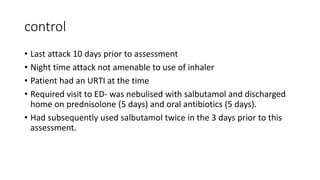
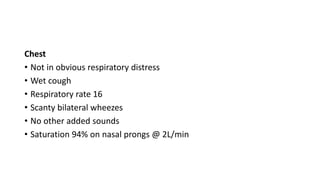
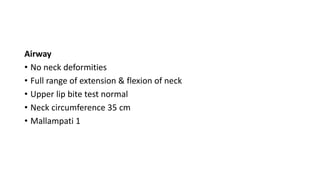
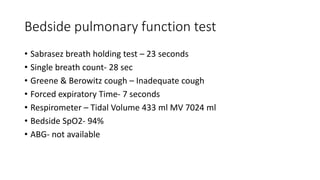
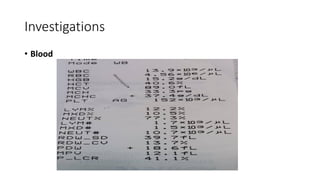
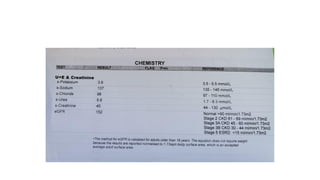
This case presentation describes a 32-year-old female patient scheduled for an appendicectomy who has a history of asthma. She presents with appendicitis and is being assessed for anesthesia. Her asthma is generally well-controlled with inhalers, though she had a recent exacerbation requiring oral steroids and antibiotics. On examination, she has wheezing but is not in obvious respiratory distress, with oxygen saturation of 94% on nasal prongs. Laboratory tests and vital signs are stable.