Body fluids
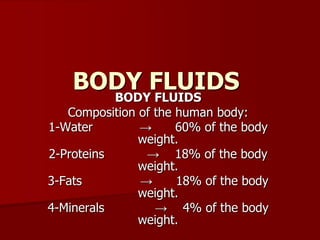
- 1. BODY FLUIDS BODY FLUIDS Composition of the human body: 1-Water → 60% of the body weight. 2-Proteins → 18% of the body weight. 3-Fats → 18% of the body weight. 4-Minerals → 4% of the body weight.
- 2. Body Water -Water constitutes about 60% of body weight in young adult male. -The amount of body H2O decline with age: -The new born has about 82%of body weight as H2O at birth and elderly about 52%.
- 3. Body Water -Loss of body H2O is a common cause of death in children who suffer from dehydration. -The amount of H2O in the body is affected by the quantity of body fat.. Lean subjects have a higher percentage of H2O than those with more body fat. This is because adipose tissue contains far less H2O than muscle, skin, and other soft tissues.
- 4. Body Water Variation of body H2O with age and sex as % of body weight Male Female At birth 82% 82% Children&adolescence 70% 70% 18-20 years 59% 57% 20-40 years 56% 51% 40-60years 55% 47% Over 60 years 52% 46%
- 5. Body Water A man who is weighing about 65 kg, the total body water (TBW) is equal to 40 Liters it is subdivided into: 1-Intracellular :(inside the cells)ICF: It is about 2/3 of total body water(25 liters) 2- Extracellular:(outside the cells)ECF:It is about 1/3 of the total body water(15liters)
- 7. Body Water The extracellular fluid is further subdivided into: a)Intravascular(inside the blood vessels): It is the blood plasma(3 liters). b)Interstitial(between the cells) in the tissue spaces(12 liters), it is similar to the plasma but with low protein content. c)Transcellular(500 ml):It found in special compartments in the body such as the pleural cavity, peritoneal cavity, spaces between the lining of the brain and spinal cord (CSF)and the joint cavities.
- 8. Body Water There is continuous exchange between the intravascular and interstitial fluid to supply the nutrients needed by the cells and removing the waste products. This exchange keeps the internal environment constant
- 9. Comparison of ECF&ICF solutes: ECF contains large amount of Na+ and Cl- but only small amounts of K+,Mg++ and PO4-- In contrast, ICF contains large quantities of K+,PO4--,moderate amounts of Mg++ and exceedingly few Ca++.
- 10. Osmolality of body fluids: Because the cell membrane is highly permeable to water, the osmolarity of ECF&ICF compartments are normally the same, about 290milliosmol/L The plasma osmolality is calculated by using the following formula: Osmolality =2[Na+] +0.055[Glucose] +0.36[ Urea] mEq/L mg% mg%
- 11. Mechanism of water balance: Normally ,total body water remains constant, therefore over 24-hours period, intake and loss of water must balance exactly to precisely regulate ECF osmolality and Na+ concentration. Maintenance of TBW balance involves regulation of both water excretion by the kidneys and regulation of water intake by the thirst mechanism.
- 12. Mechanism of water balance: Water intake: 1-Drinks and food → supply about 2100 ml/day. 2-Oxidation of carbohydrates, produces about 300ml/day.
- 13. Mechanism of water balance: Water loss: 1-Urine: about 1.5L/day. 2-Sweat: variable amount depending on the environmental temperature and physical activity. The volume of sweat is normally 100ml/day.In hot weather or during heavy exercise, water loss may increase up to 1-2 liters/hour. 3-Insensible water loss by evaporation through skin and respiratory system. It is termed insensible water loss because we are not consciously aware of it. It is about 0.5 L/day.
- 14. Mechanism of water balance: Regulation of water intake: -It is controlled by thirst sensation. -Thirst sensation: It is the conscious desire for water. -The thirst center is found in the lateral nuclei of the hypothalamus. -This center is connected to the osmoreceptors in the anterior nuclei of the hypothalamus.
- 15. Regulation of water intake: Water intake is stimulated by: 1-Inceased effective osmotic pressure of the plasma: It acts via osmoreceptors located in the anterior hypothalamus. When the Na+ concentration increases about 2 mEq/L above normal, the thirst mechanism is activated causing a desire to drink water .This is called the threshold for drinking. 2-Decreased extracellular fluid volume: Hemorrhage or hypotension caused increased drinking even though there is no change in osmolality of the plasma
- 16. Regulation of water intake: Mechanism: a)Renin-Angiotensin System: Hypovolemia stimulates Rennin secretion→ resulting in rise of Angiotesin II in the circulation. Angiotensin II stimulates thirst & acts on the kidney to reduce fluid and electrolyte excretion. b)Baroreceptors in the heart and blood vessels:
- 17. Regulation of H2O excretion by kidney: -Urine output is regulated and is one of the primary contributions to maintaining water balance. -Daily urine output can be as high as 20L or as low as 500mL depending on the water intake
- 18. Regulation of water intake: Mechanism: 3-Other factors: -Dryness of the pharyngeal mucous membrane→ thirst sensation. -Prandial drinking: The intake of liquids is increased during eating: a-Increased plasma osmolality as food is absorbed. b-Gastro-instinal hormones may stimulate the thirst.
- 19. Regulation of H2O excretion by kidney a-In conditions of H2O excess: as a result of excess fluid intake: The renal response is to increase water excretion. In conditions of maximal water excretion urine volume can increase to 18-20L/day. b-Conditions of fluid depletion: as a result of restricted intake or inappropriate losses, the renal response is to reduce water excretion. The urine volume can be reduced to as little as 500ml/day .
- 20. Regulation of H2O excretion by kidney -The ability of the kidney to excrete urine of variable volume and osmolality is absolutely dependent on the action of ADH.
- 22. Regulation of H2O excretion by kidney ADH secretion is triggered by: 1-Rise in plasma osmolality,which are detected by hypothalamic osmoreceptors. 2-Decrease in ECF volume: This is detected by baroreceptors. The osmoreceptors mechanism is the most important for minute to minute control of ADH secretion. ADH increases water reabsorption by the collecting duct and therefore minimizes water loss.
- 23. FORCES AFFCTING EXCHANGE OF BODY FLUIDS 1-Diffusion: It is the net movement of particles through the cell membrane from high concentration to low concentration. Also from positively charged ions to negatively charged ions i.e. diffusion governed by either chemical or electrical gradient. -Net movement of particle /unit time =flux.
- 24. FORCES AFFCTING EXCHANGE OF BODY FLUIDS II-Filtration: It is forced passage of fluid through a membrane due to difference in the hydrostatic pressure on the two sides. -The rate of filtration depends on the pressure difference, surface area of the membrane and its permeability
- 25. FORCES AFFECTING EXCHANGE OF BODY FLUIDS III-Osmosis: It is the movement of solvent molecules across a membrane to the other side in which there is higher concentration of solute to which the membrane is impermeable.
- 26. FORCES AFFECTING EXCHANGE OF BODY FLUIDS IV-Active transport: It is the transport of particles from low concentration to high concentration across the cell membrane. This type of transport occurs against the laws of physical chemistry(uphill) it requires energy derived from adenosine triphosphate(ATP).The particles may be transported against chemical, electrical or pressure gradient. good example for active transport is Na+-K+ pump and calcium pump.
- 27. FORCES AFFECTING EXCHANGE OF BODY FLUIDS Mechanisms of fluid exchange: The forces which govern this exchange of fluid between the plasma and the interstitial fluid are: 1-Hydrostatic pressure due to fluid tension within the circulation. 2-The colloid osmotic pressure of the plasma proteins.
- 28. FORCES AFFECTING EXCHANGE OF BODY FLUIDS The hydrostatic pressure is much higher in the capillaries than in the tissue spaces and tends to drive fluid out of the capillaries by filtration. The osmotic pressure is much higher in the blood plasma than in the interstitial fluid and tend to draw back into the capillaries by osmosis. These two forces act in opposite directions.
- 29. FORCES AFFECTING EXCHANGE OF BODY FLUIDS While the osmotic pressure is uniform throughout the capillary length, the hydrostatic pressure falls from the arteriolar to the venular end. At the arteriolar end of the capillary the hydrostatic pressure is greater than the colloid osmotic pressure and, therefore, fluid tends to pass out of the capillaries. At the venous end of the capillaries, the hydrostatic pressure is less than the colloid osmotic pressure and therefore, H2O is reabsorbed into the capillaries at this end of the capillary.
- 30. FORCES AFFECTING EXCHANGE OF BODY FLUIDS APPLIED PHYSIOLOGY OF TISSUE FLUID EXCHANGE Edema: Edema is defined as the abnormal collection of fluid in the interstitial spaces. There are three main causes which occur frequently in clinical practice: 1-Increased capillary hydrostatic pressure 2-Decrease in the plasma colloid osmotic pressure 3-Obestruction of lymph vessels.
