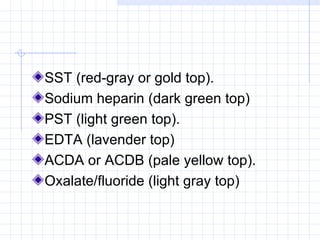
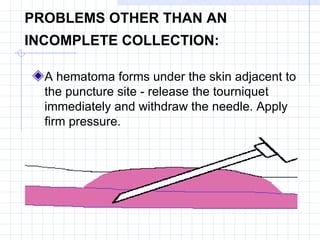
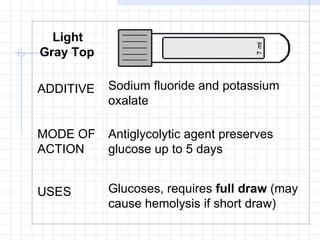
This document provides guidelines for routine venipuncture and specimen handling. It describes the venipuncture procedure, including patient preparation, vein selection, order of draw, labeling samples, and troubleshooting incomplete collections. It also lists the additive, function, and uses of various colored collection tube types, such as red top for chemistries, gold top for serum separation, and purple top for complete blood counts. Complications like hematomas are addressed.