This document discusses retinal artery occlusion. Key points:
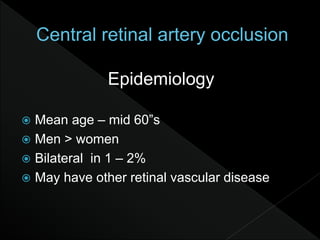
- It typically affects people in their mid-60s and is more common in men.
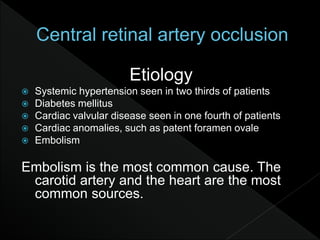
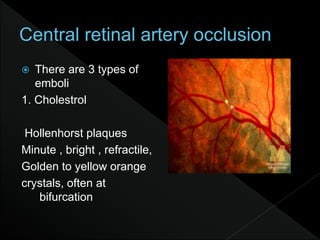
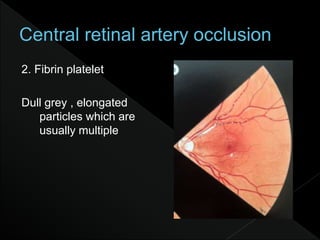
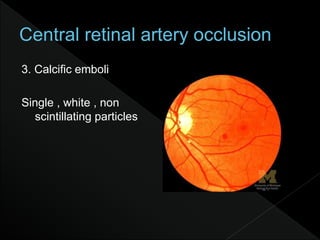
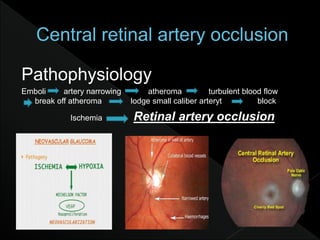
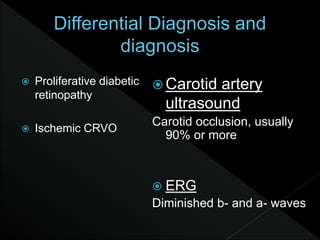
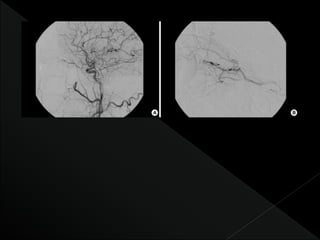
- Embolism, usually from the heart or carotid artery, is the most common cause.
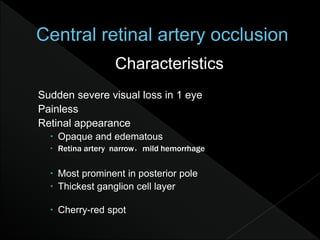
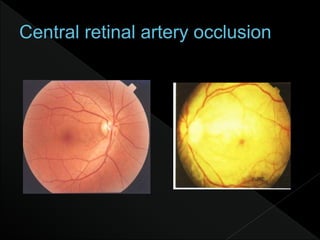
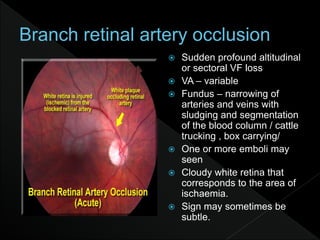
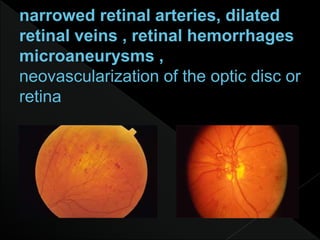
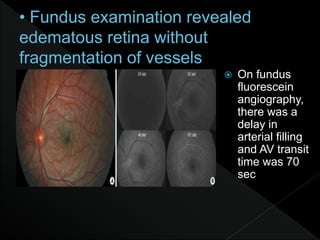
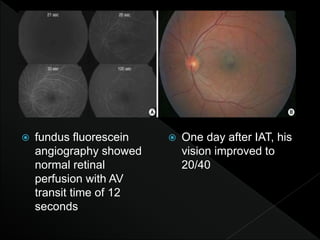
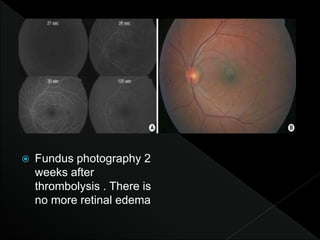
- Symptoms include sudden severe vision loss in one eye. On examination, the retina appears opaque and edematous with a narrowed artery.
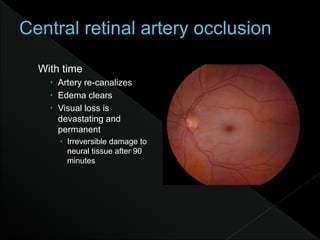
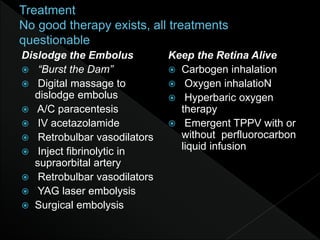
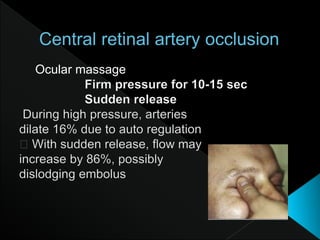
- Visual loss is usually permanent if not treated within 90 minutes. Prompt diagnosis and treatment aimed at dissolving the clot are needed to preserve vision.