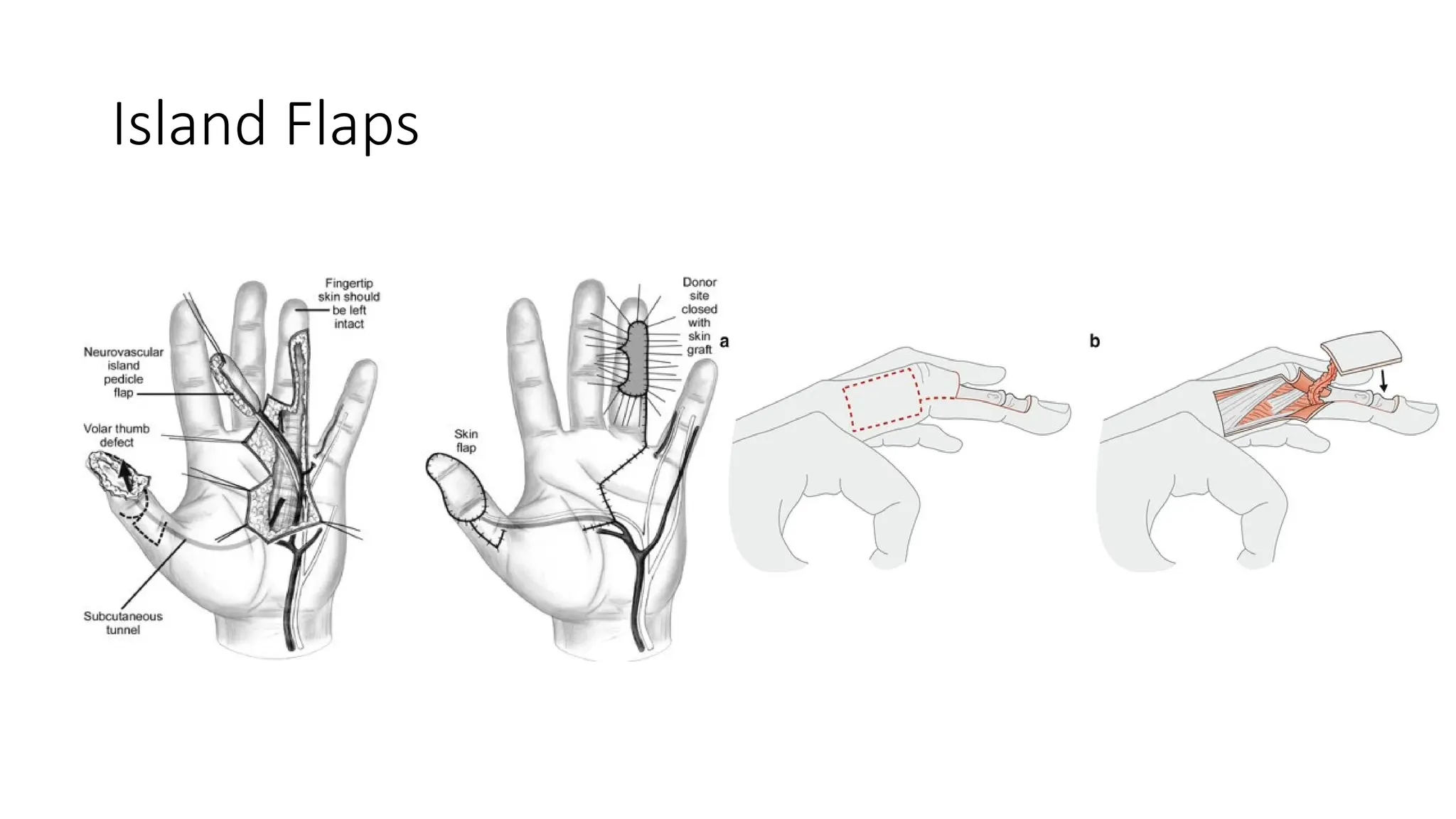
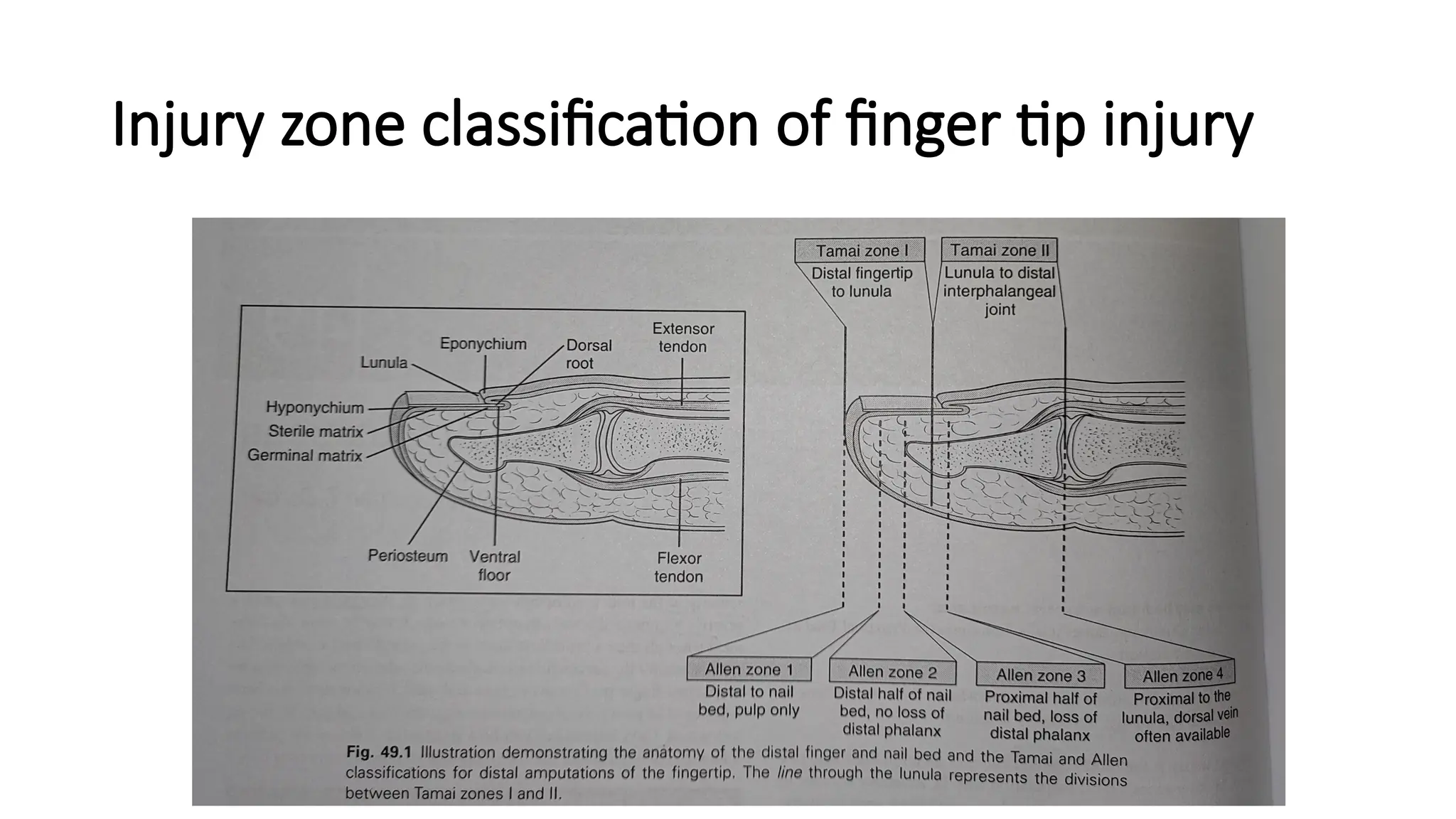
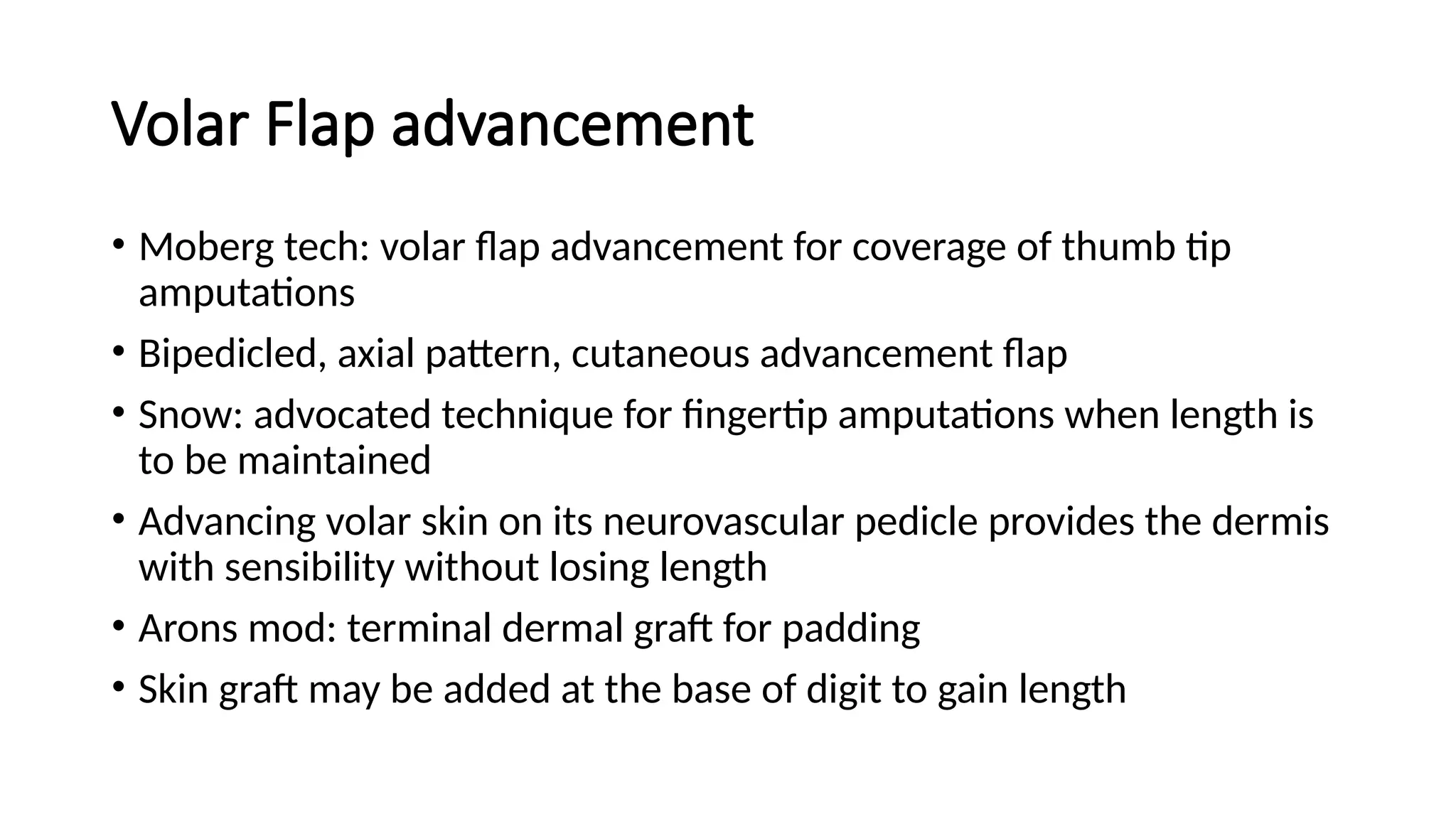
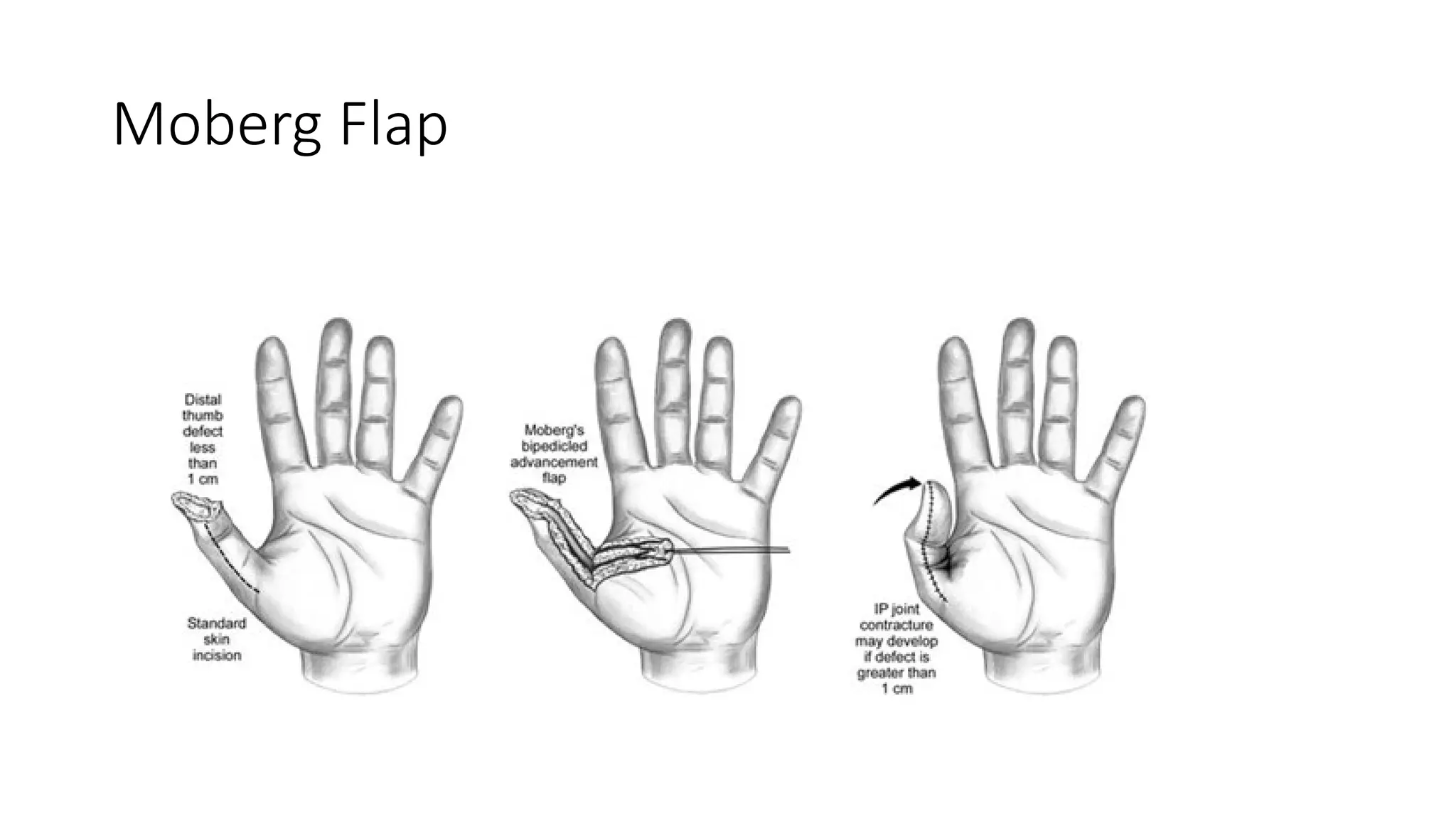
The document discusses various surgical approaches for managing fingertip injuries, emphasizing functional recovery and the importance of patient attitude. It outlines techniques like non-microsurgical reattachment, dressing for healing by secondary intention, primary closure, and split thickness grafting, each with specific applications based on the type and severity of the injury. The document highlights classification of fingertip injuries, goals of amputation surgery, and methods to reduce complications while allowing for early return to daily activities.

![• The area of contact of injured digital tip with thenar eminence is outlined
• An “H” is drawn on the skin approx. 20% wider than the defect
• Transverse limb of incision is made at the most distal contact point of fingertip with
thenar eminence
• Square proximal and distal flaps are elevated including s/c
• Proximal flap sutured to fingertip and distal flap is sutured to proximal margin of
defect on volar side of injured finger]proximal flap advanced distally and distal flap
advanced proximally to close the donor defect
• Soft dressing, 2 weeks later flap detached
• Fingertip closed with proximal flap and distal flap is advanced into thenar defect
• Closes donor site , problem of scar solved](https://image.slidesharecdn.com/00002fingertipinjury-241124174631-c78004ee/75/00002-FINGER-TIP-INJURY-pptx-TRY-TO-EXPLAIN-BASICS-AND-SHARE-THE-KNOWLEDGE-33-2048.jpg)