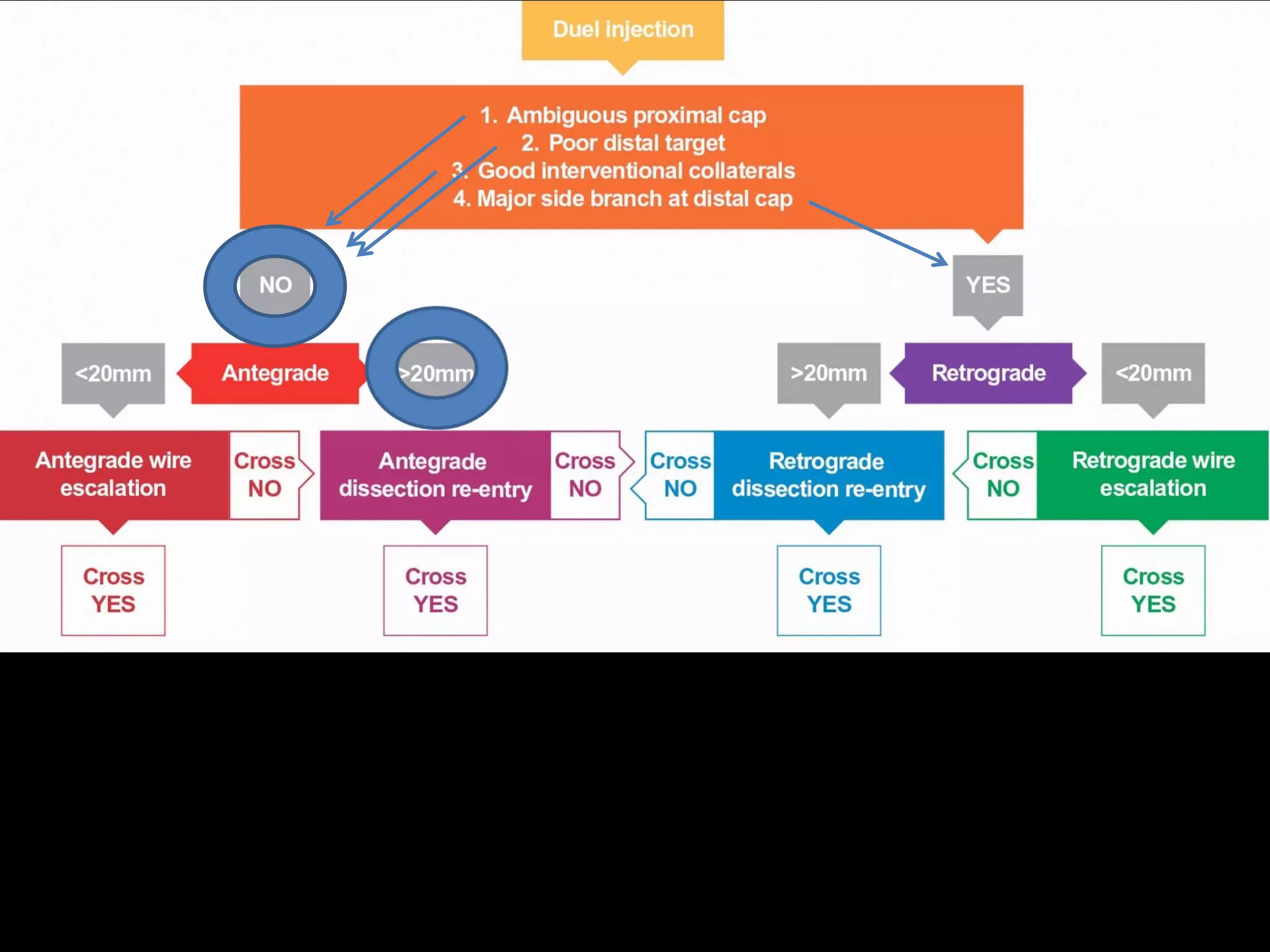
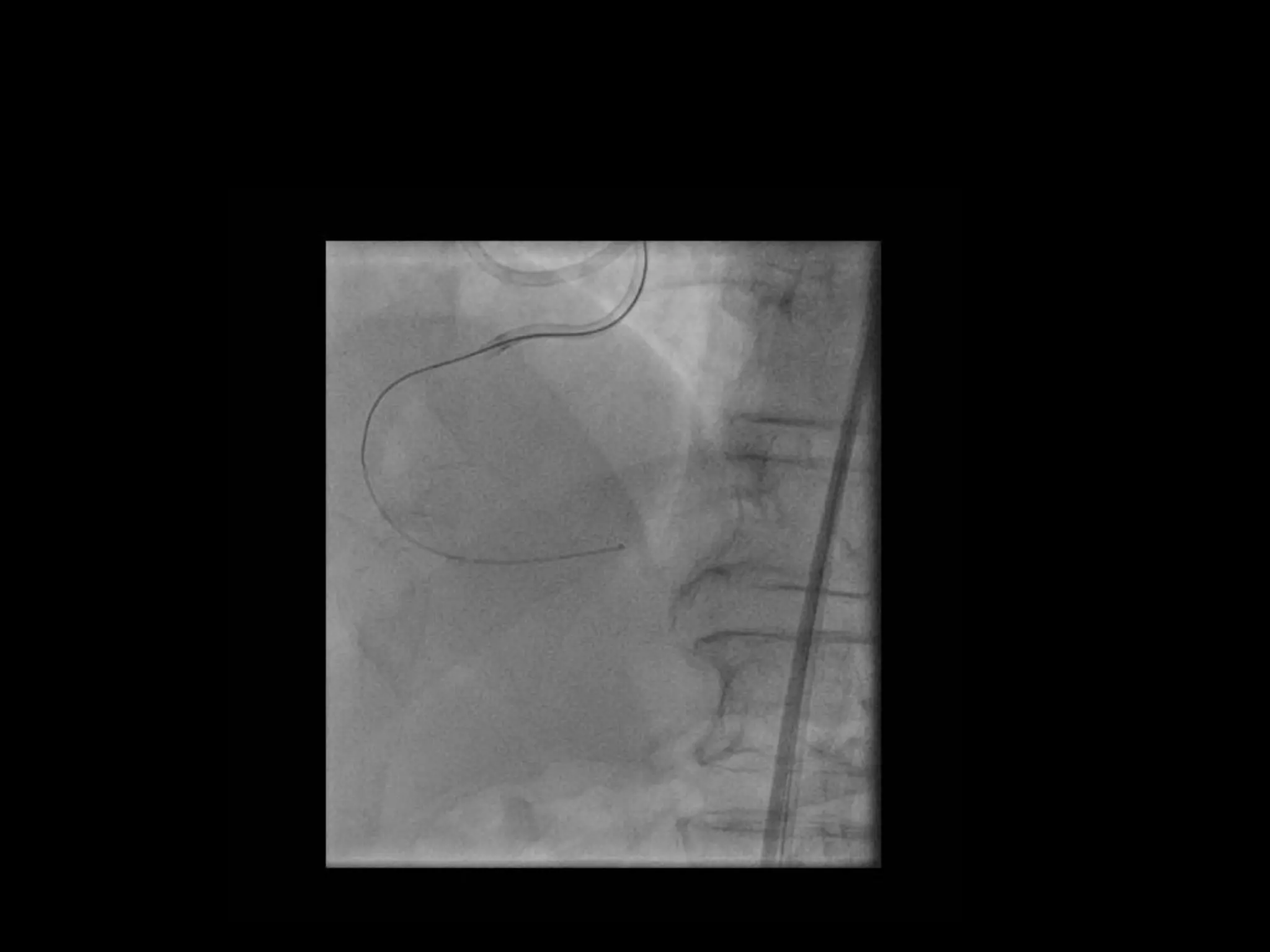

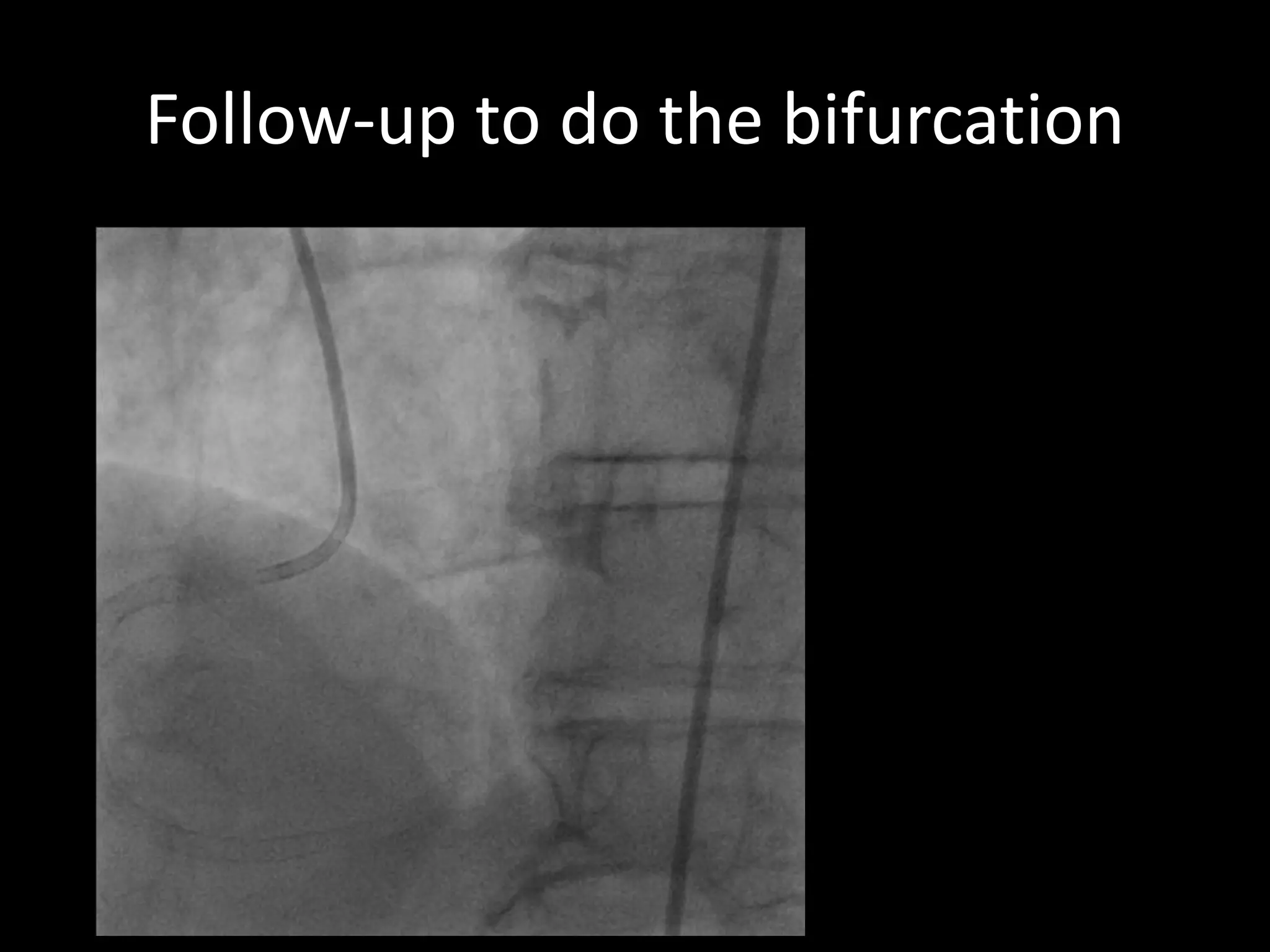
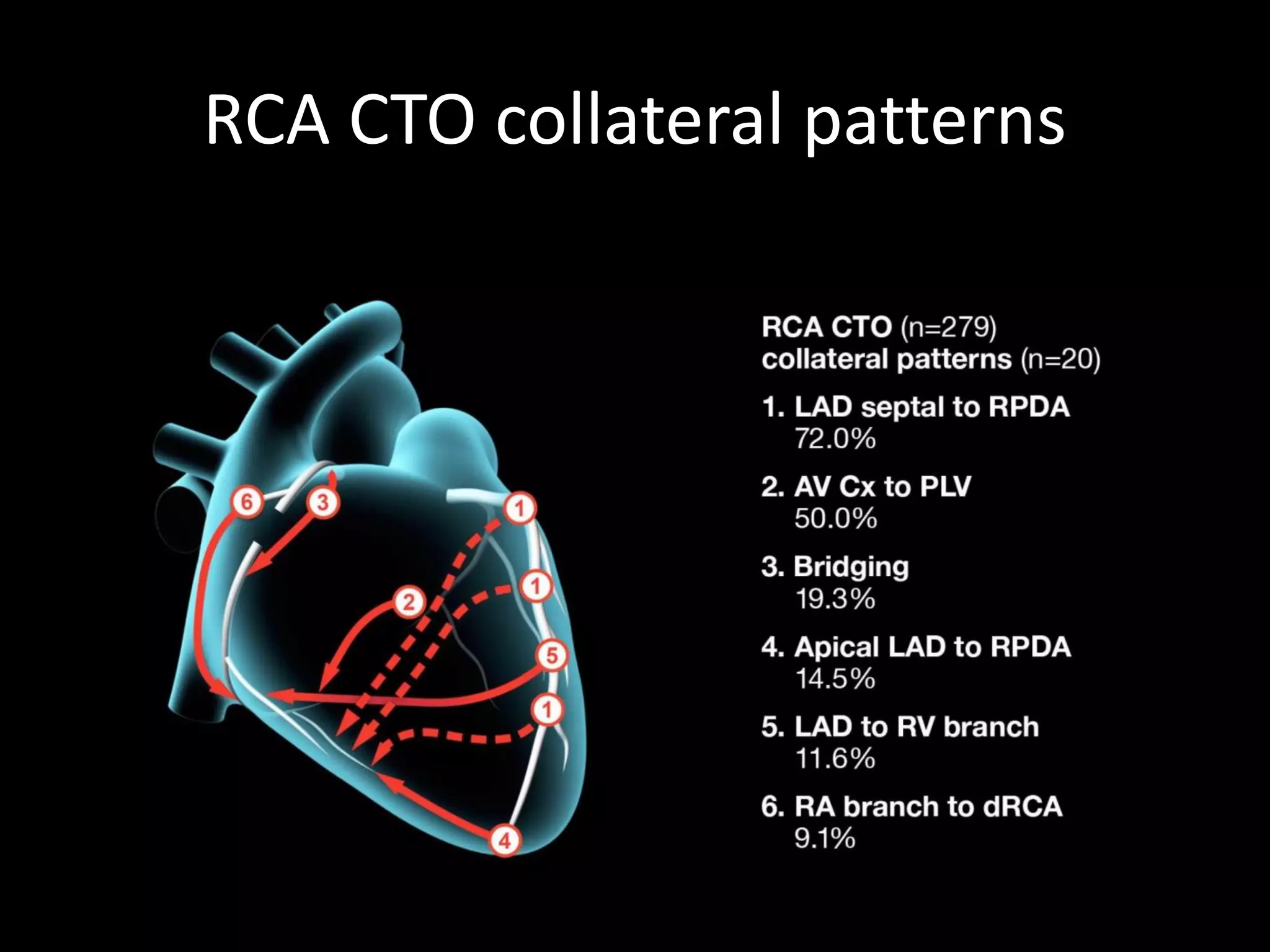
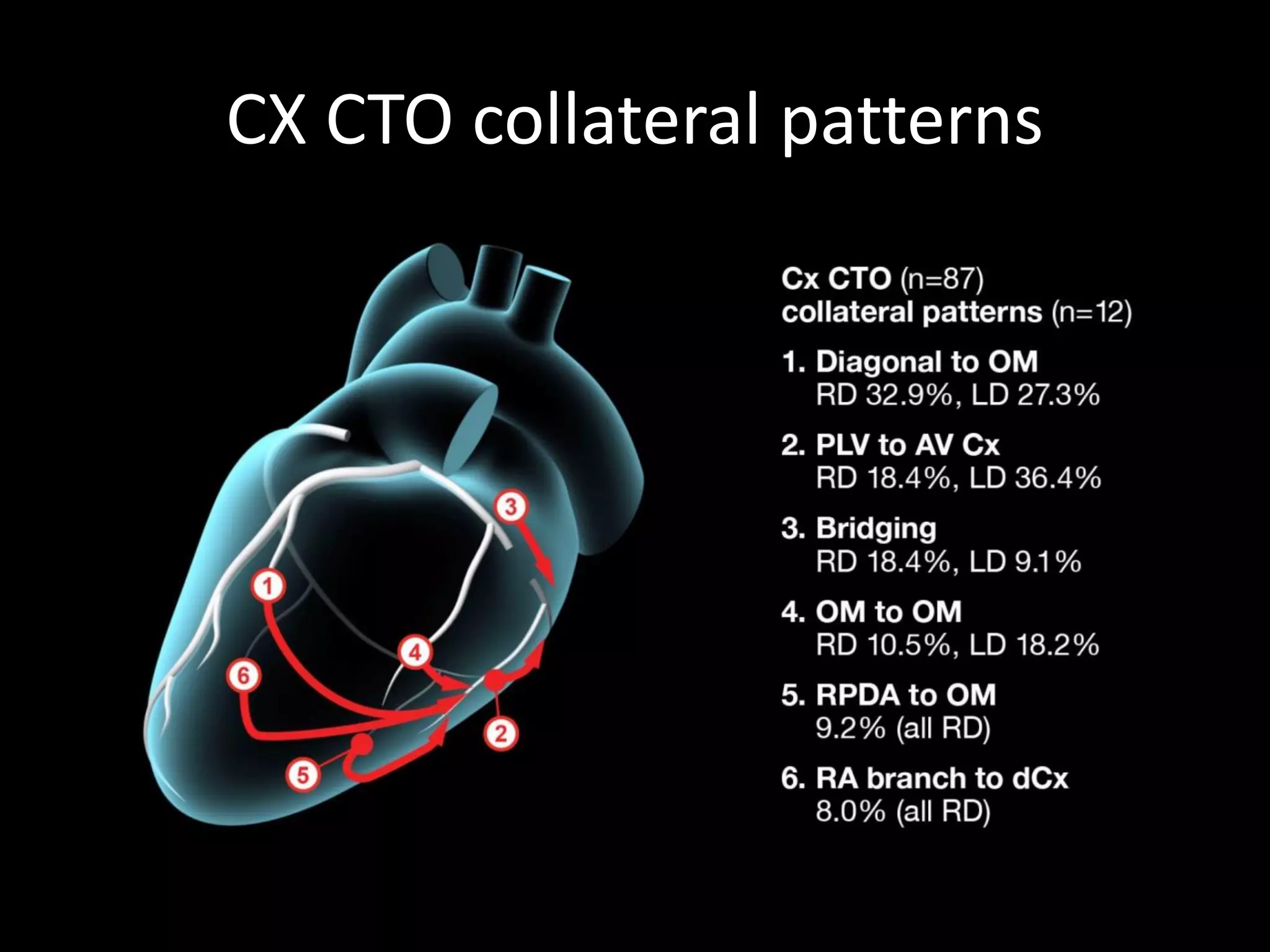

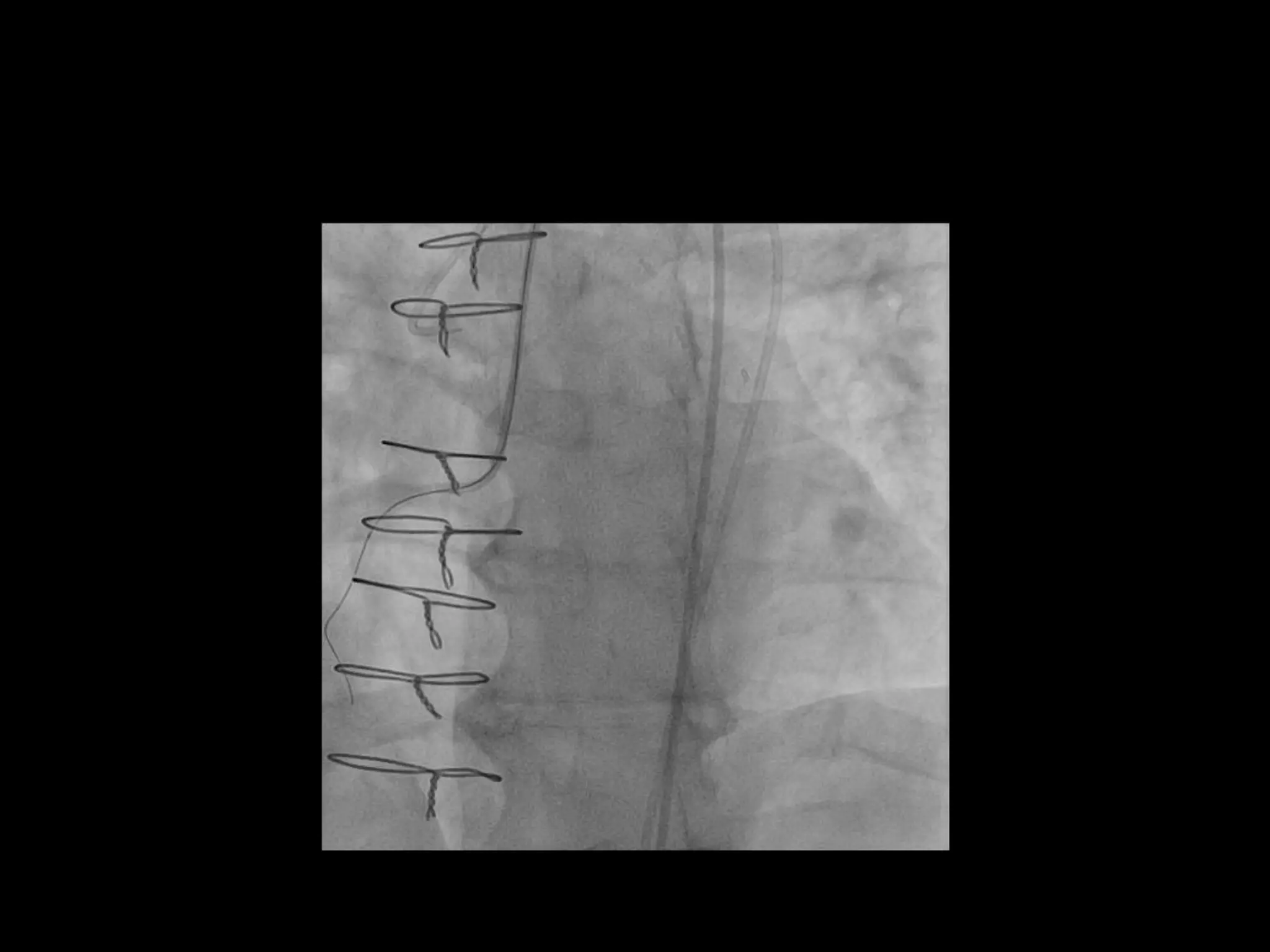
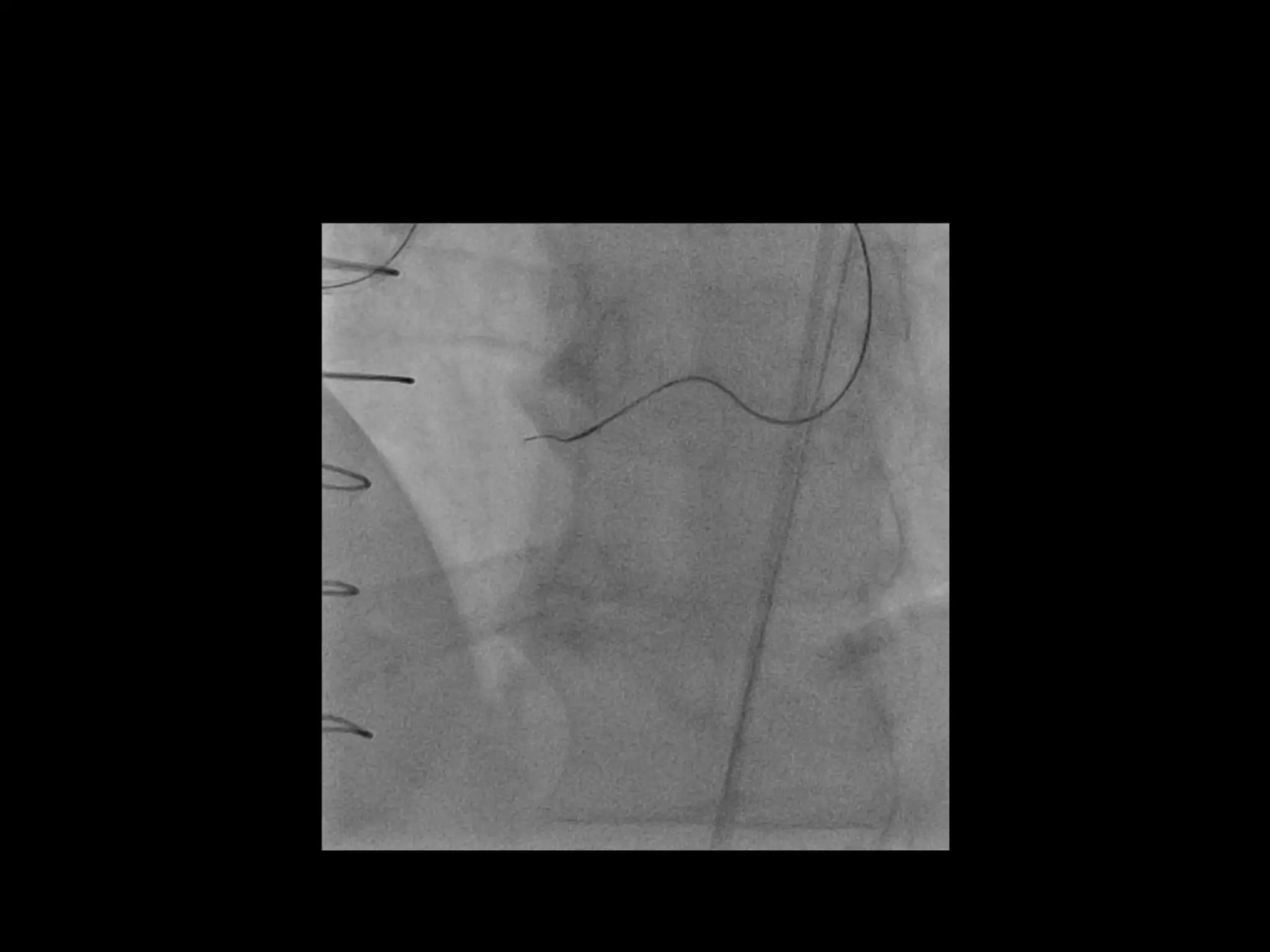
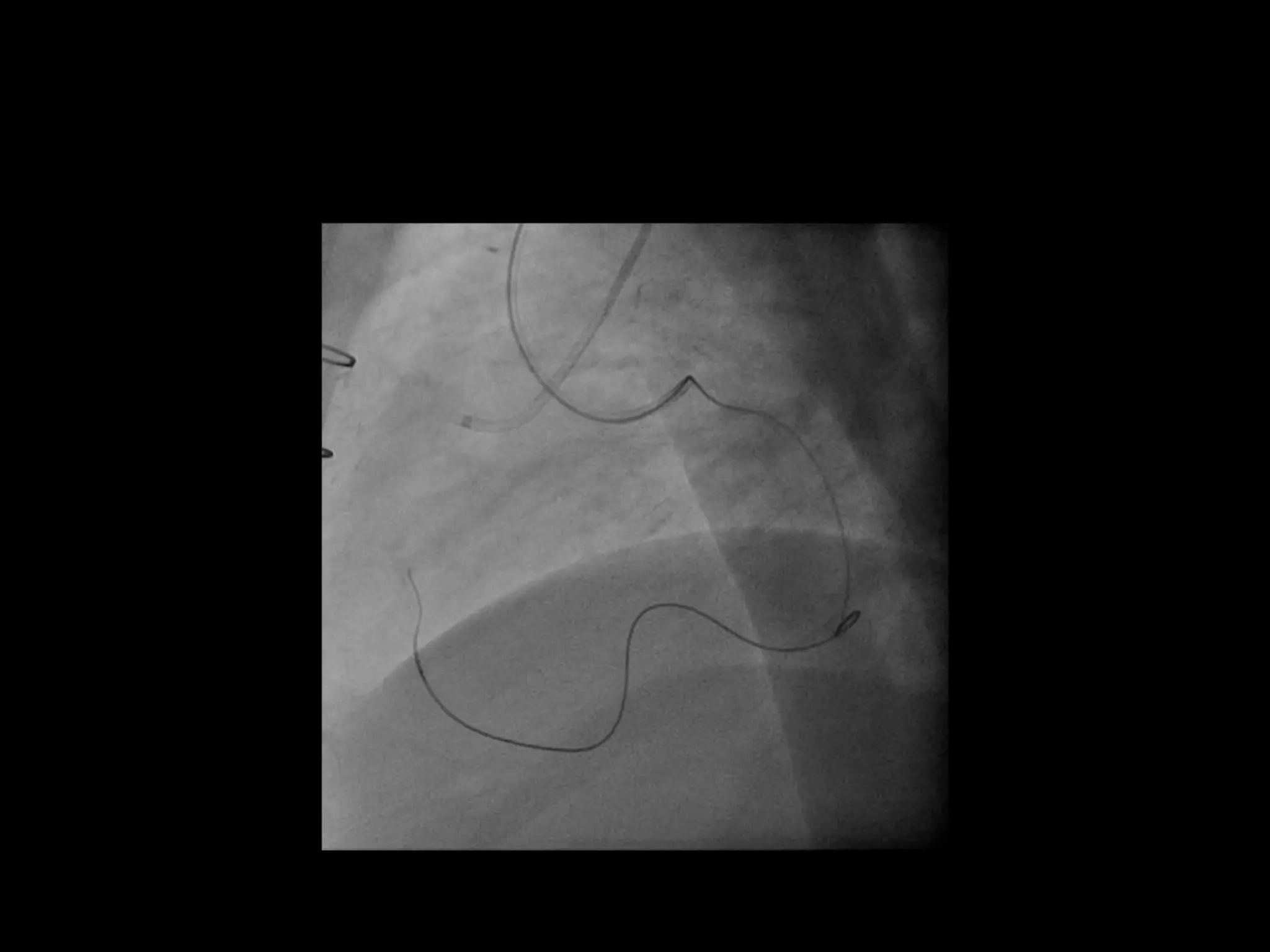
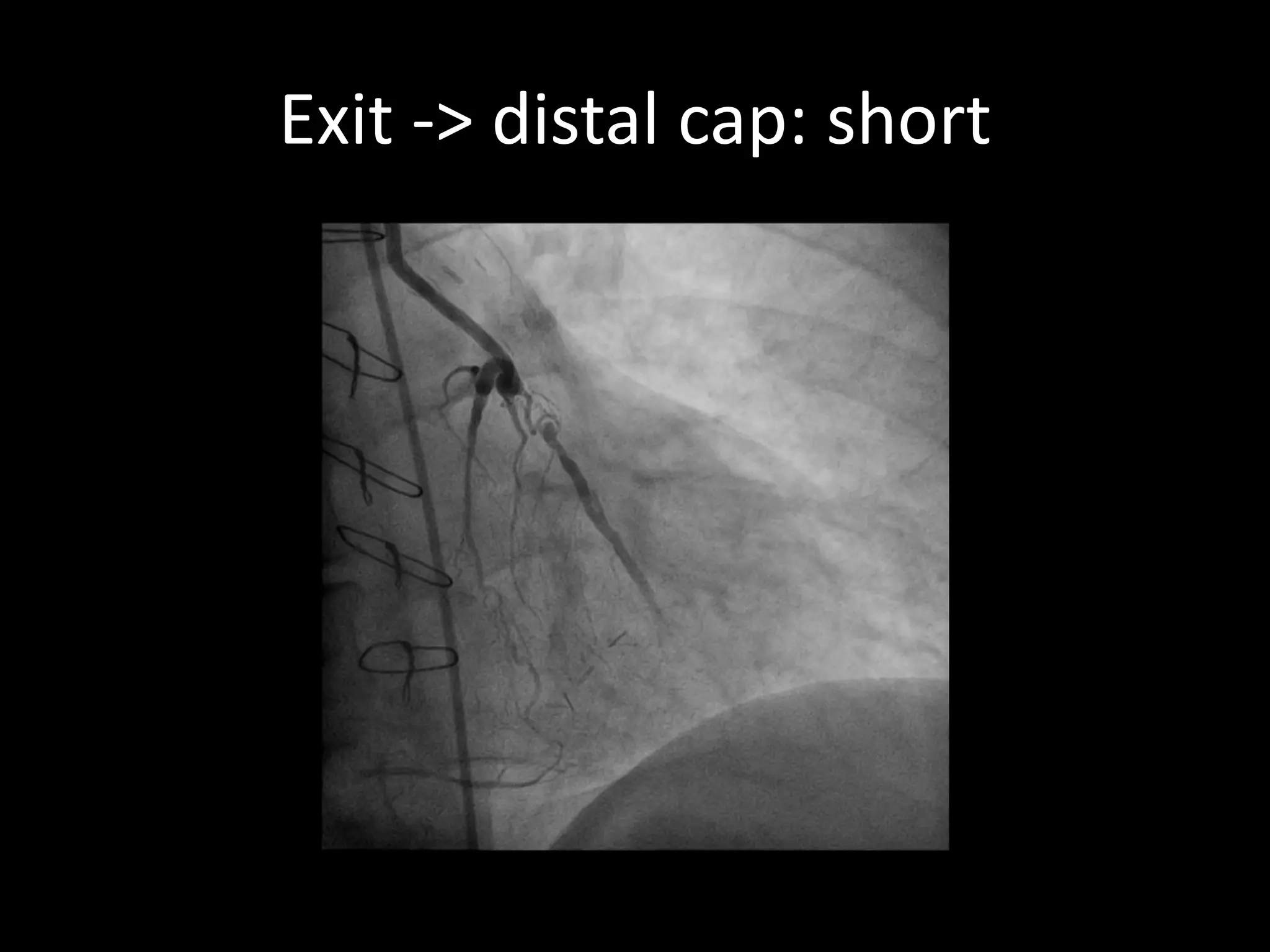
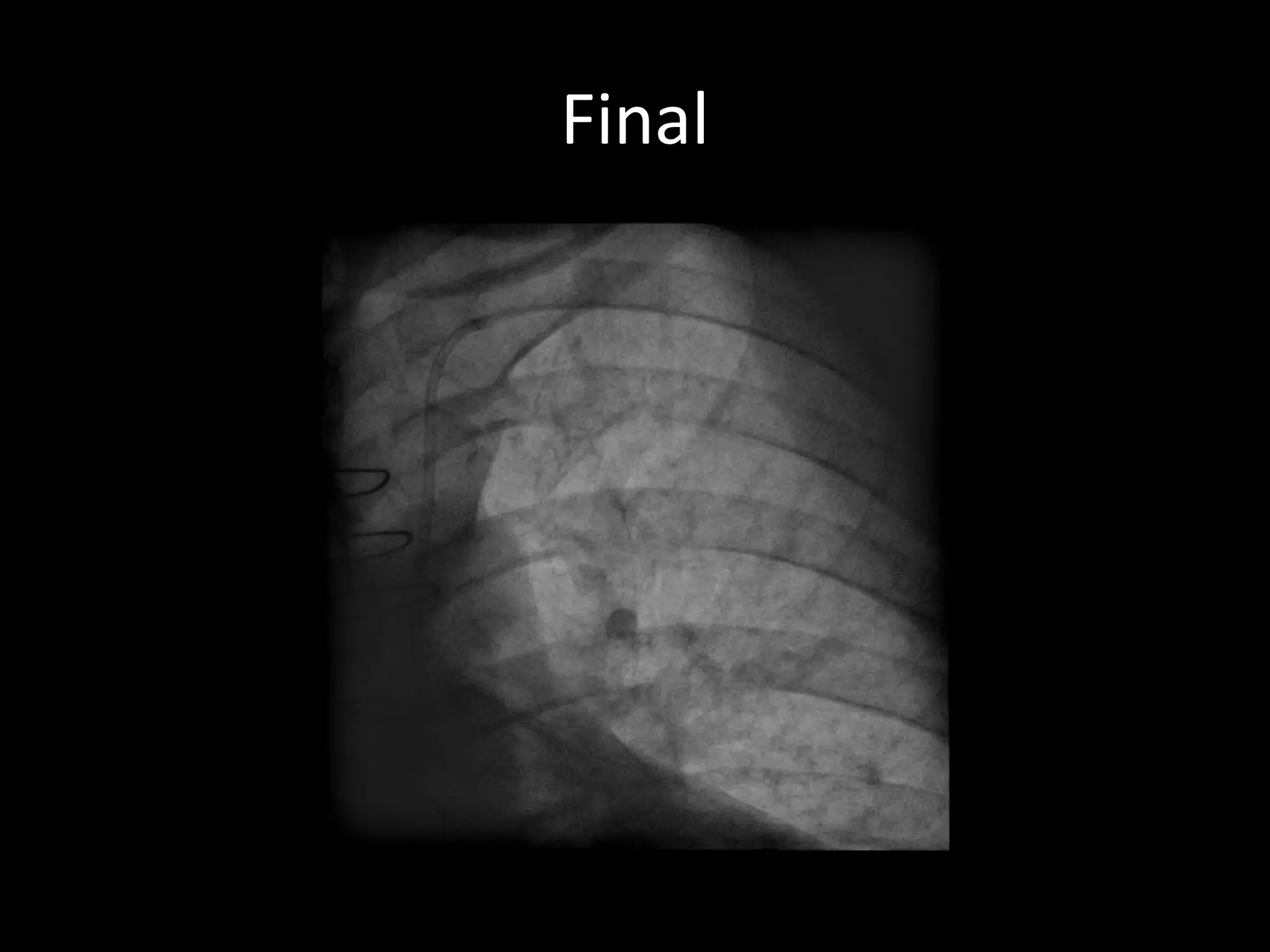
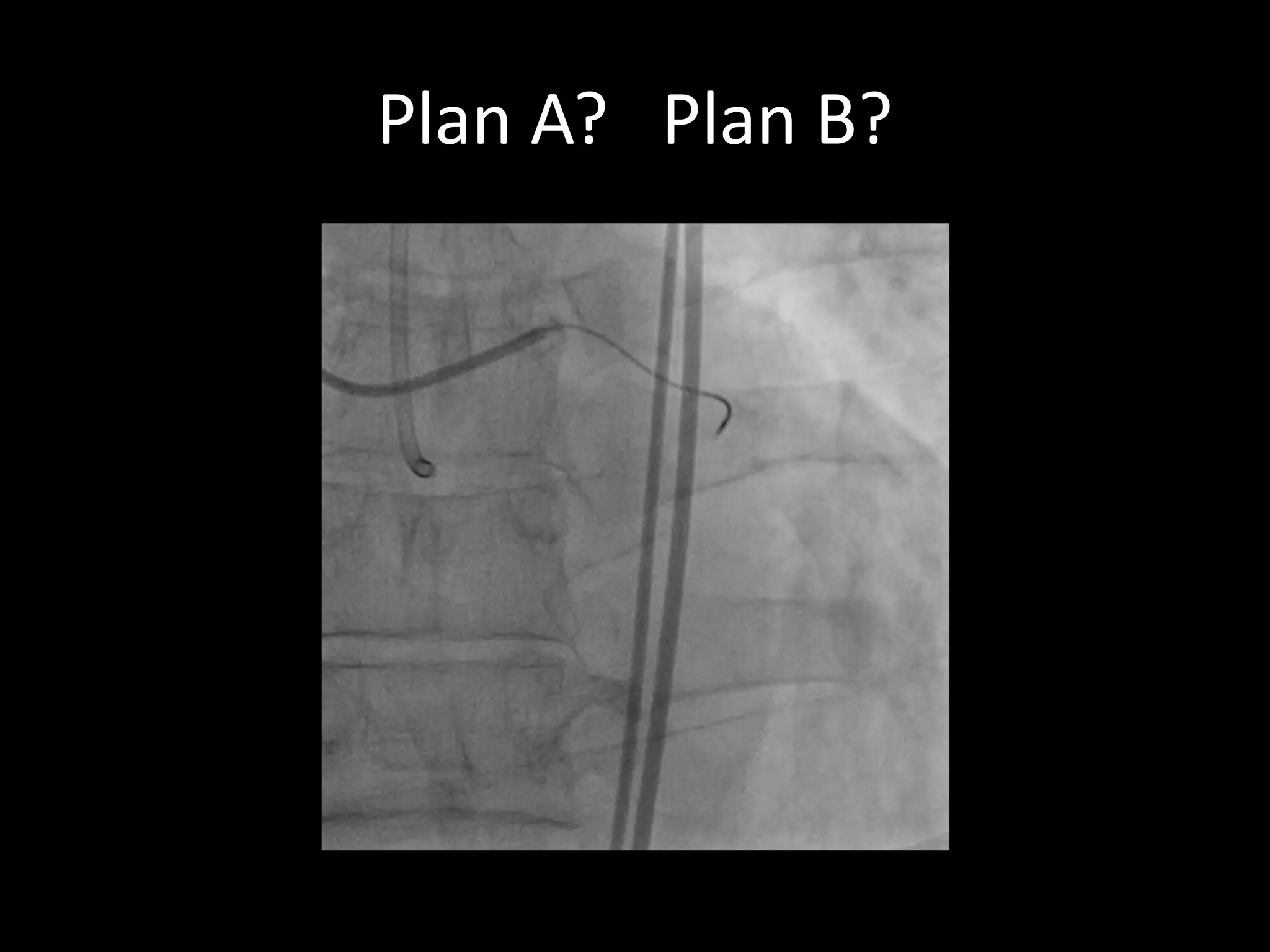
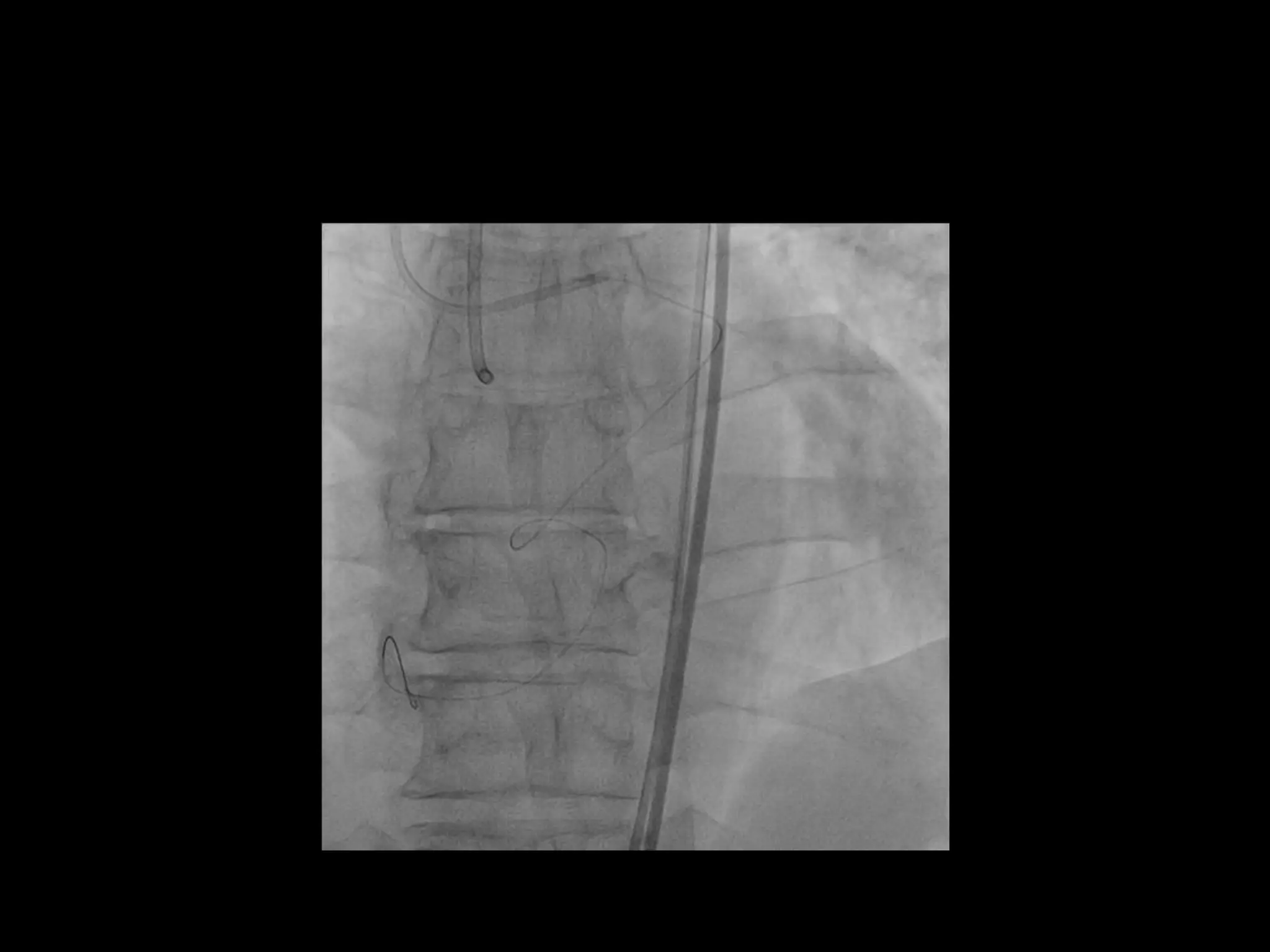
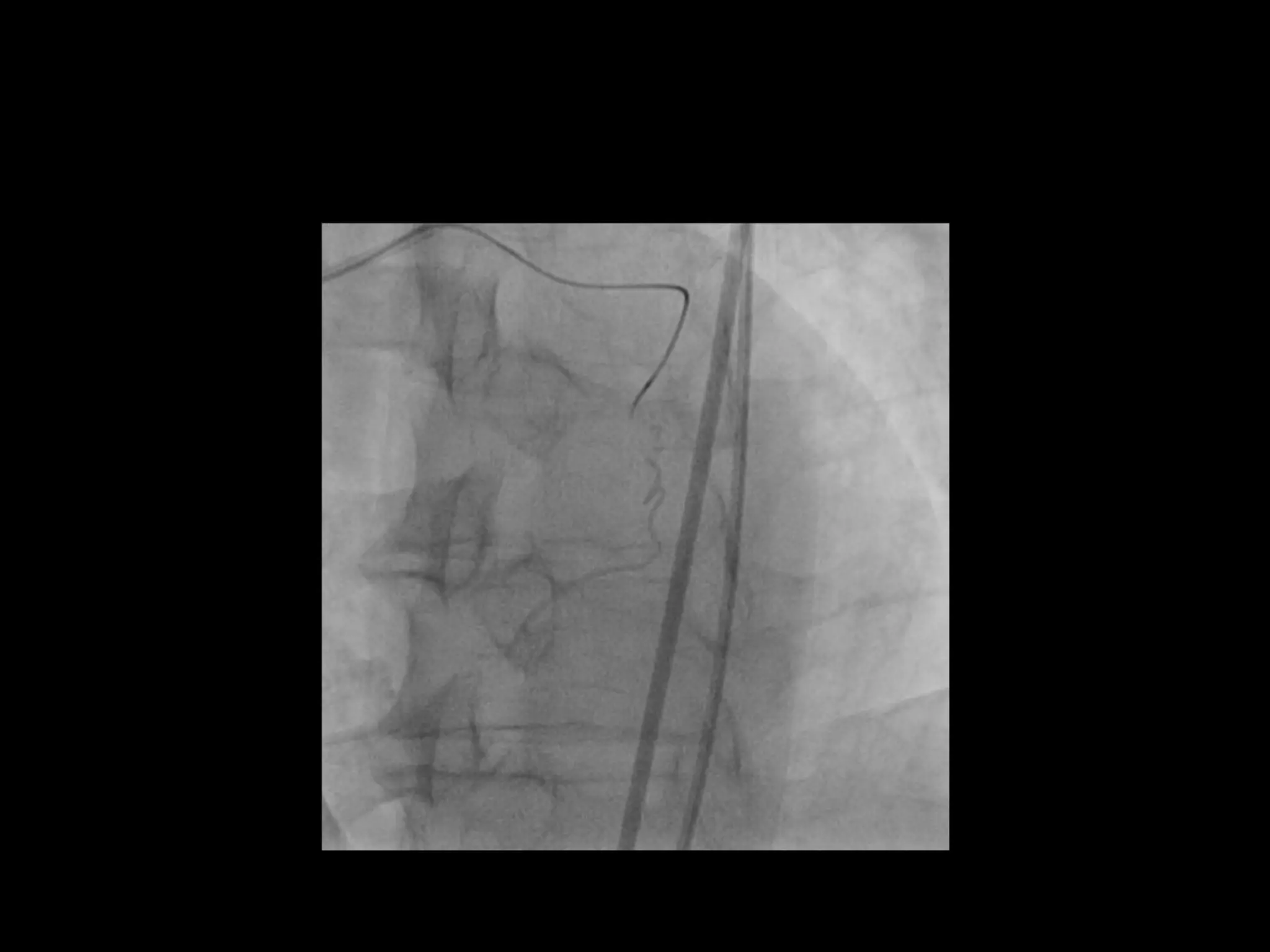
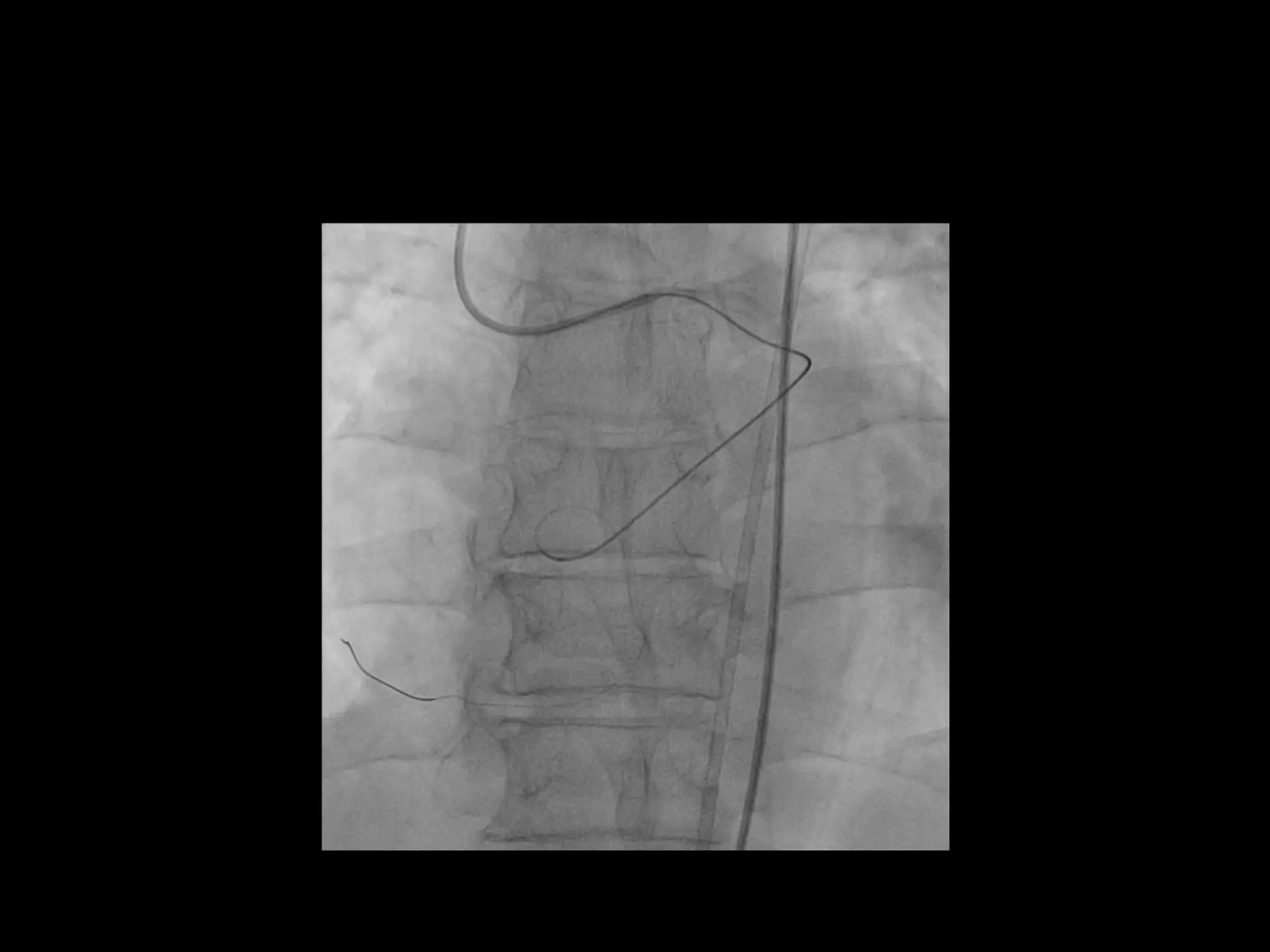
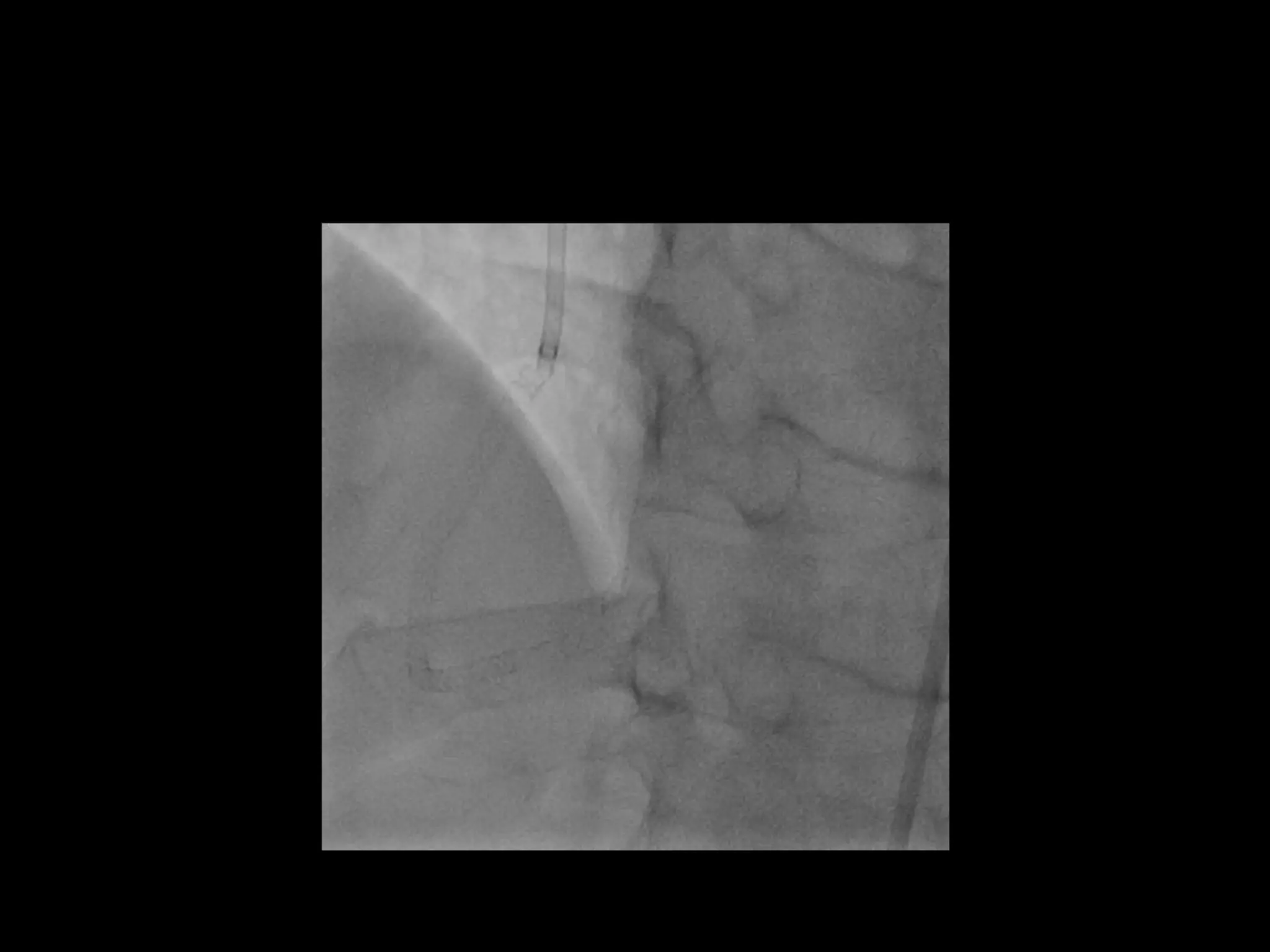
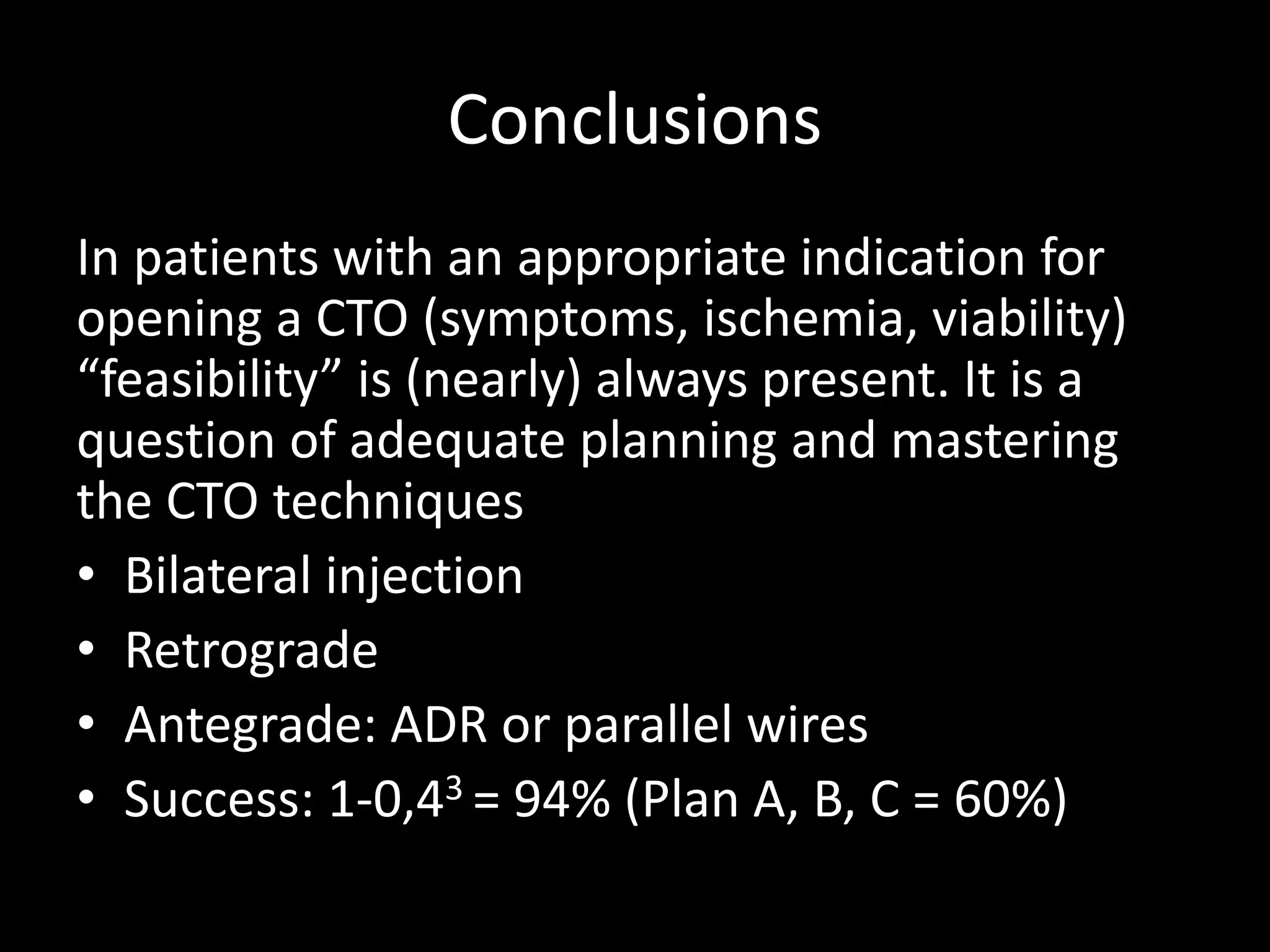
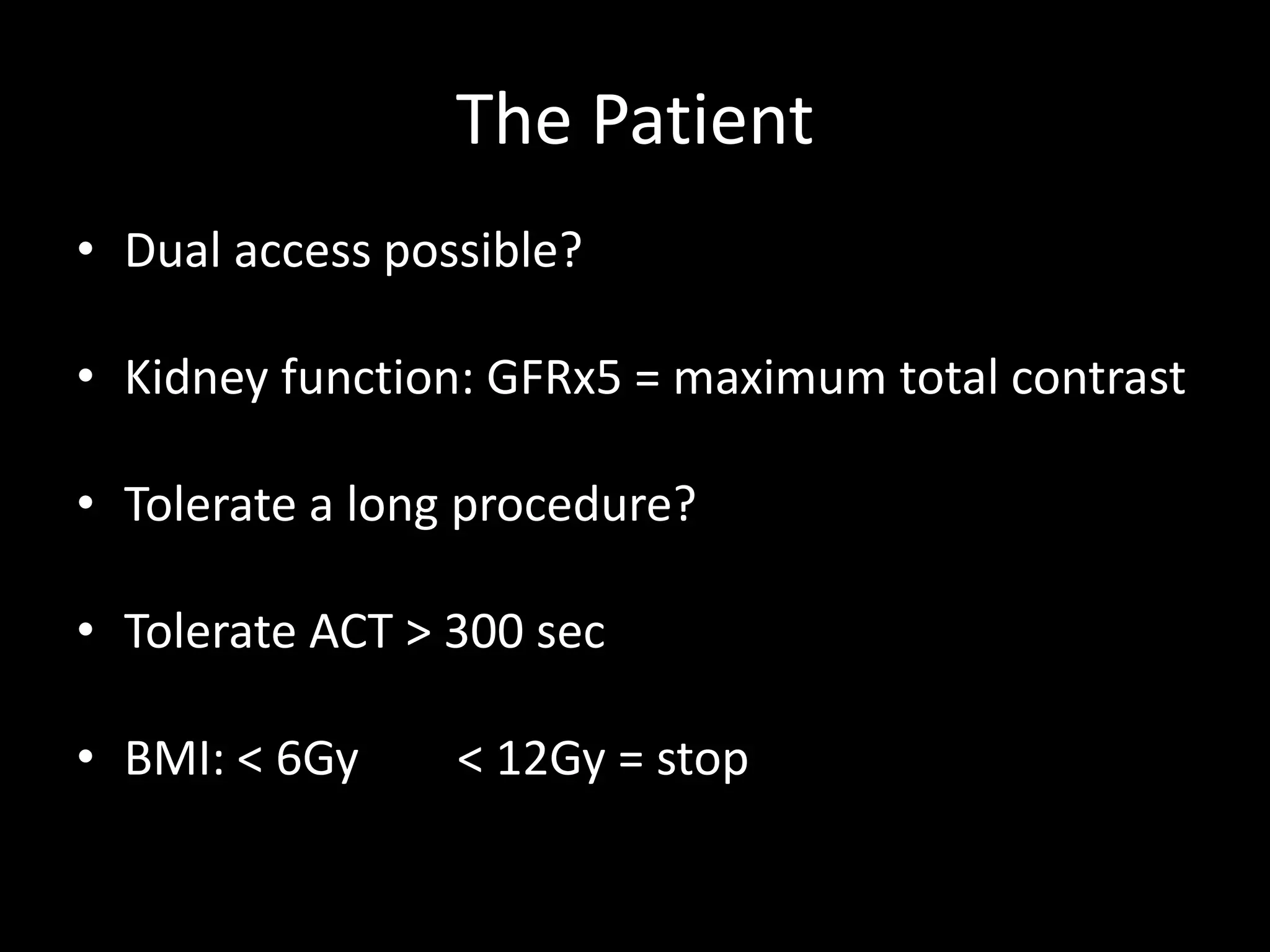
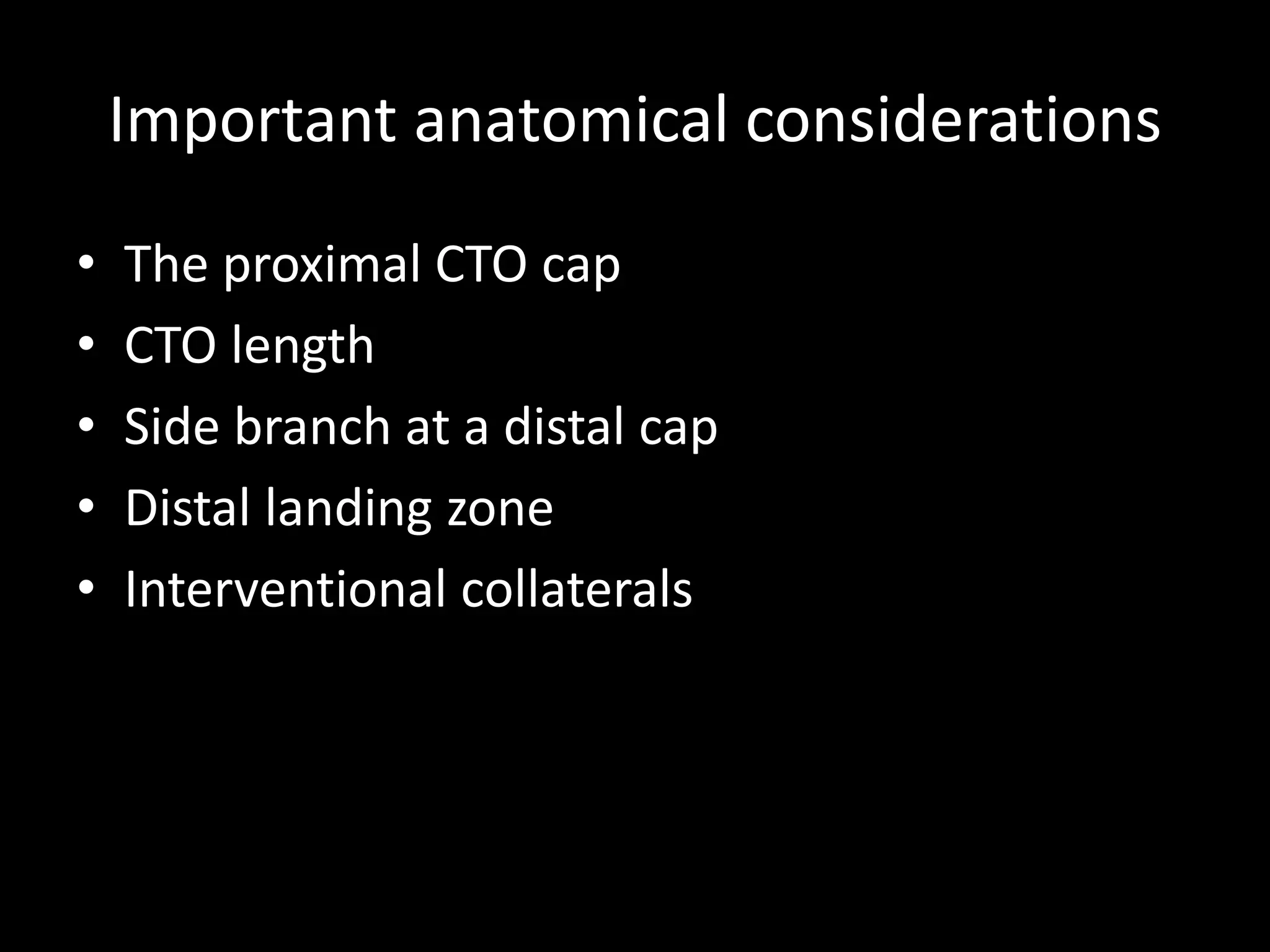
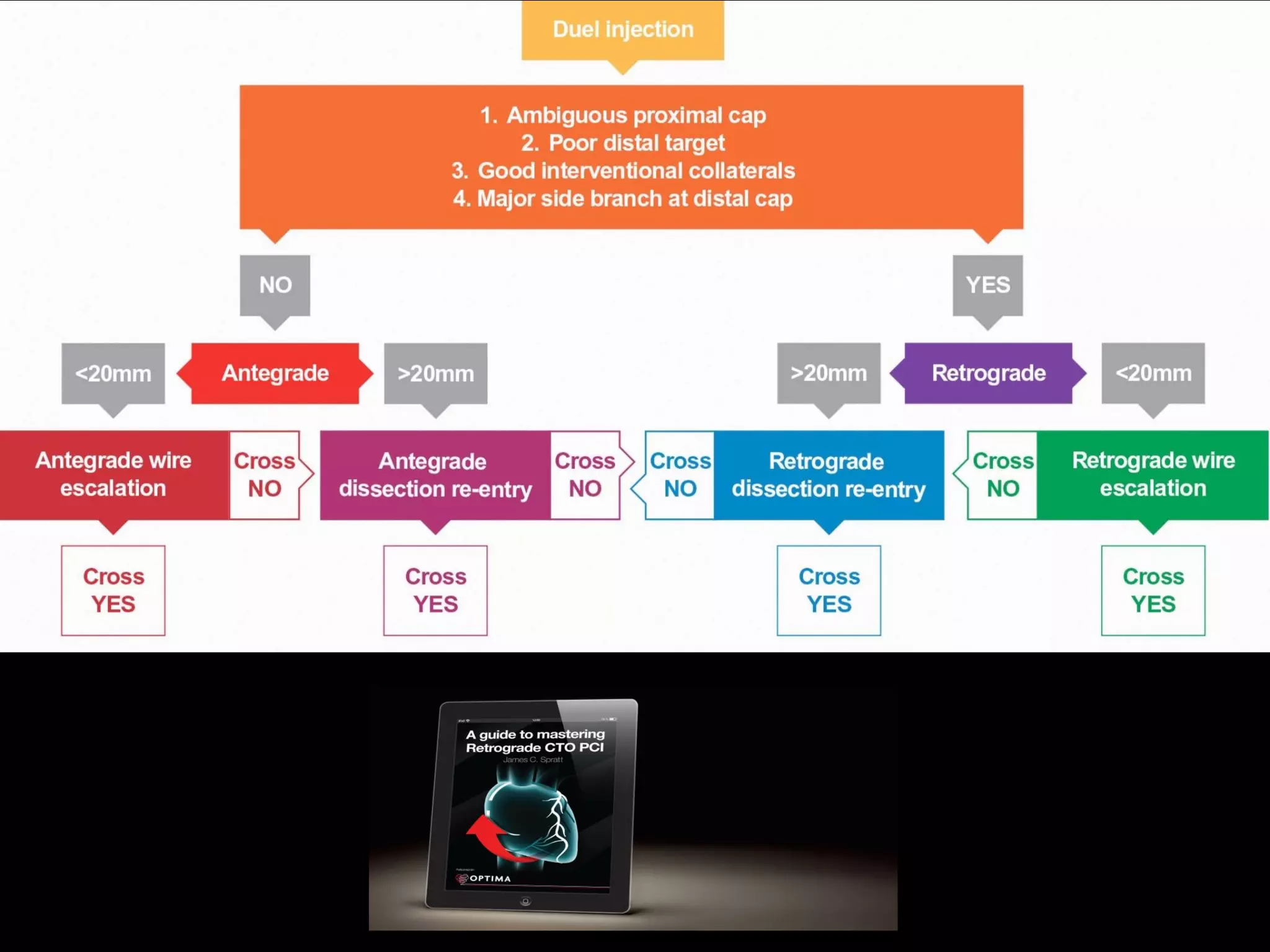
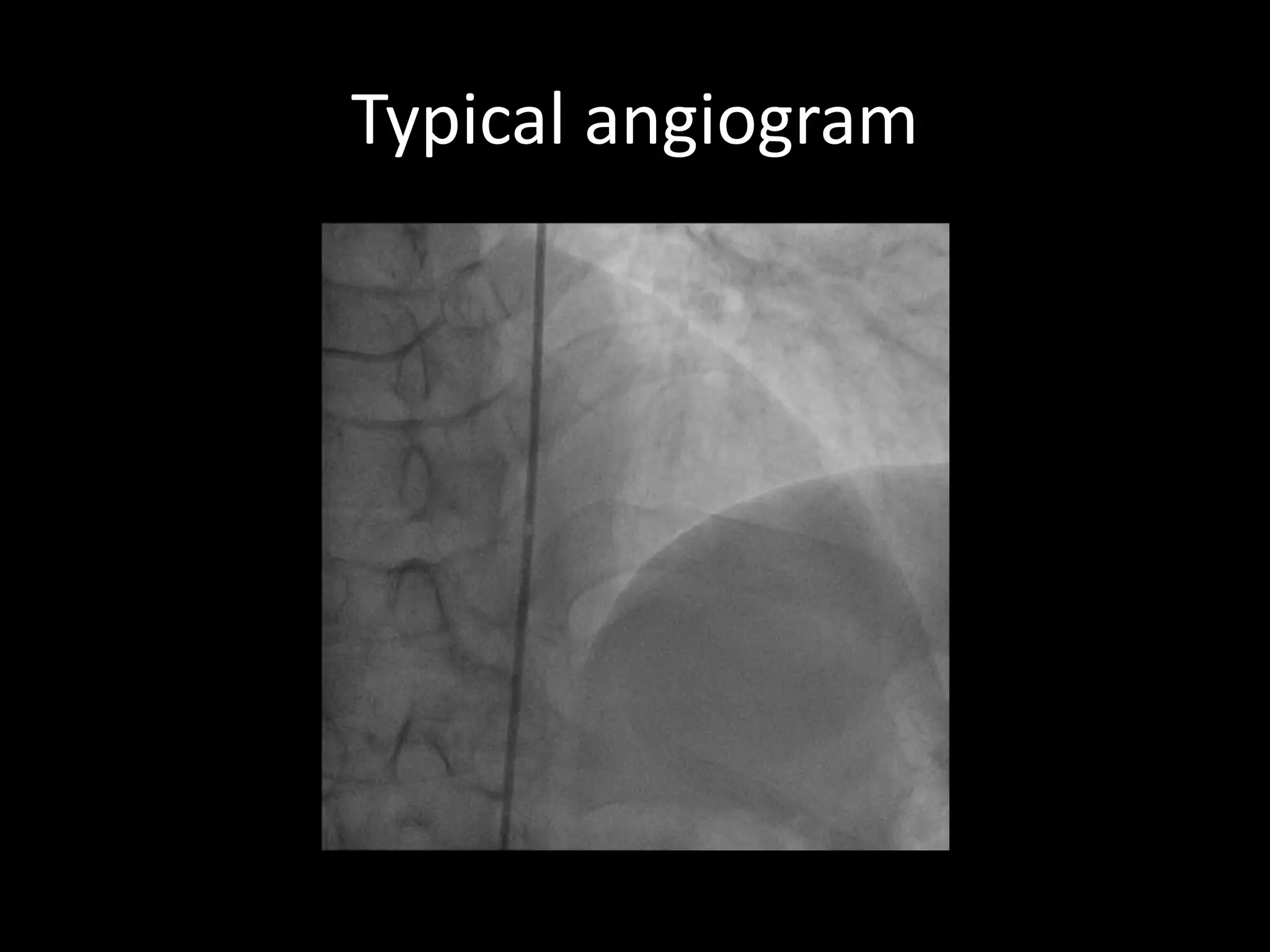
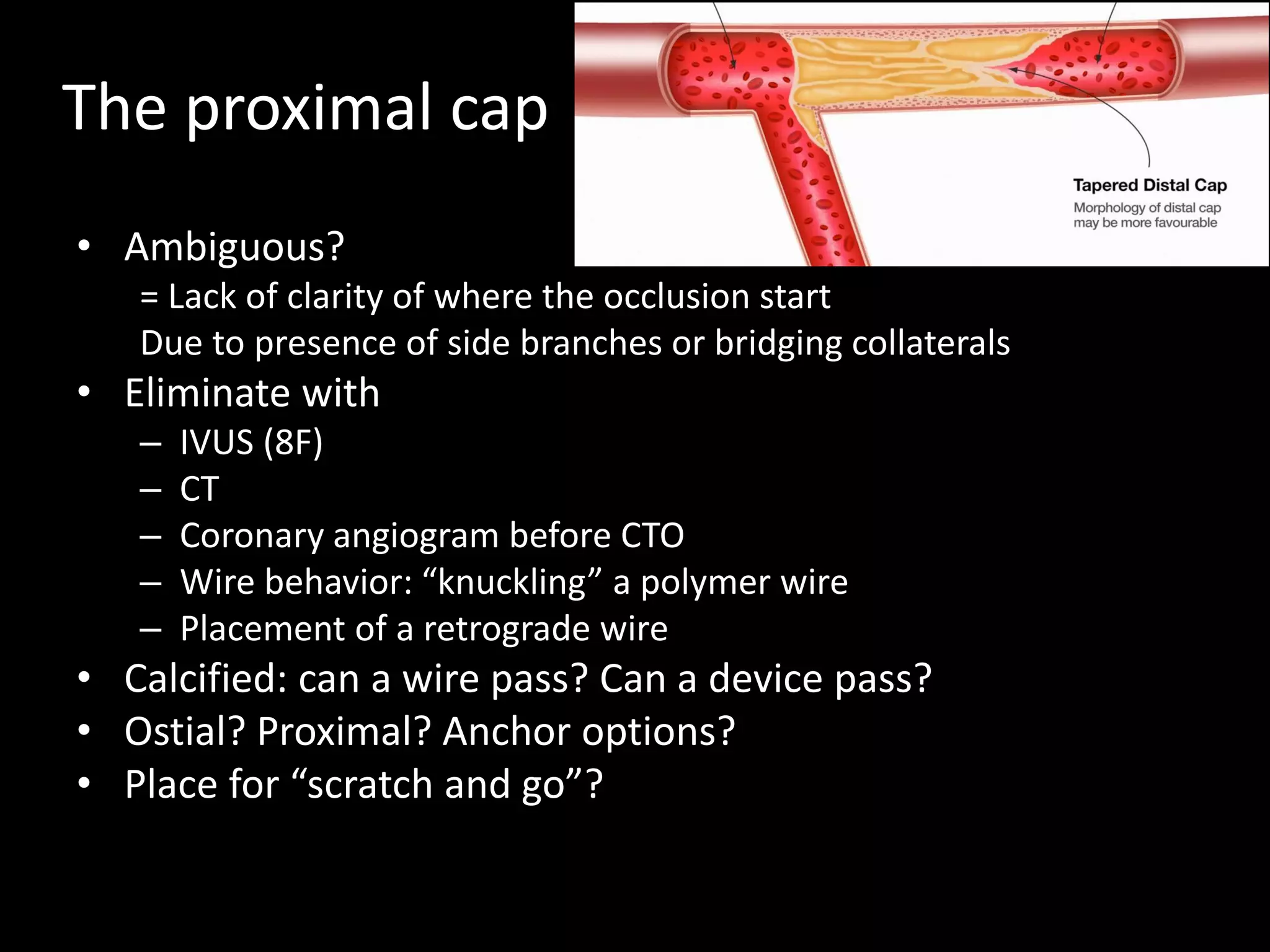
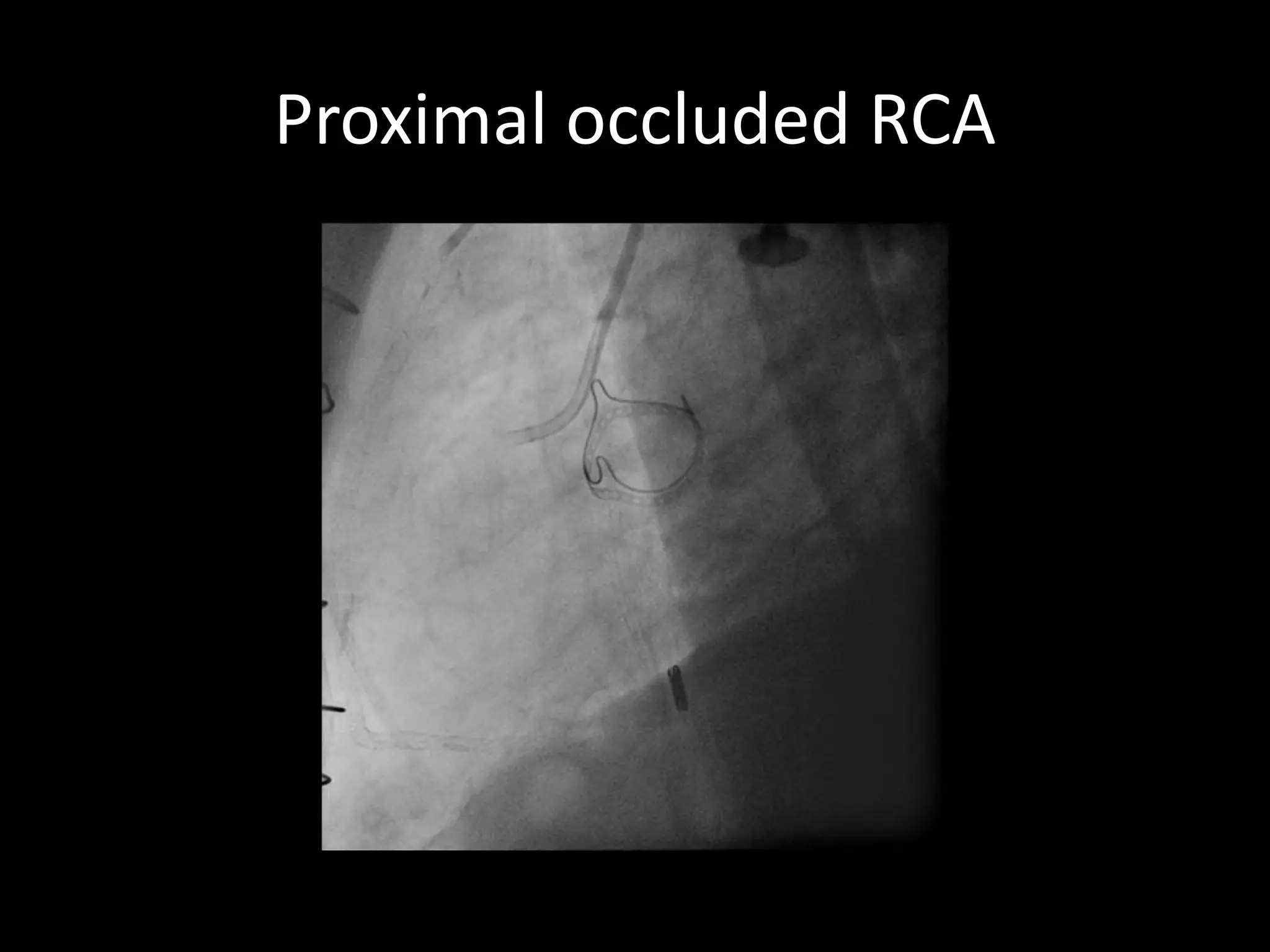
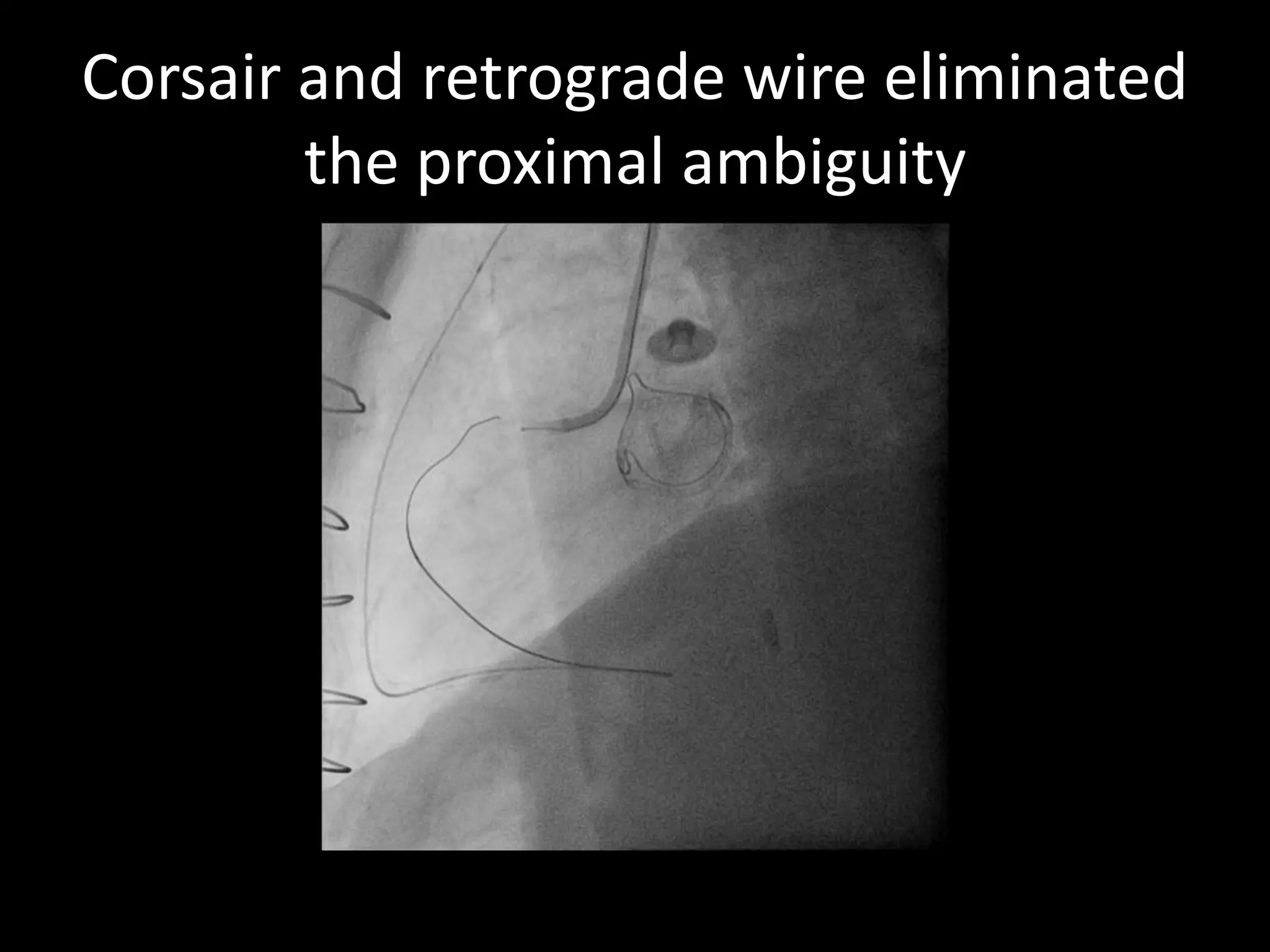
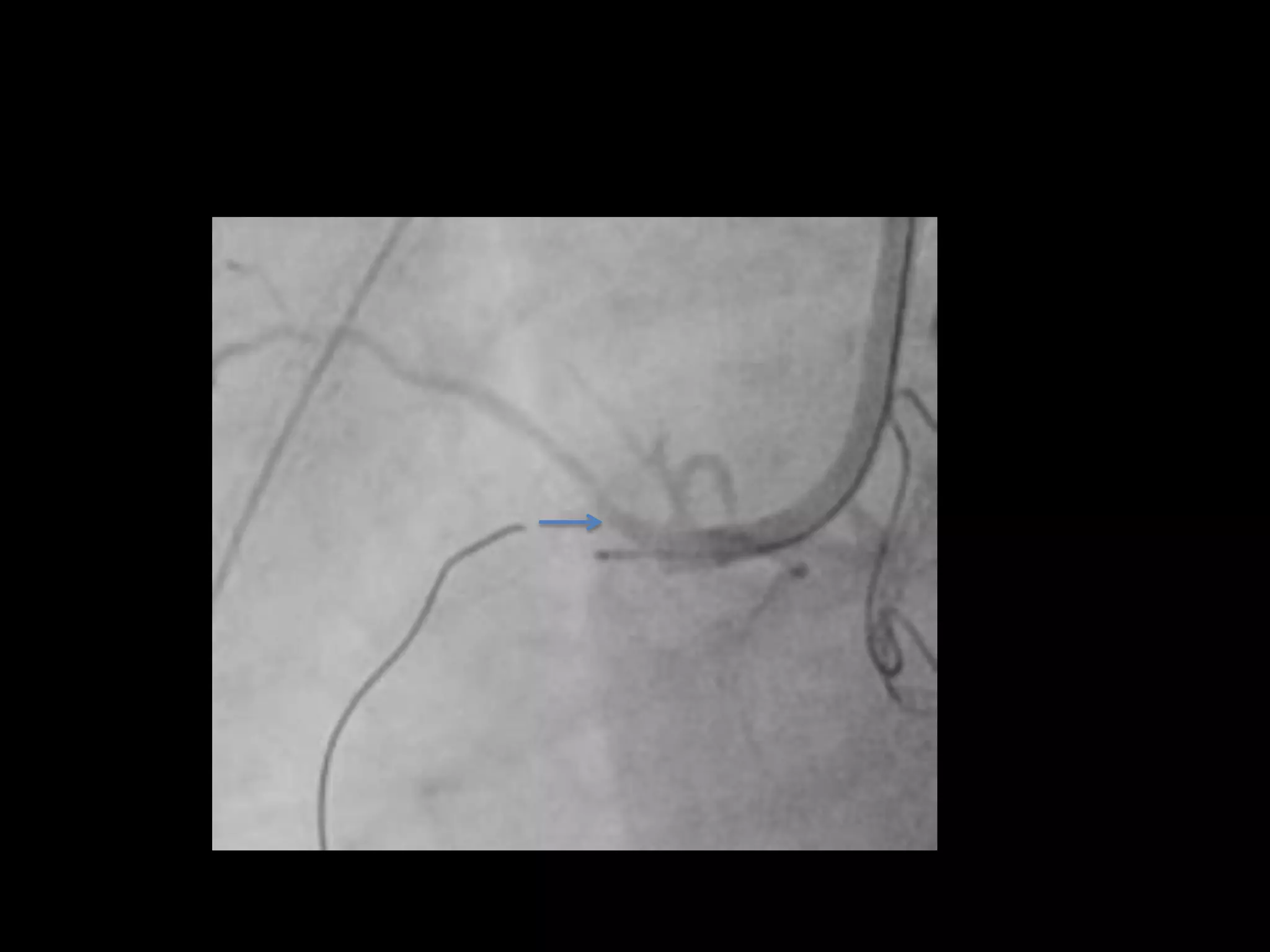
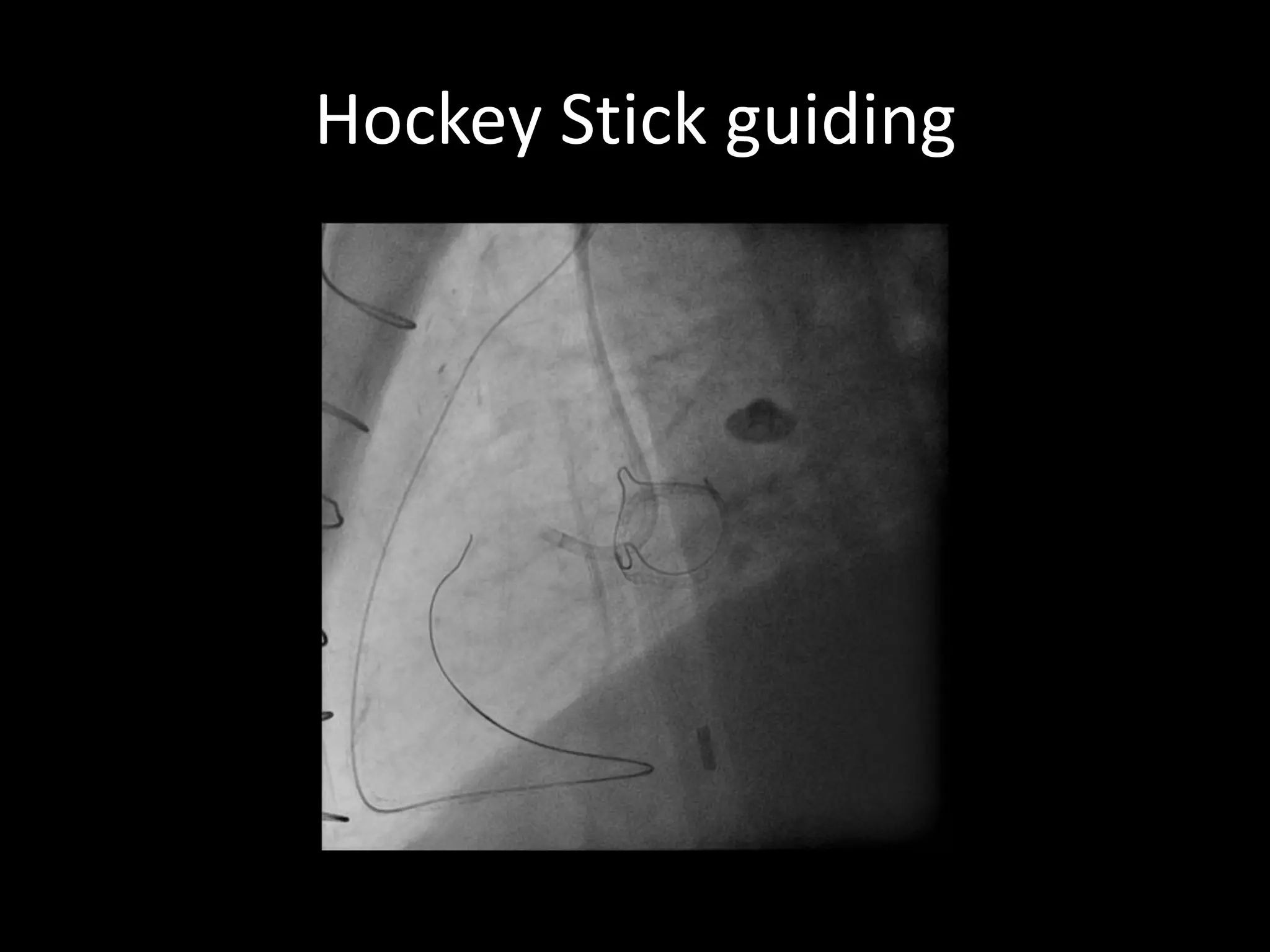
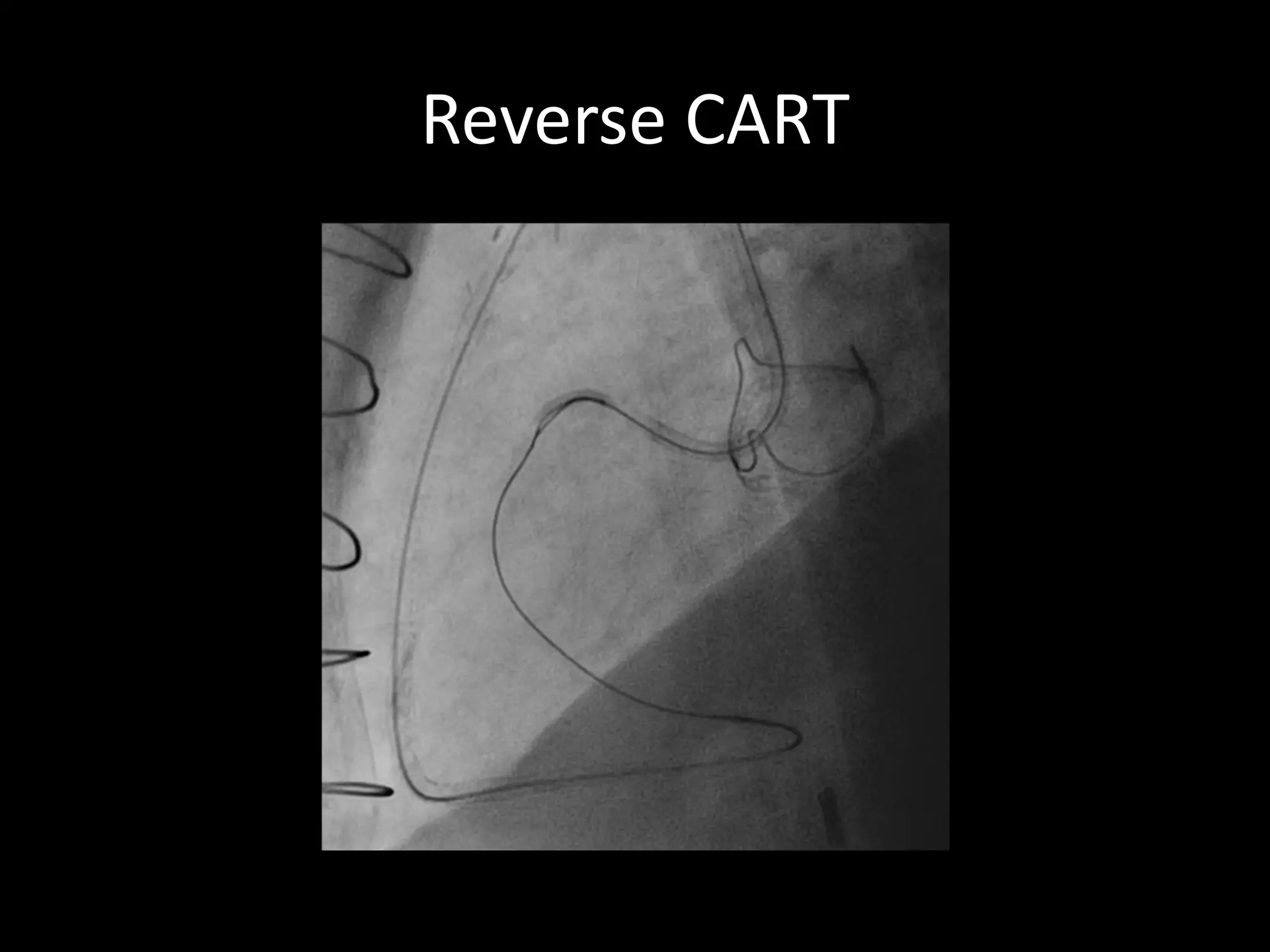
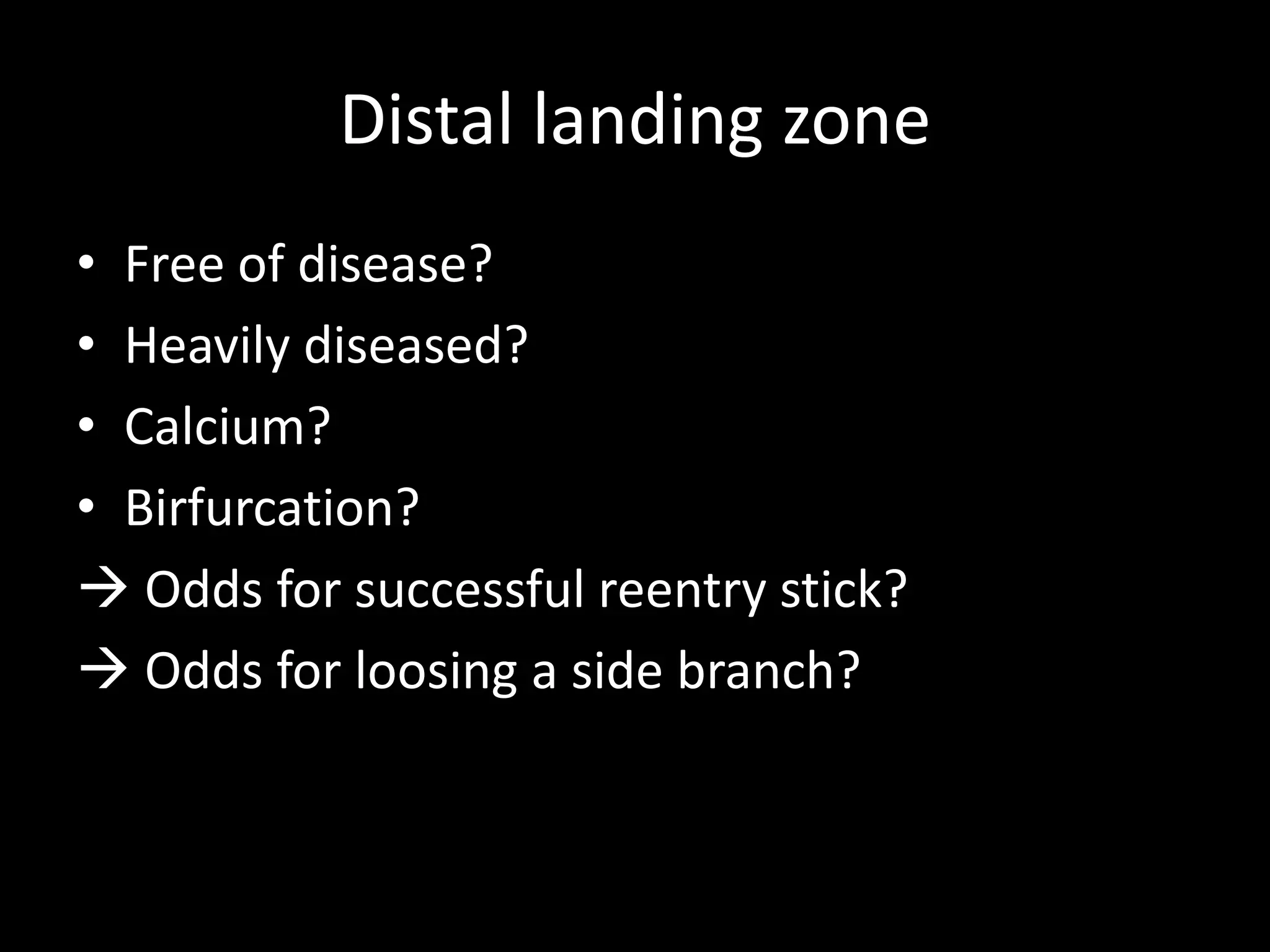
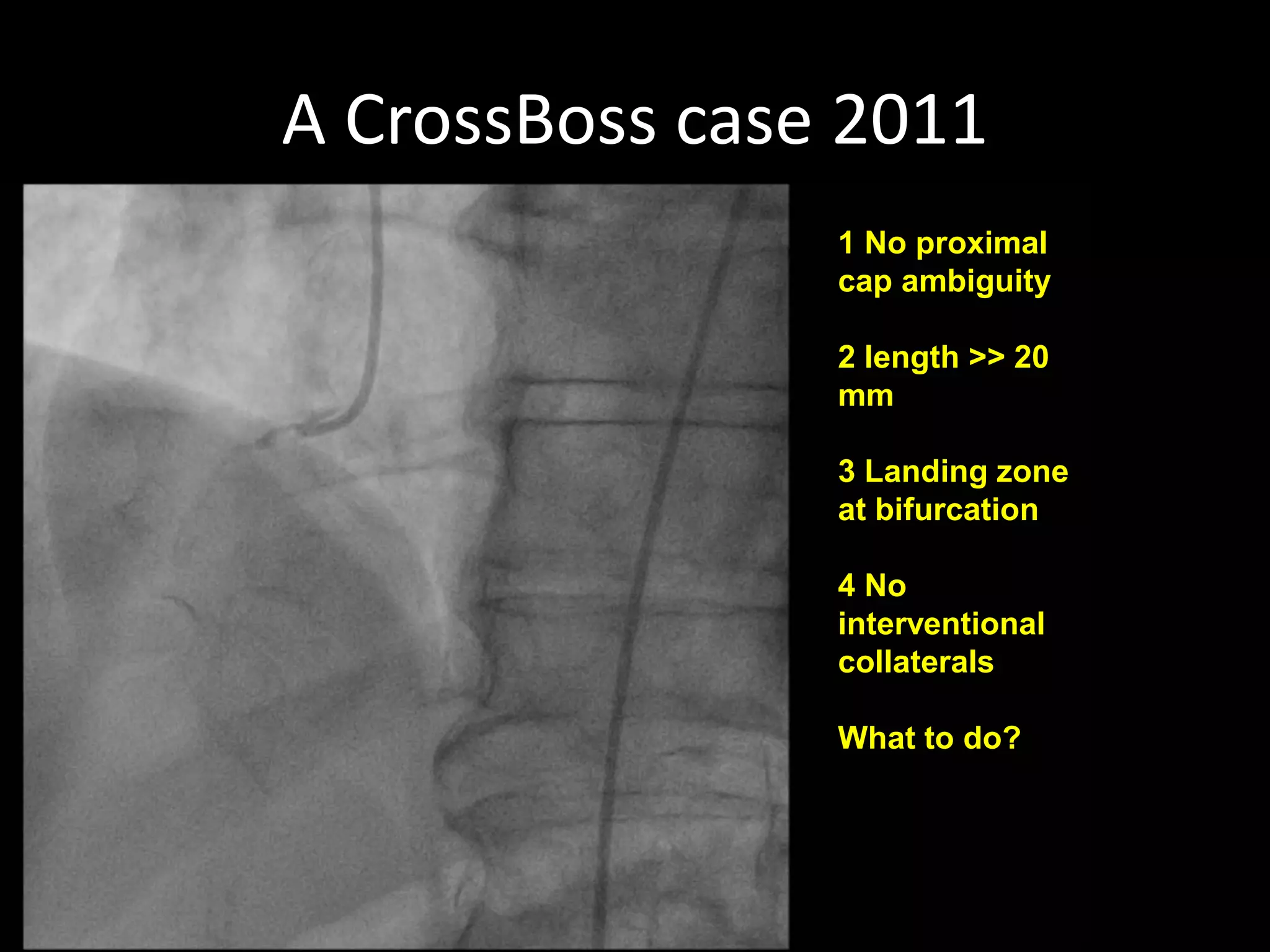
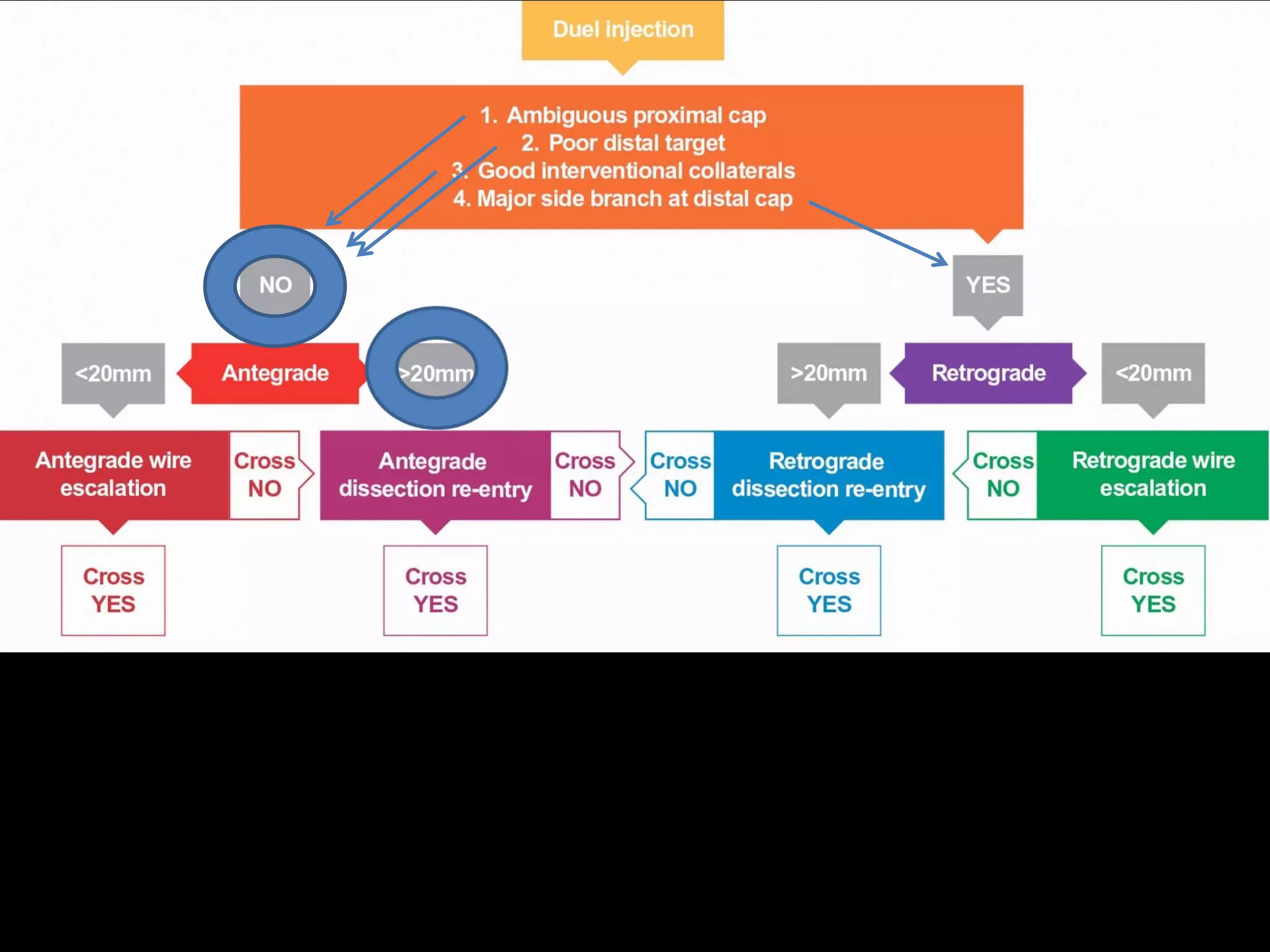
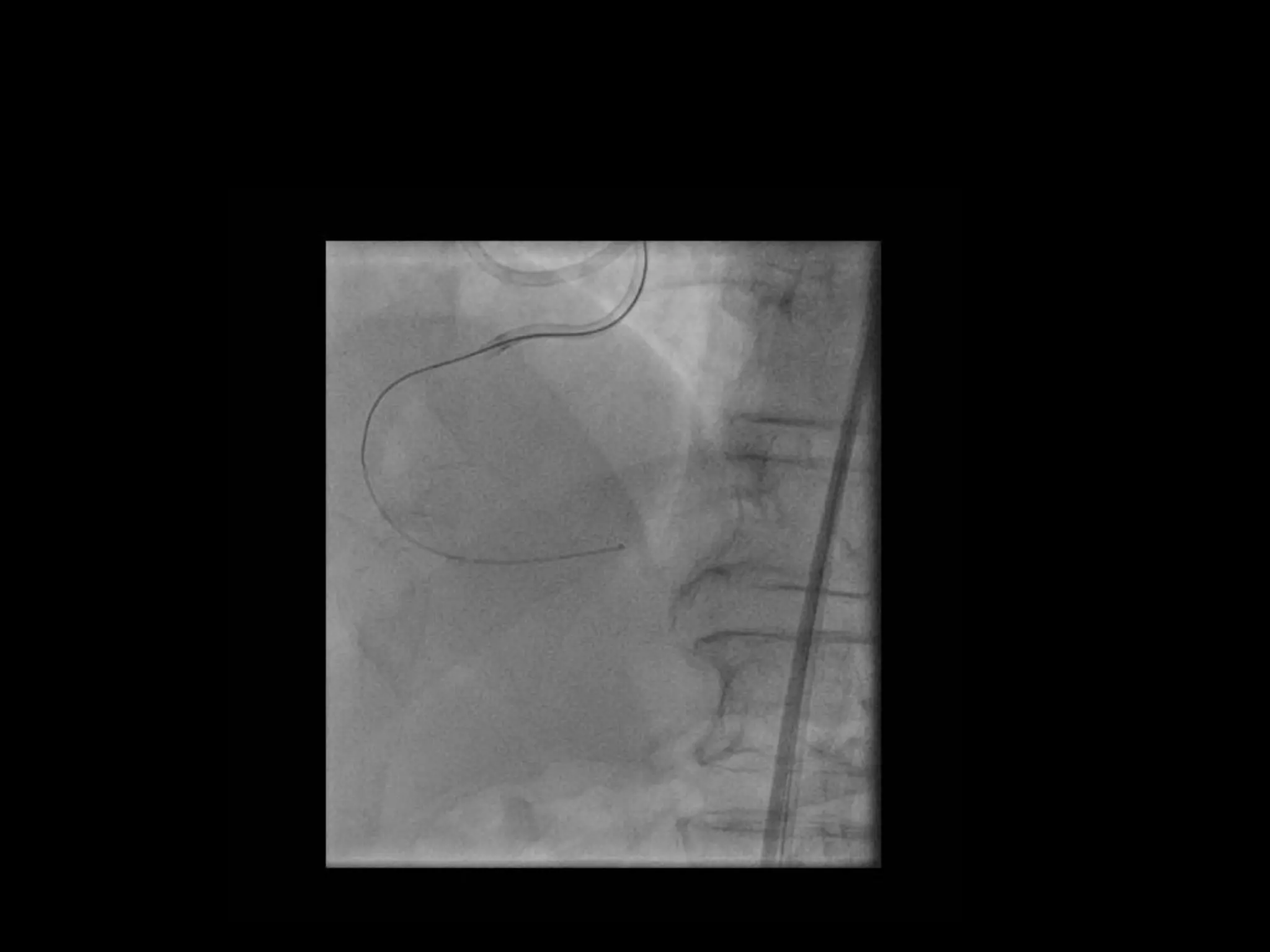
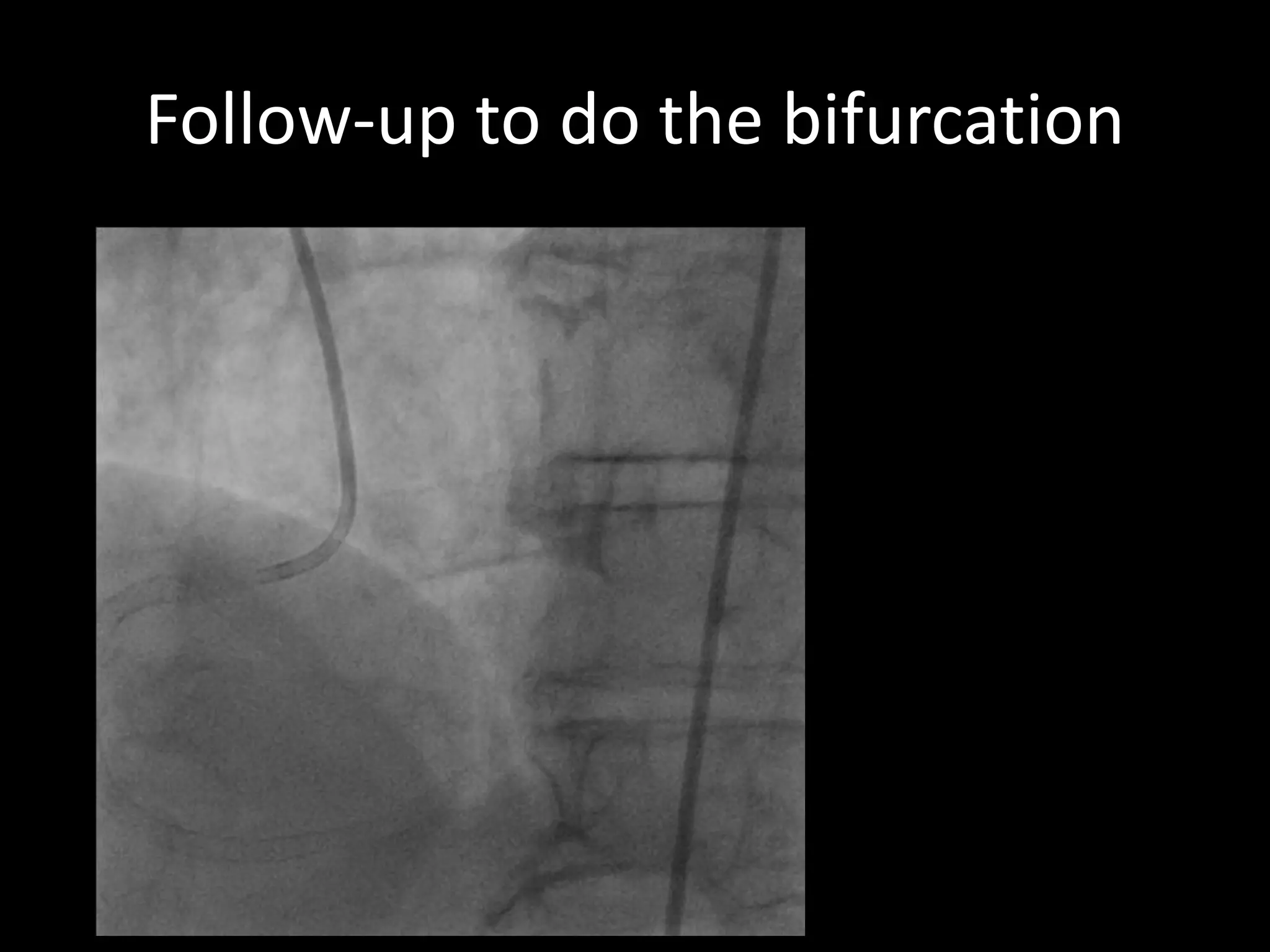
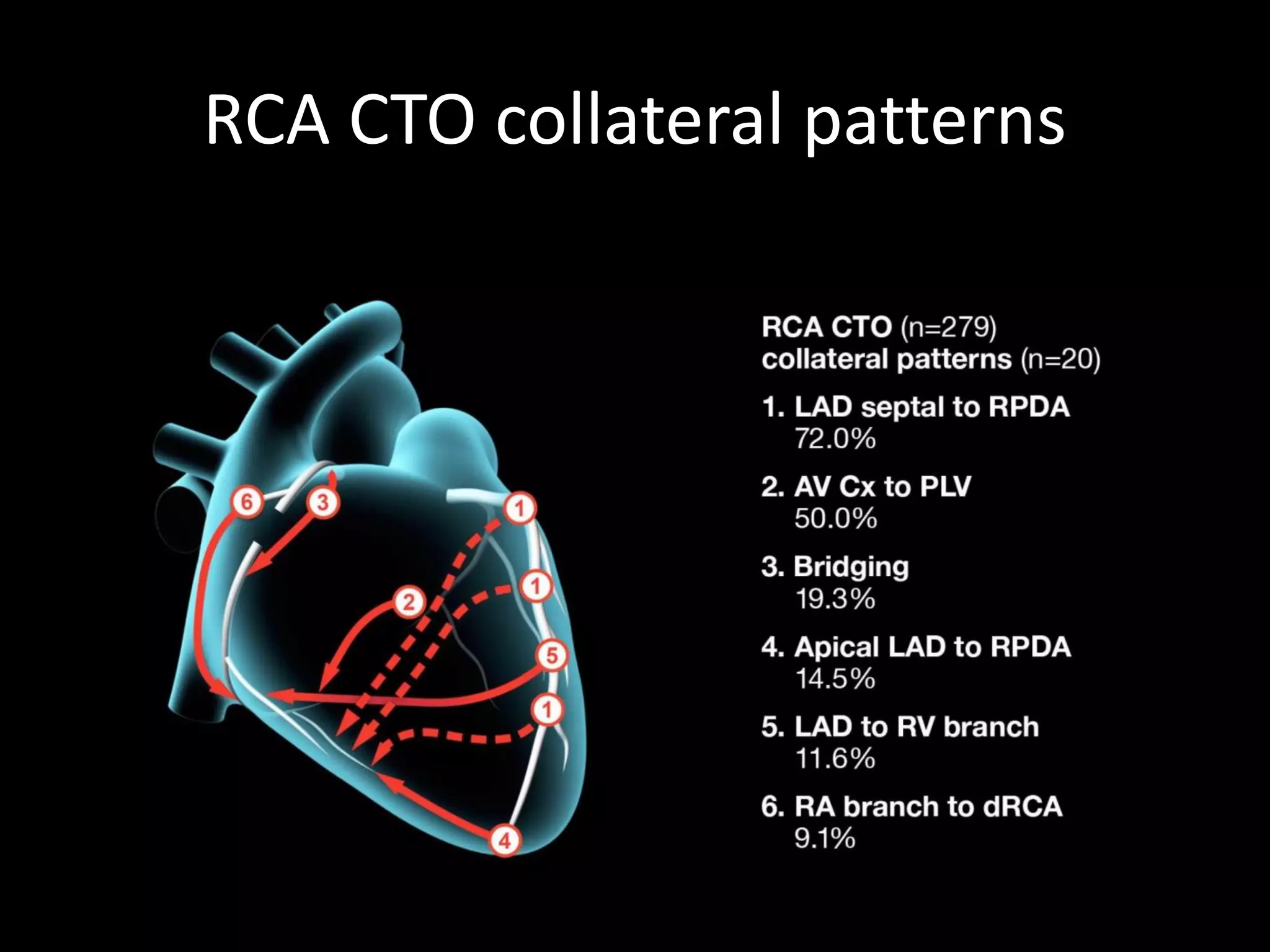
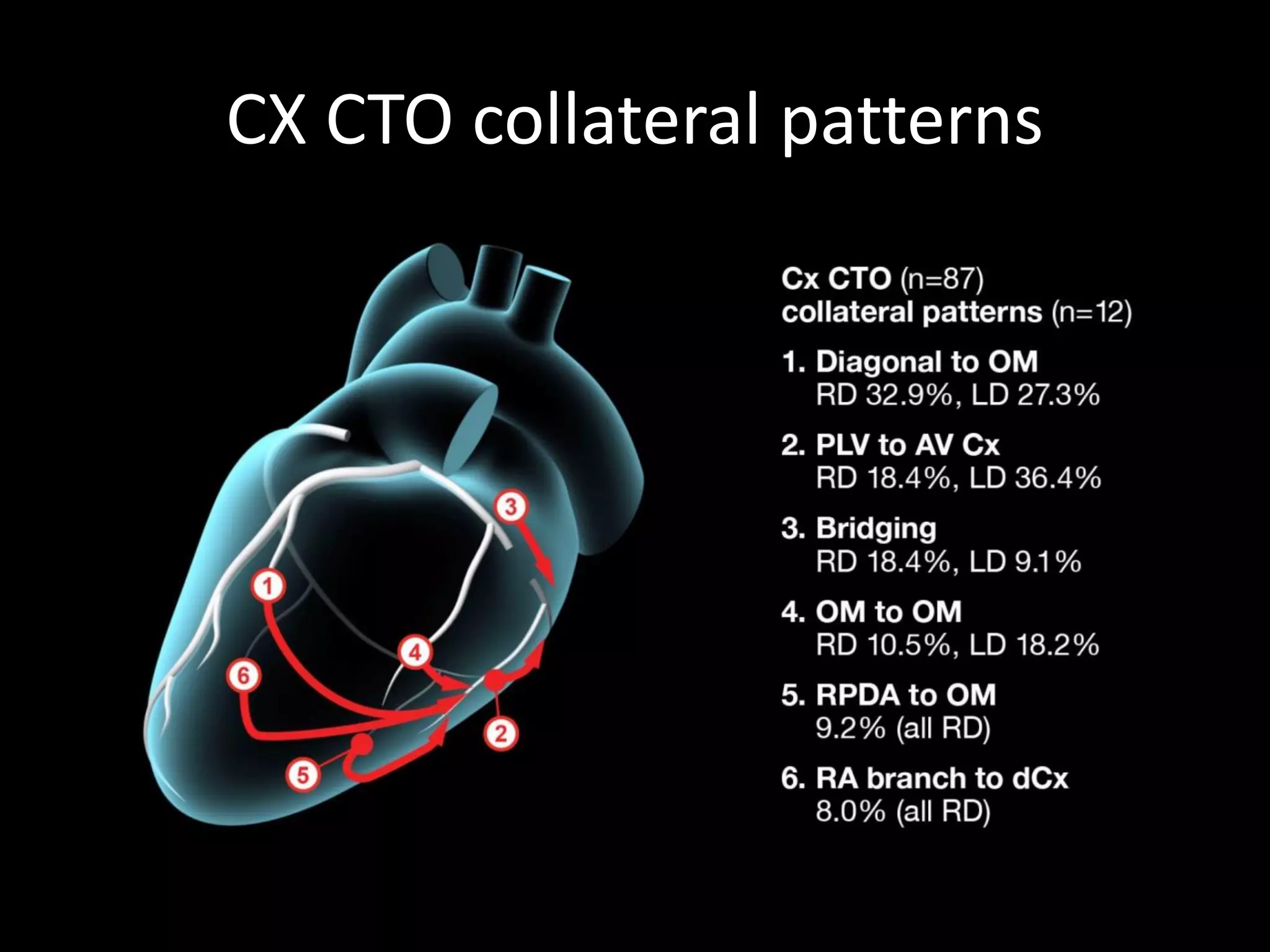
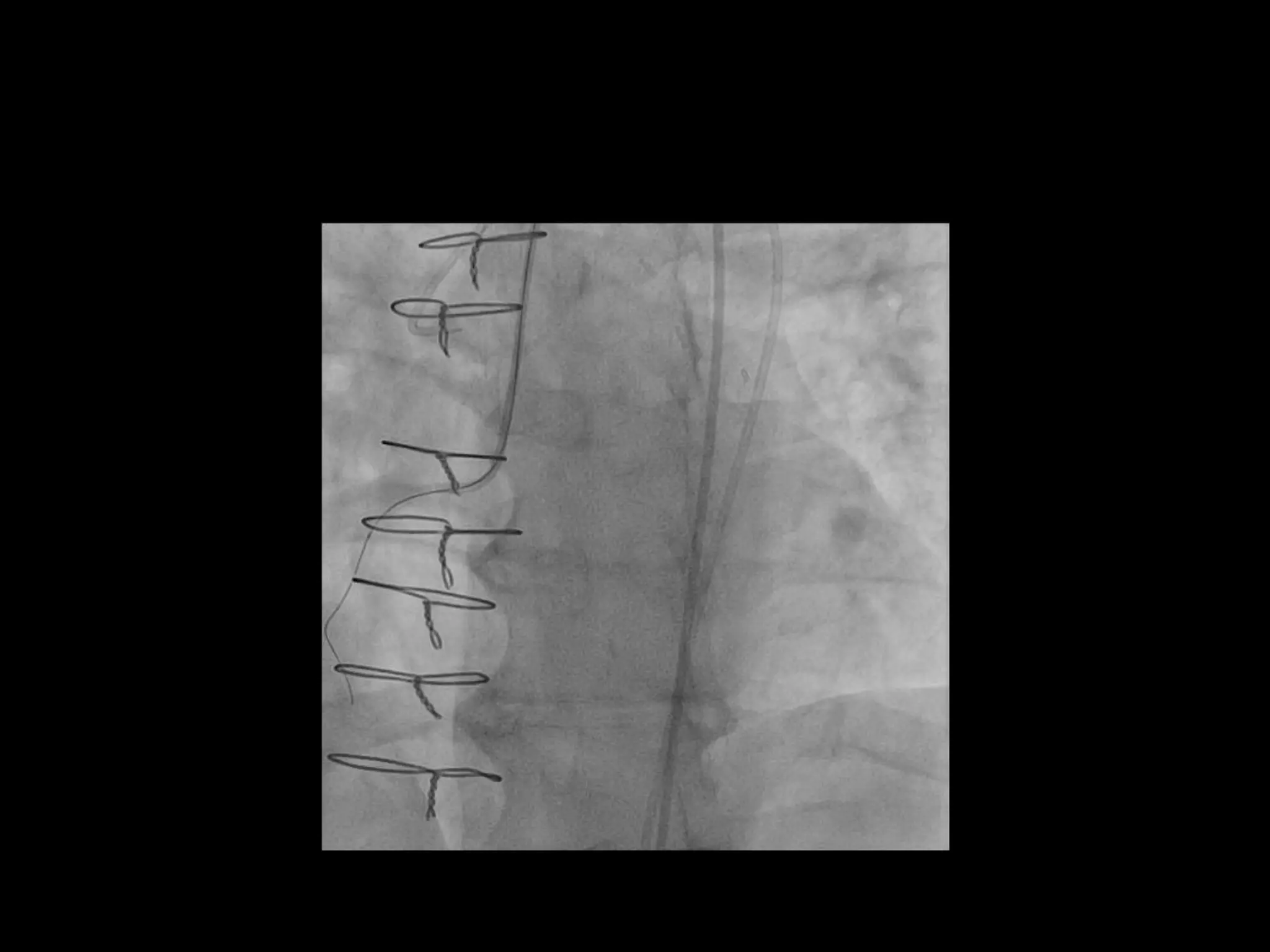
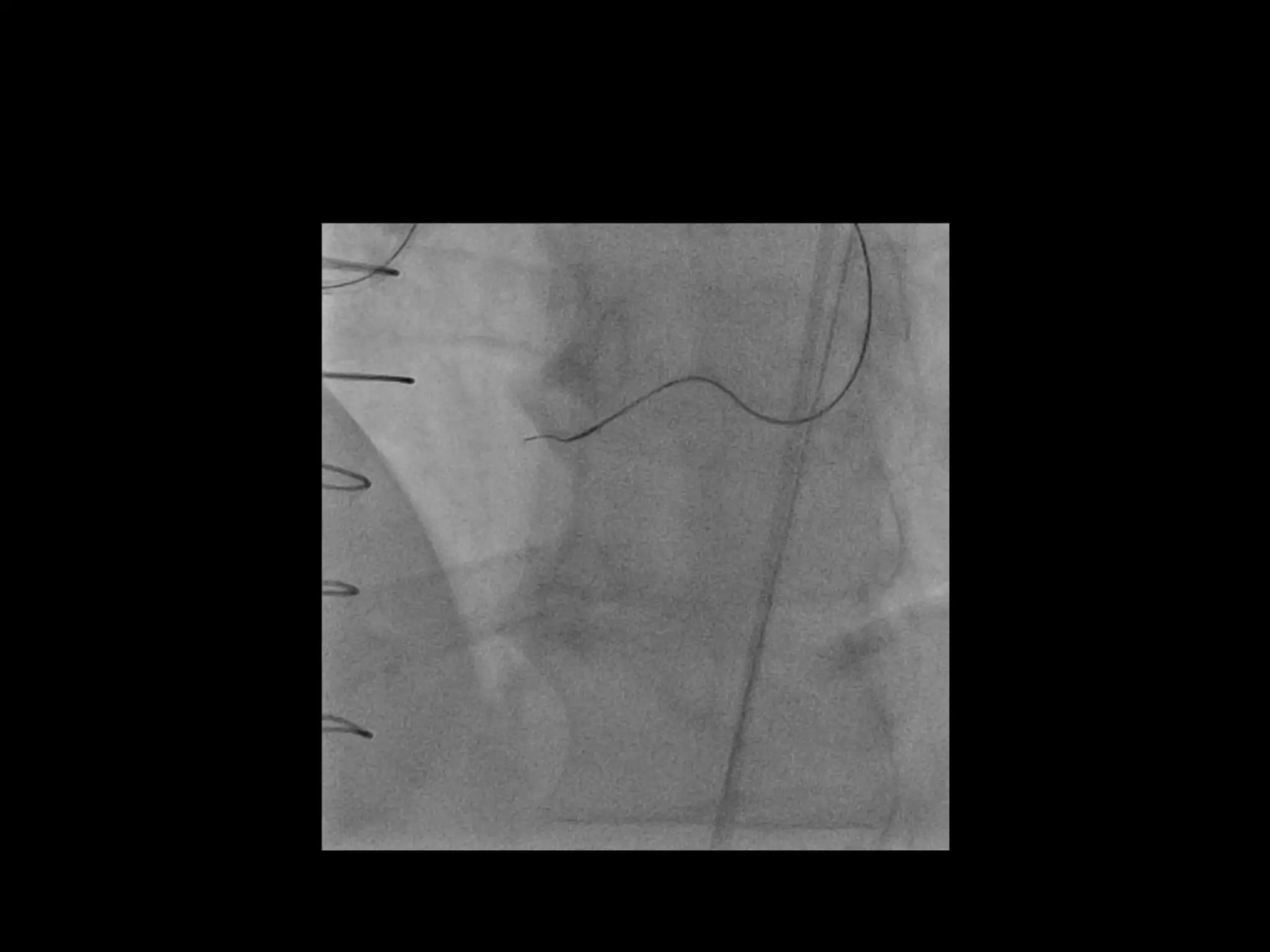
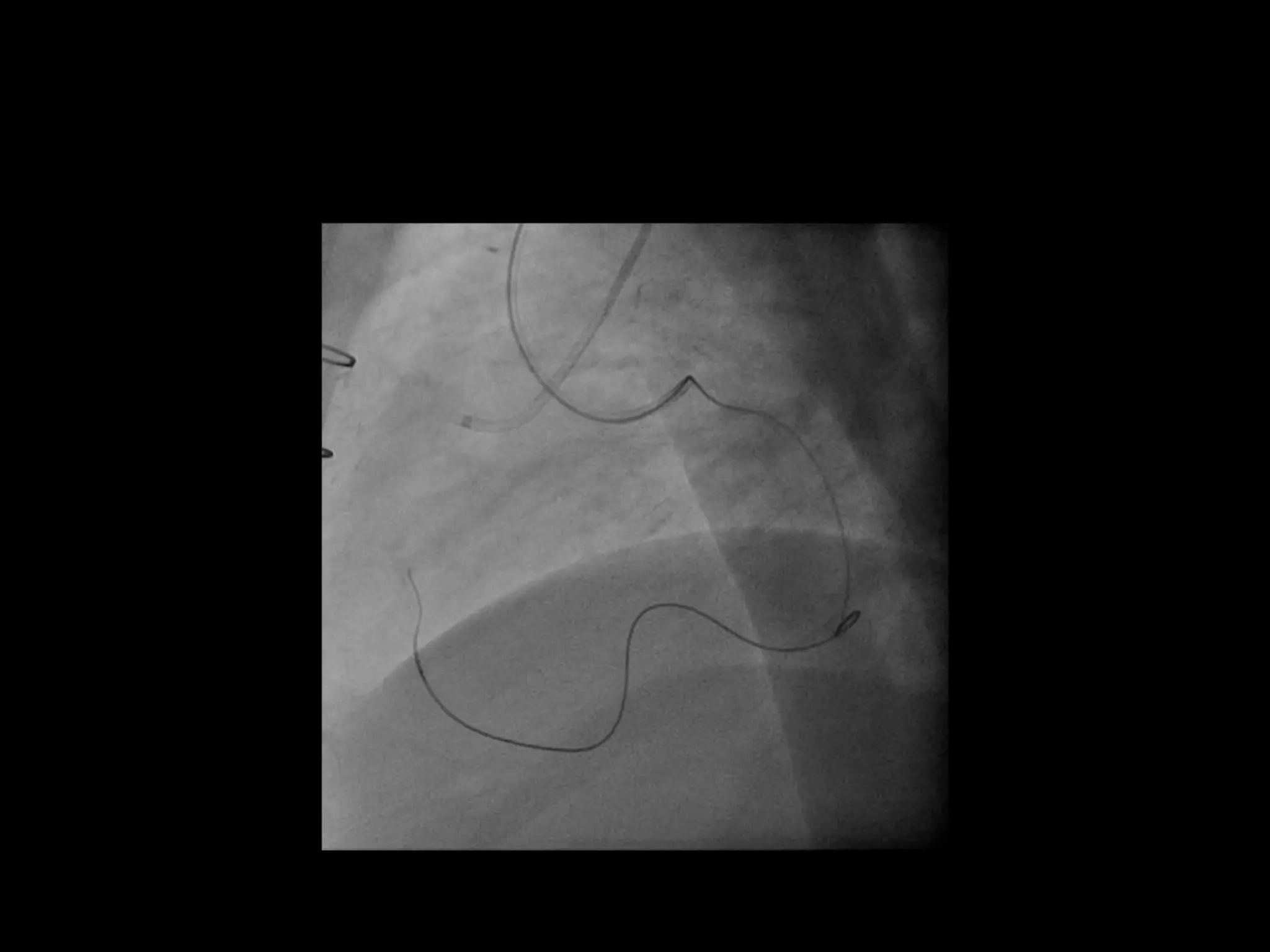
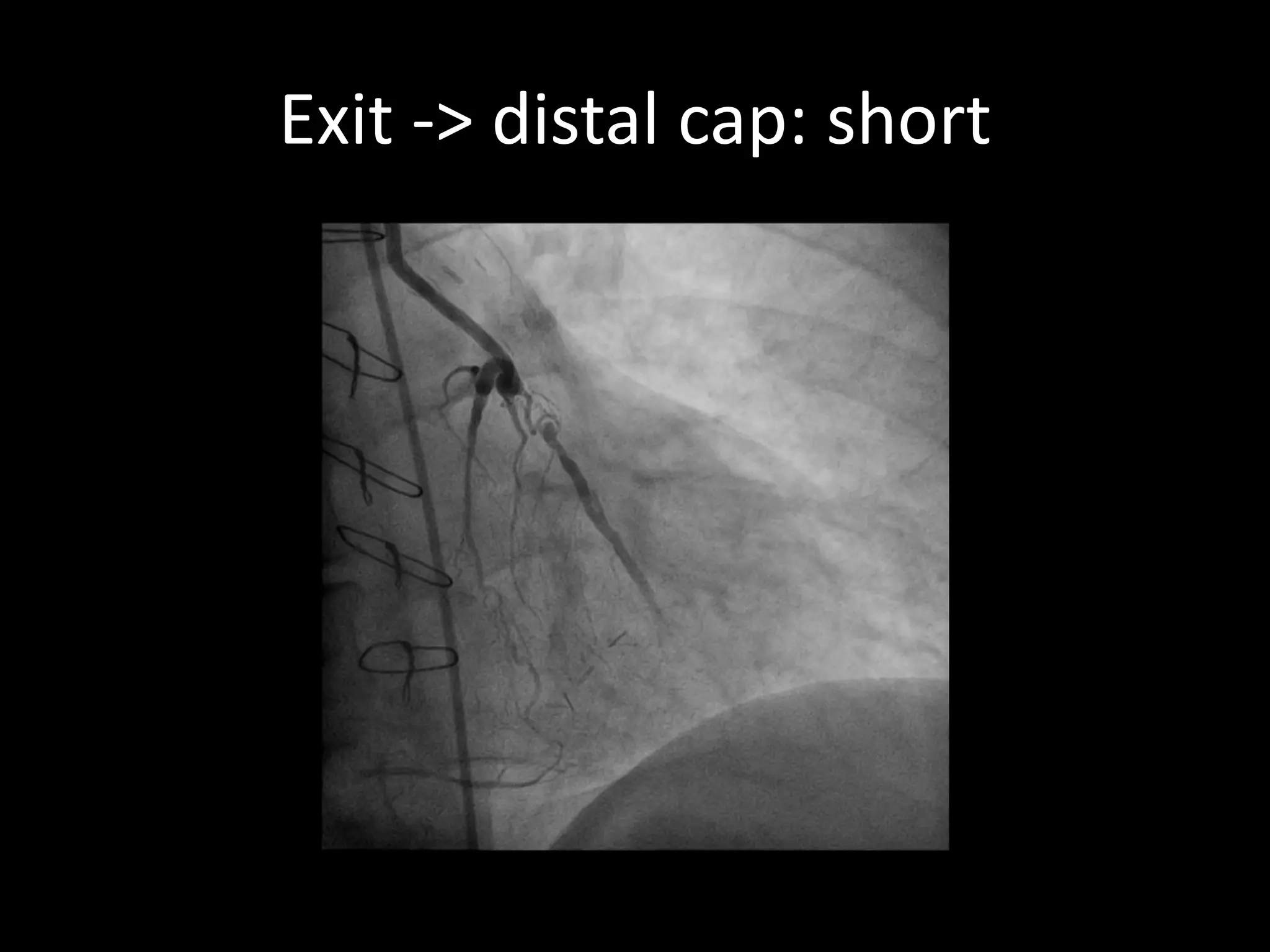
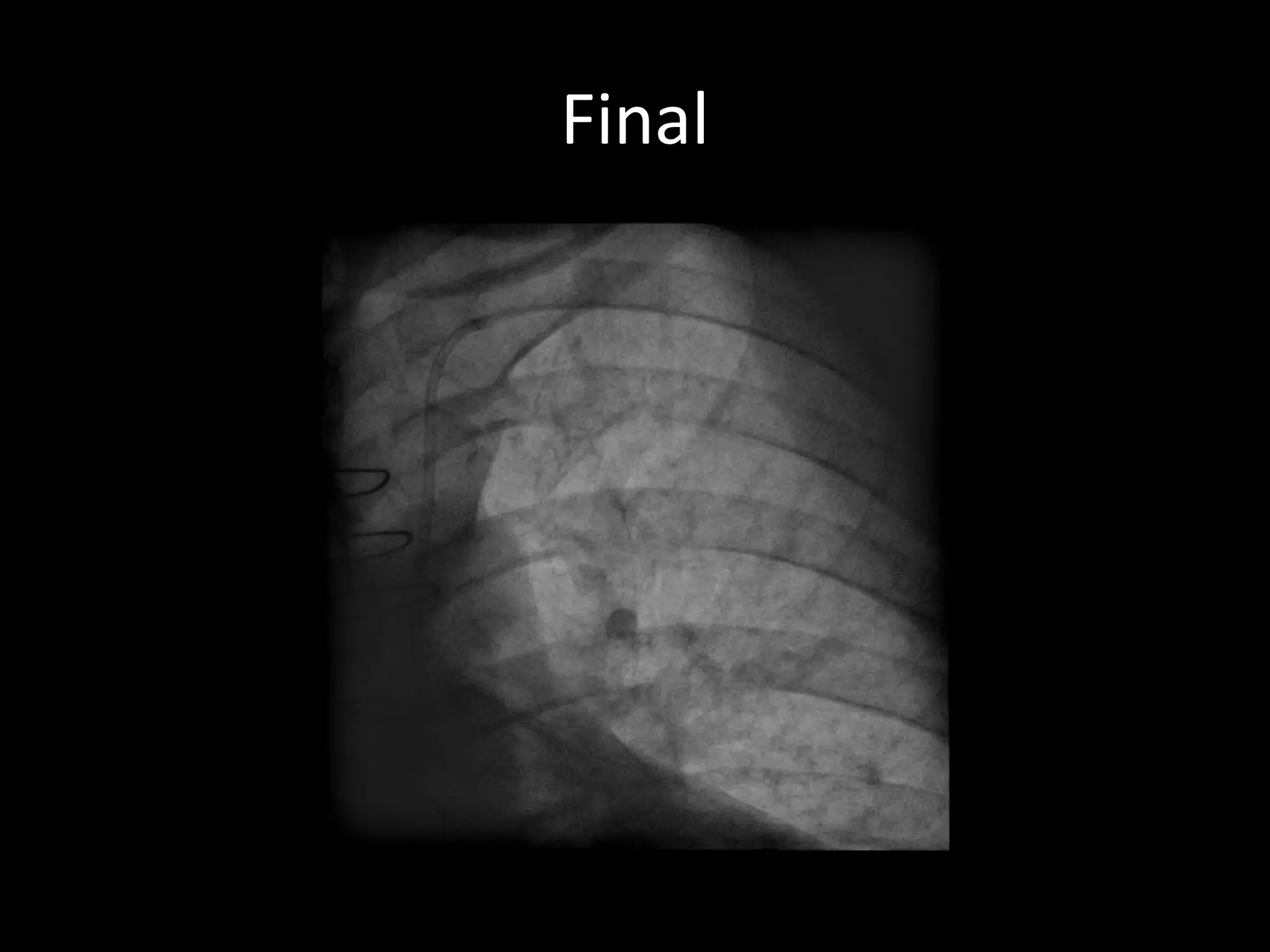
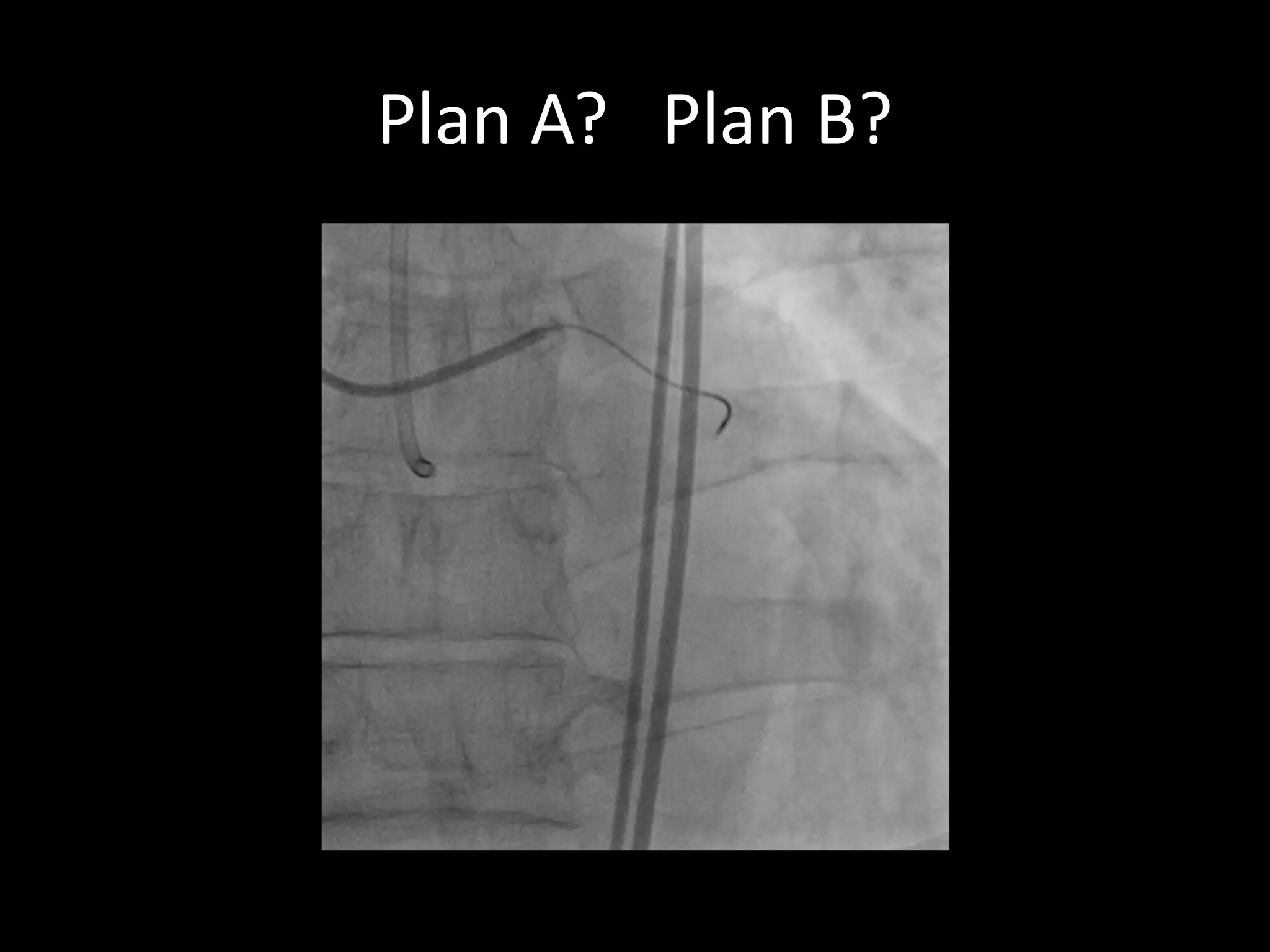
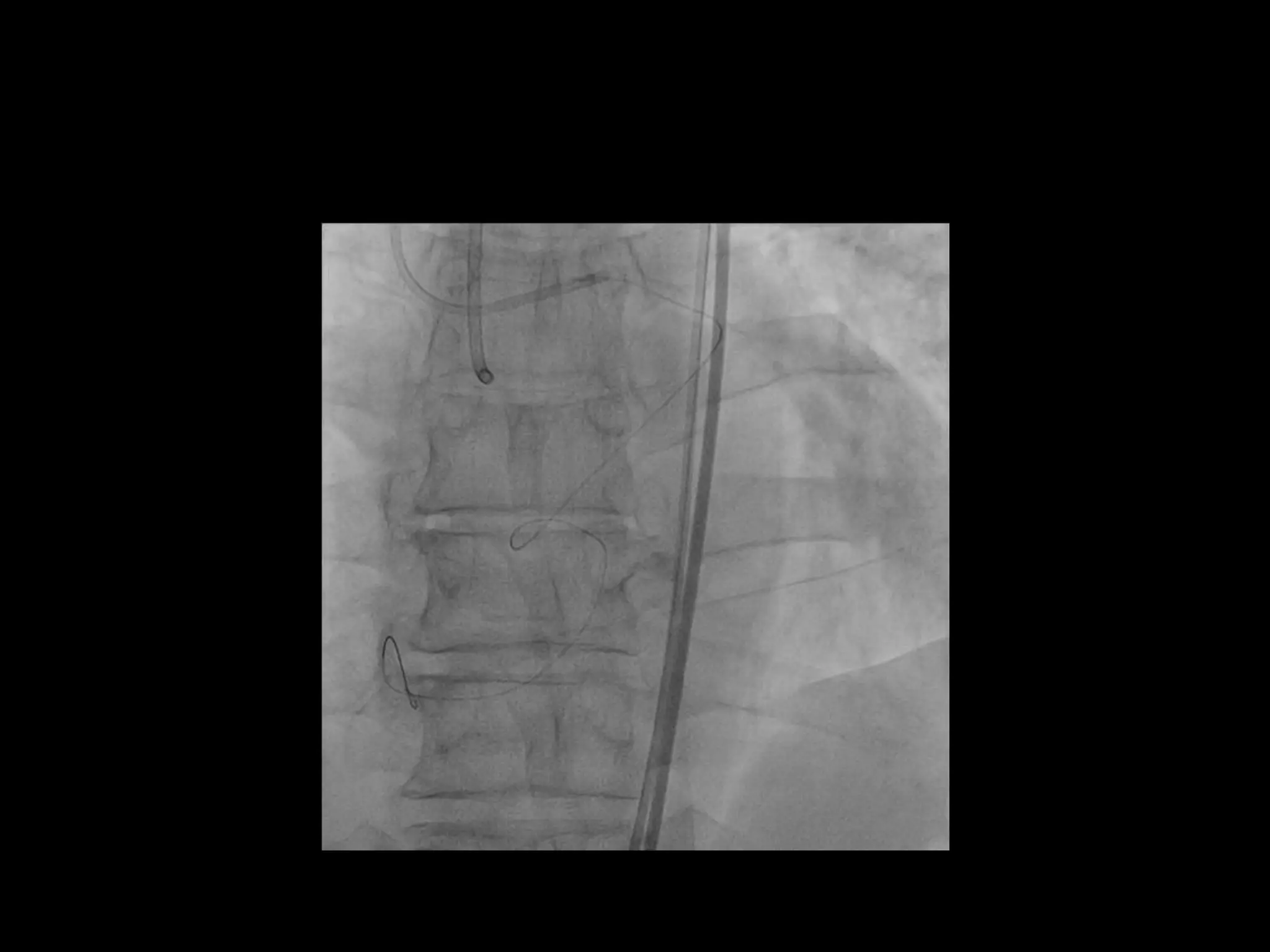
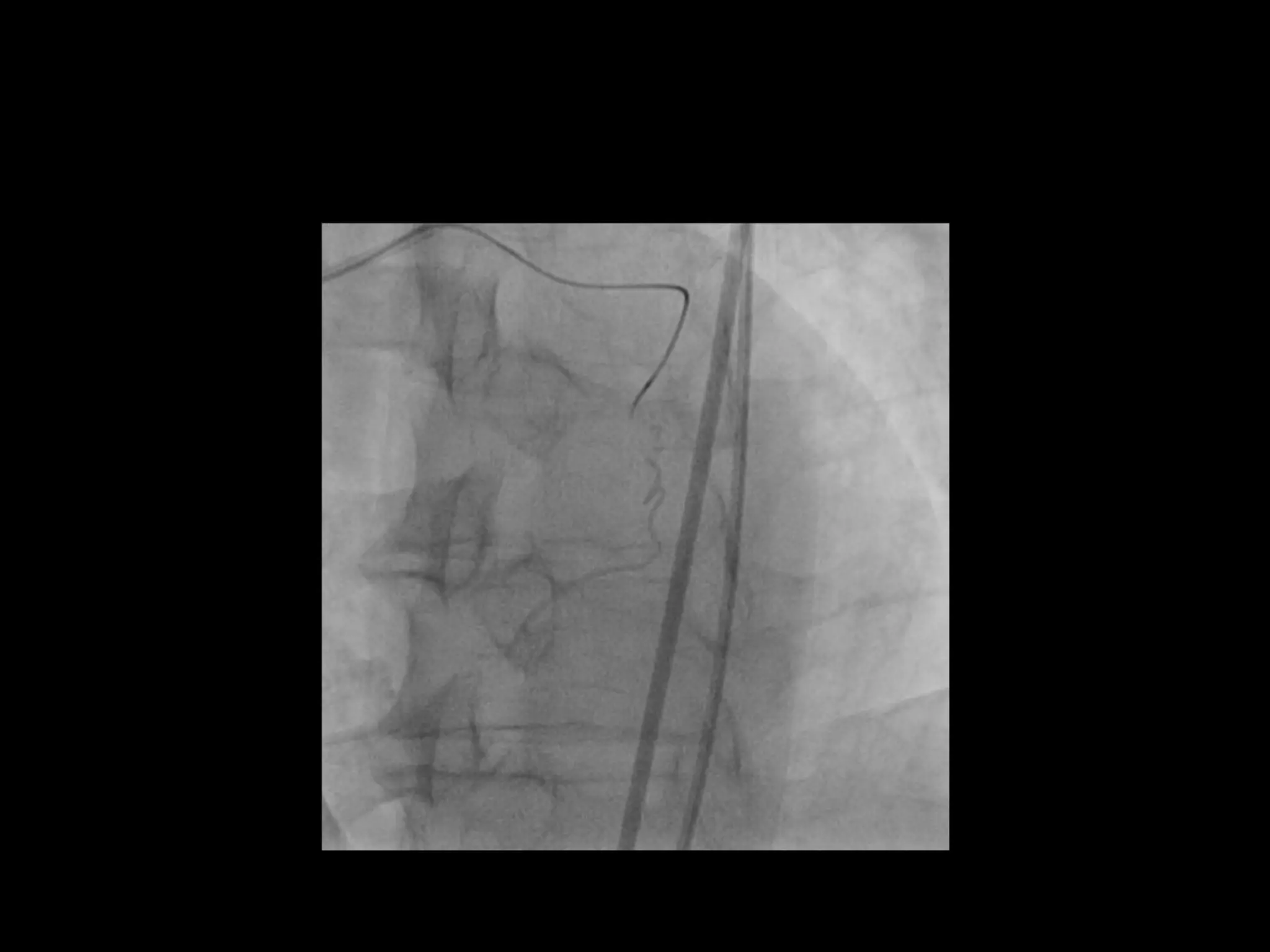
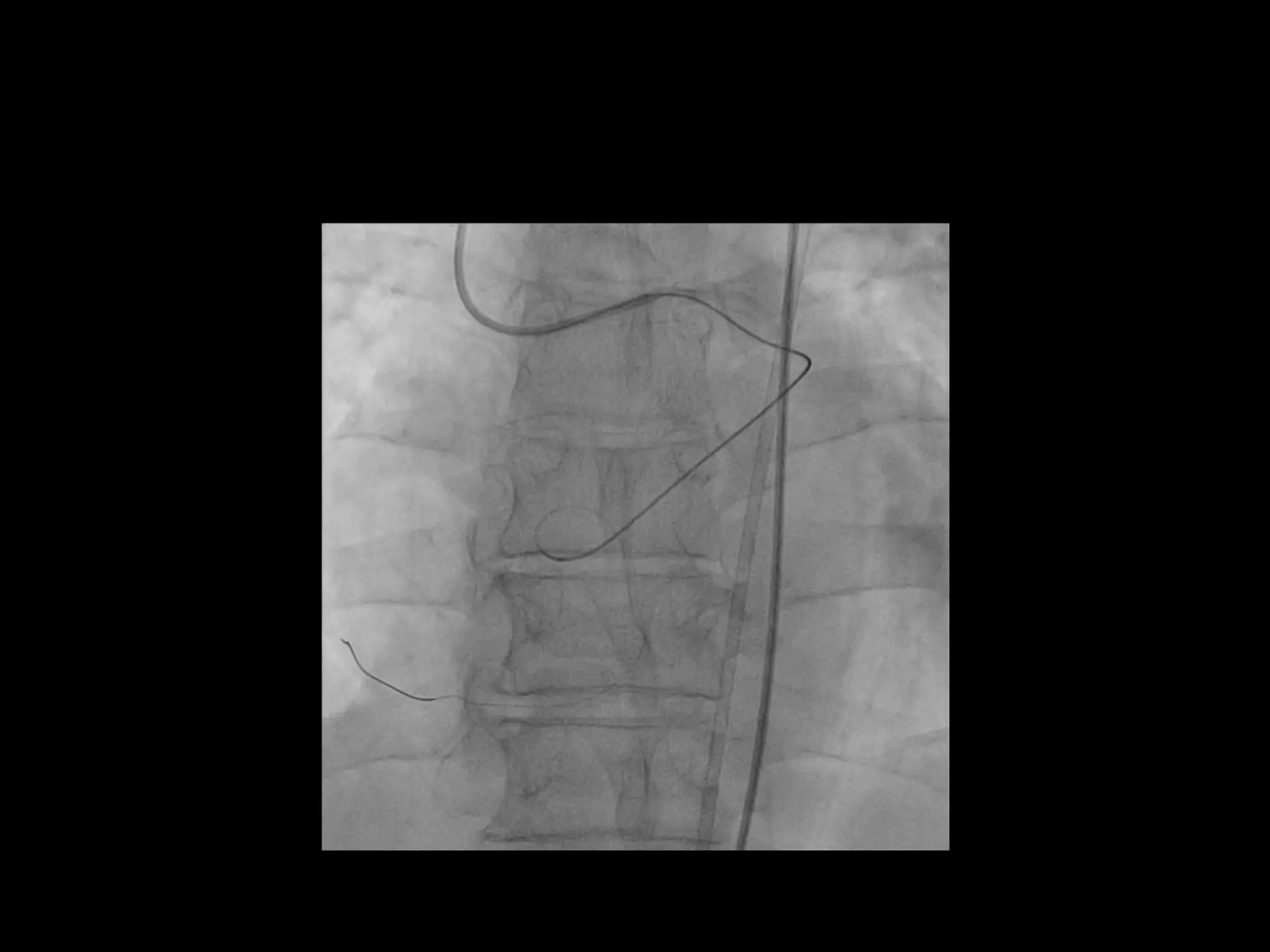
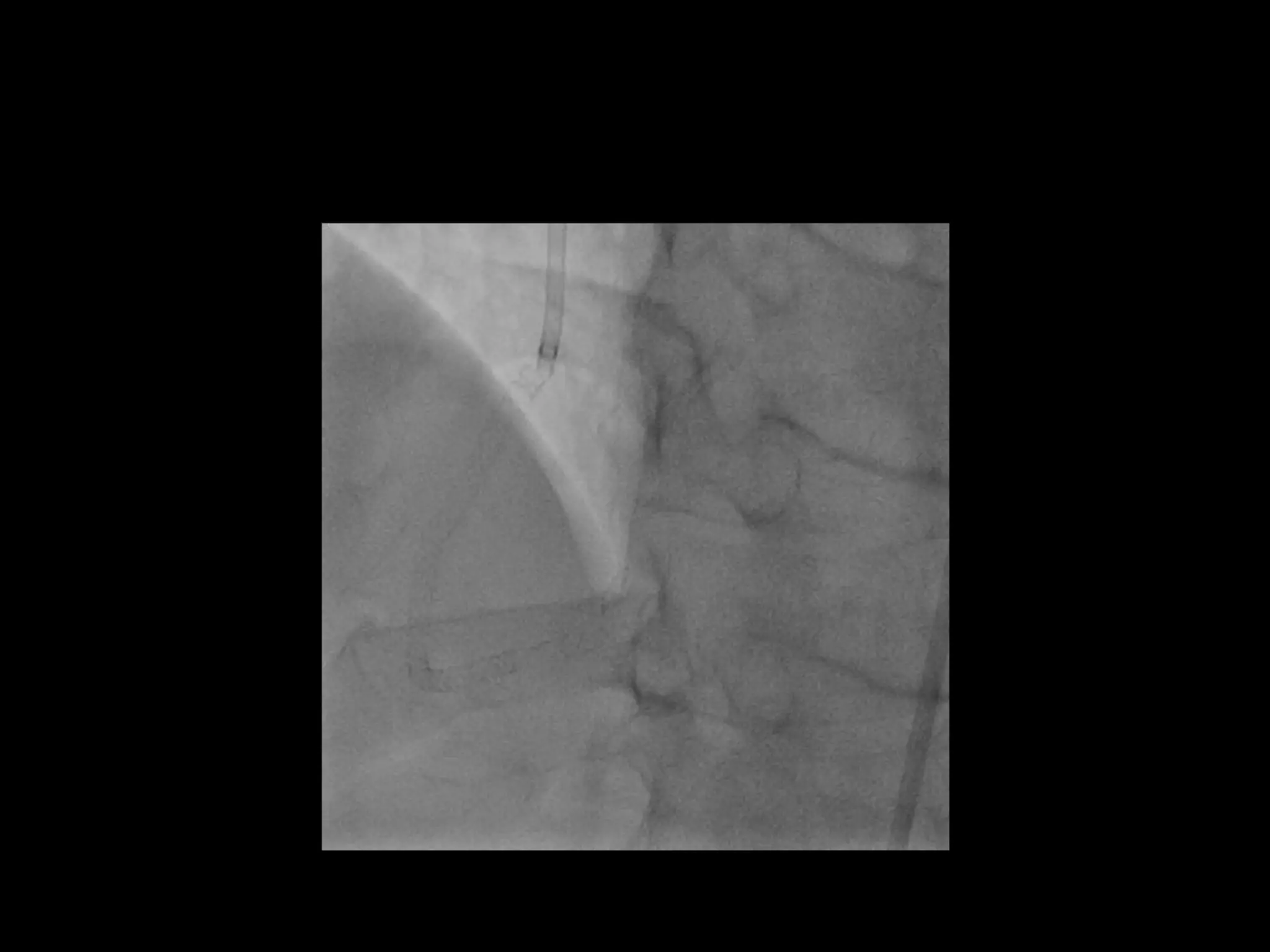
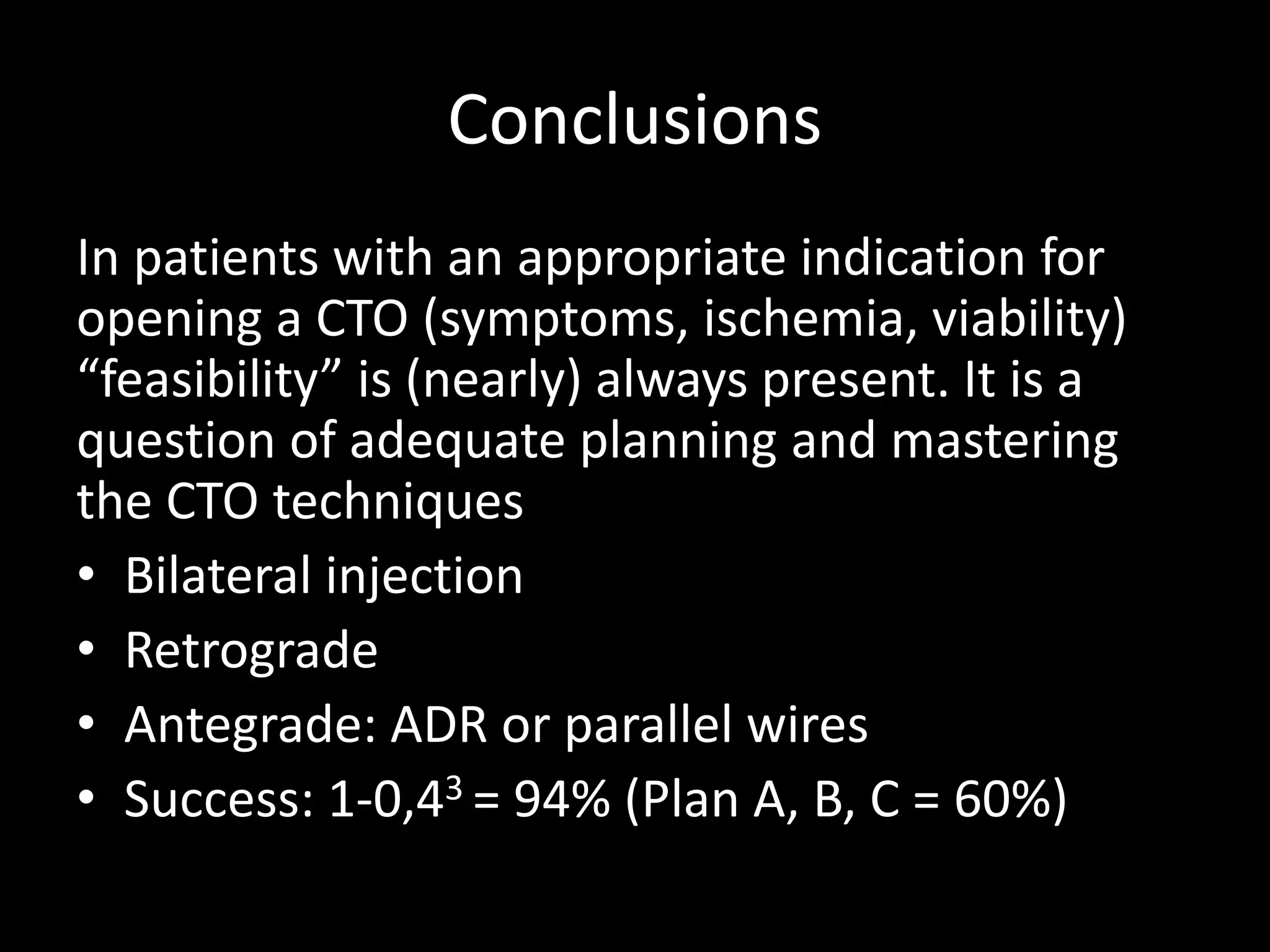
This document provides guidance on evaluating the feasibility of percutaneous coronary intervention (PCI) for a chronic total occlusion (CTO). Key factors to consider include: the patient's tolerance for a long procedure, contrast load, and radiation exposure; the CTO's proximal cap ambiguity, length, distal landing zone, and presence of interventional collaterals; and ensuring good quality angiography. With adequate planning and use of appropriate CTO techniques, feasibility is nearly always present for symptomatic patients. Success rates of CTO-PCI are reported to be 94% when using a planned approach.