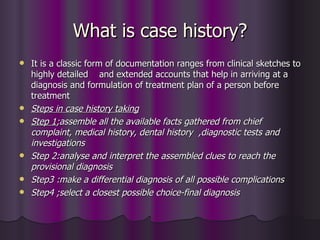
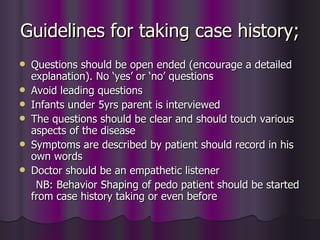
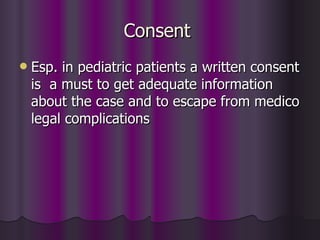
A case history provides essential clinical information to arrive at an accurate diagnosis and treatment plan. It involves gathering details from the chief complaint, medical history, dental history, and diagnostic tests. A thorough case history examination covers vital statistics, medical/dental histories, a review of symptoms, and physical and dental examinations. This information is analyzed to form provisional and differential diagnoses before confirming the final diagnosis and developing an appropriate treatment plan. A case history is a critical part of the clinical decision making process.

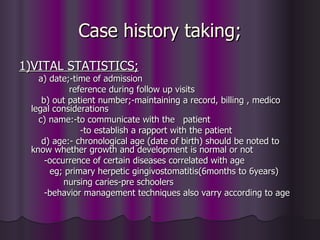
![e) sex;-girls mature earlier than boys-require treatment
earlier
-some diseases shows sex predilection
eg: anorexia-females
hemophilia -males
f) race/ethnic origin:-certain religious cultures depends the
etiology of certain diseases.
g) school/class:-to communicate with teacher
-to know the IQ level
h) address;-communication
-to chart out appointments for patients from distant
places
-to know endemic status of disease in the locality
i] socio economic status-to know about the nourishment,
hygiene, $ payment capacity of the patient](https://image.slidesharecdn.com/casehistorytaking-090714063032-phpapp02/85/dental-history-taking-8-320.jpg)