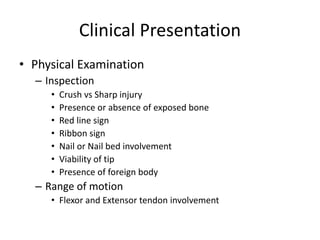
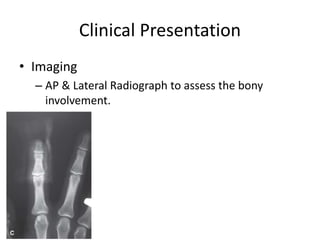
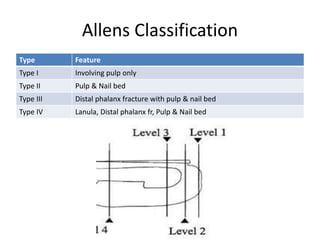
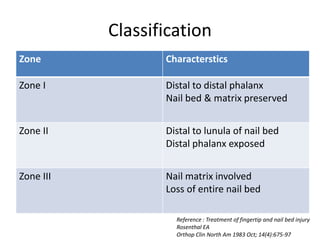
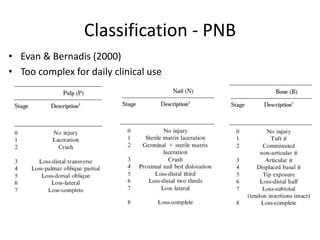
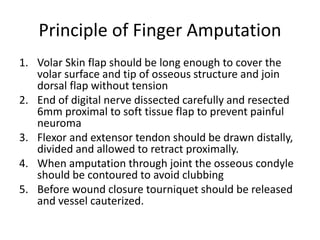
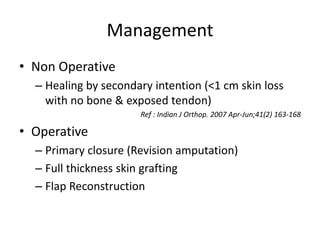
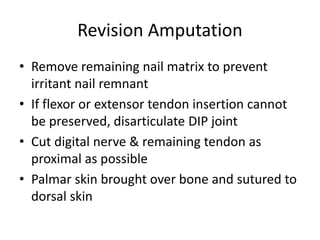
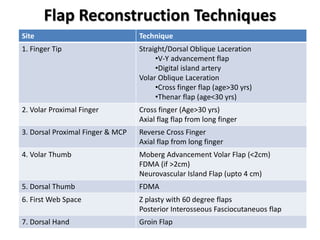
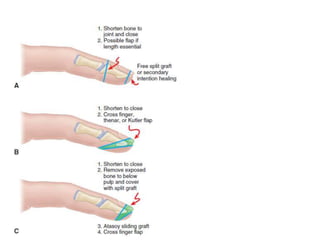
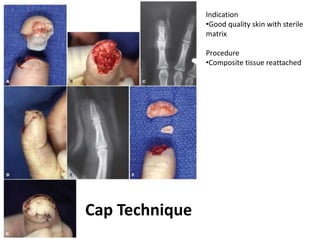
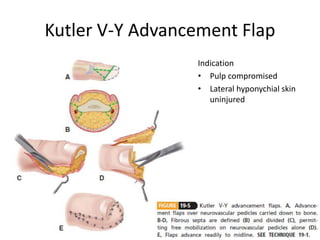
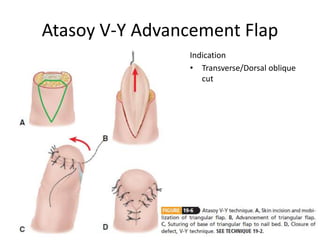
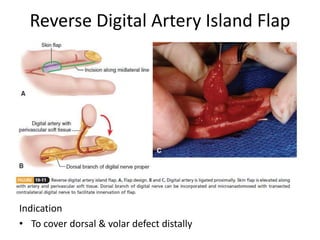
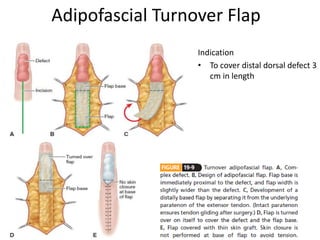
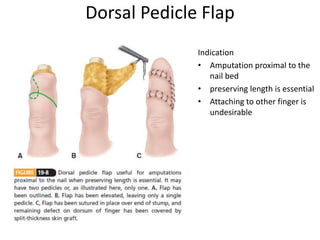
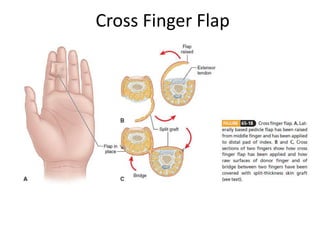
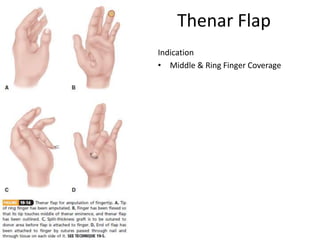
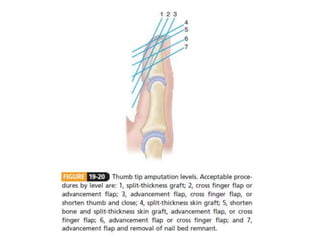
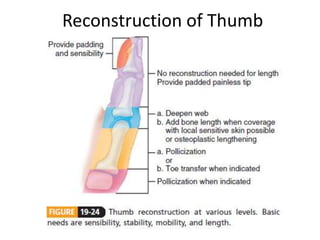
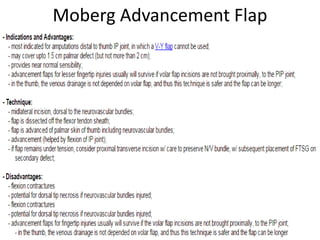
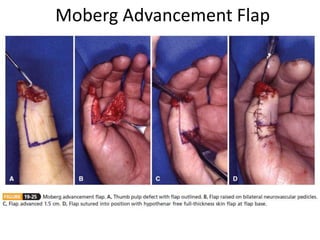
Finger tip injuries are common, especially in working adults and children, and require prompt treatment to restore function, sensibility, and a viable length. Injuries are classified based on the structures involved and treatments include revision amputation, primary closure, skin grafting, or flap reconstruction depending on the severity and location of the injury. Various flap techniques like V-Y advancement flaps or cross finger flaps are used to reconstruct the pulp and cover bone depending on the zone and site of injury on the finger or thumb.