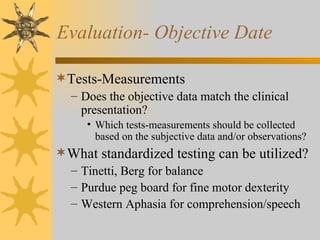
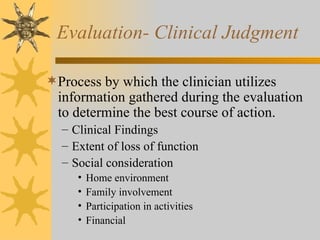
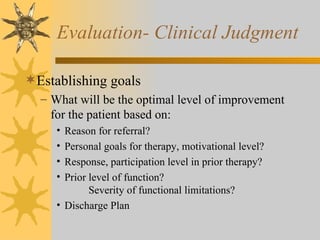
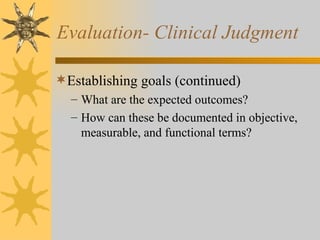
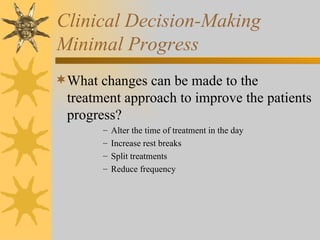
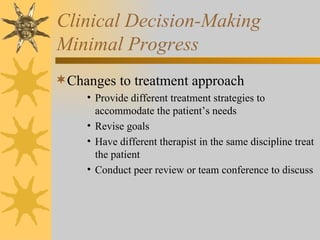
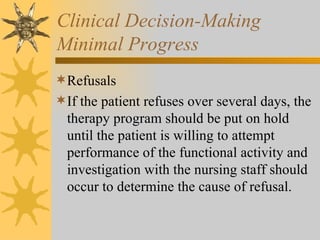
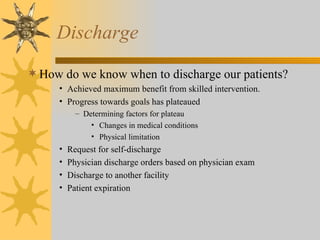
The document discusses clinical decision making in evaluating and treating patients. It involves gathering subjective and objective data from patients, determining appropriate goals and treatment plans based on evaluation findings and clinical judgment, monitoring patient progress, and determining discharge. Treatment plans are adjusted based on a patient's response. Frequent re-evaluations ensure treatment strategies remain appropriate.