This document provides an overview of acetabular fractures including:
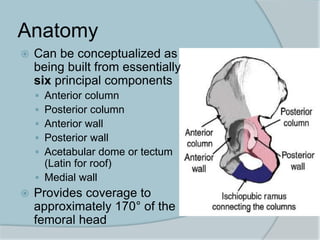
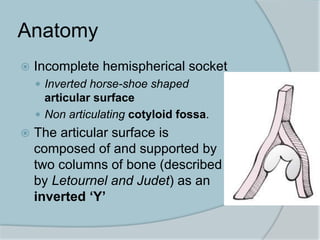
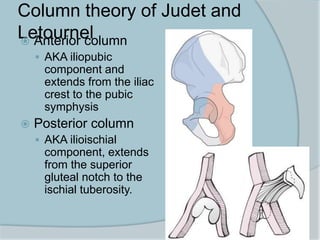
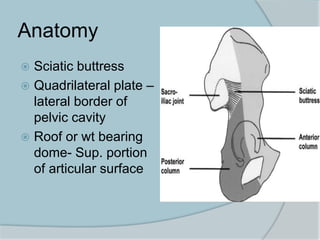
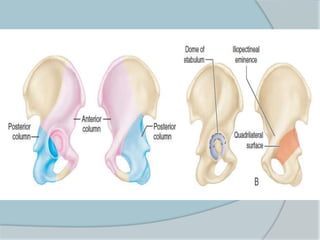
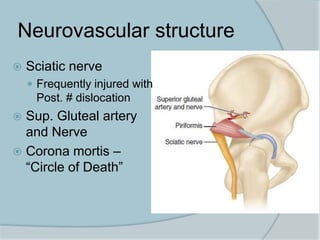
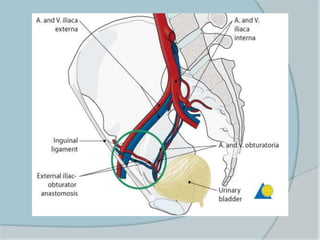
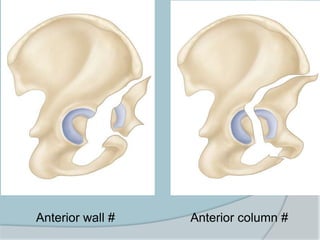
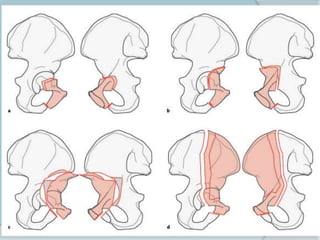
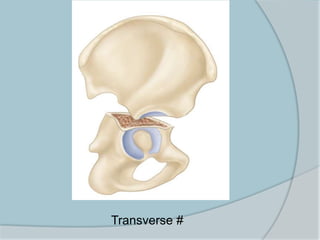
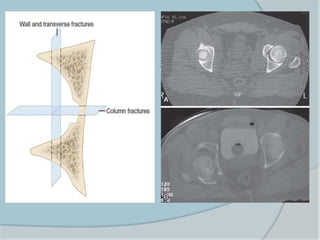
- Anatomy of the acetabulum and its components
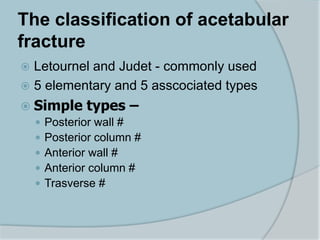
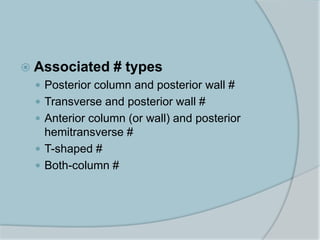
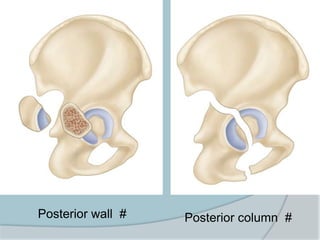
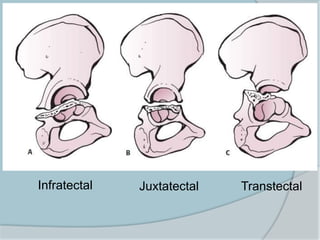
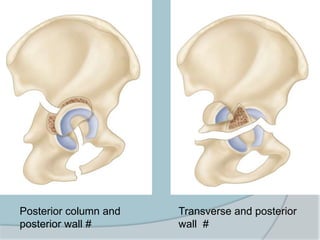
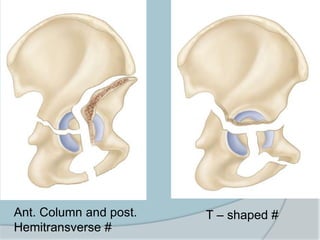
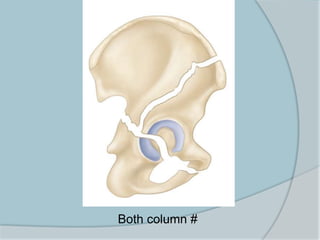
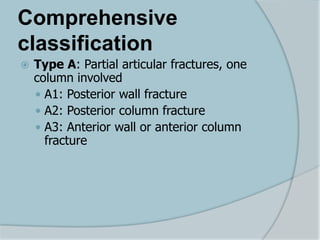
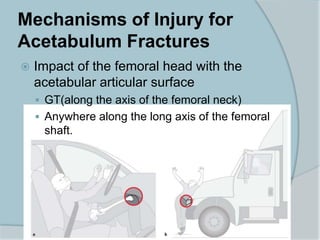
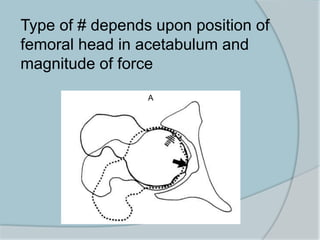
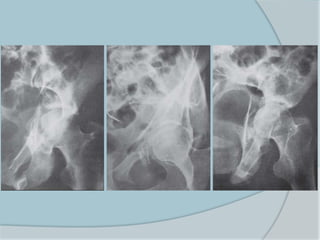
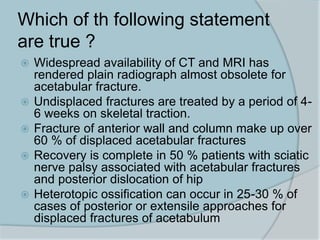
- Mechanisms and classifications of acetabular fractures
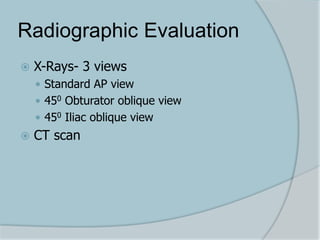
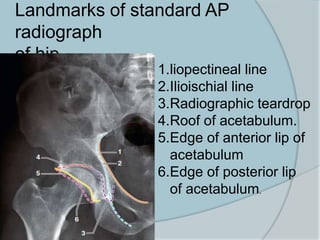
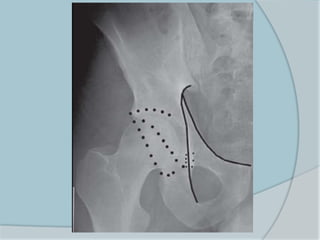
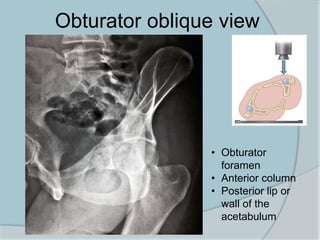
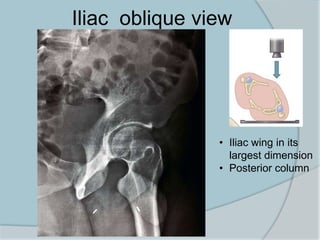
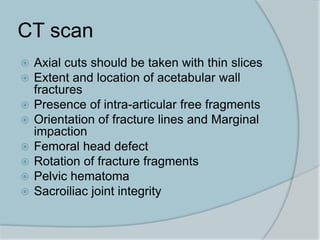
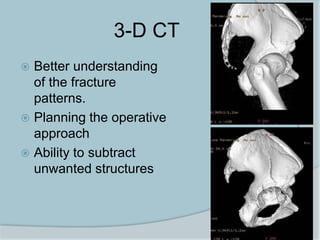
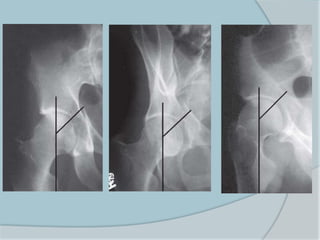
- Evaluation through radiographs and CT scans
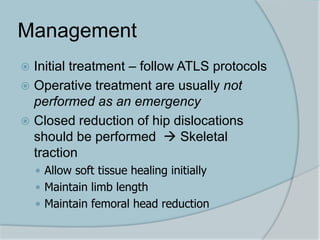
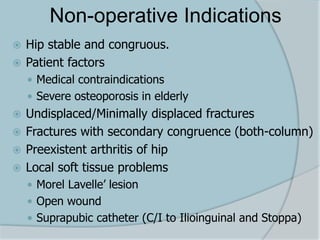
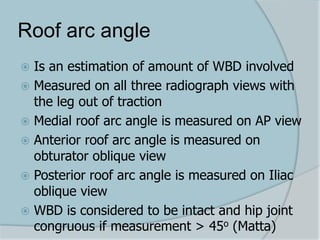
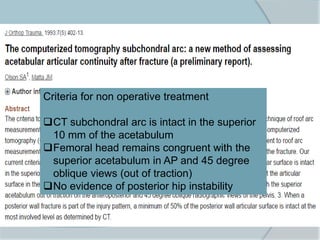
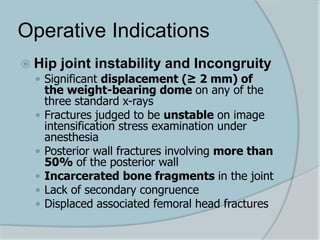
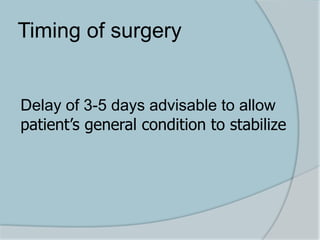
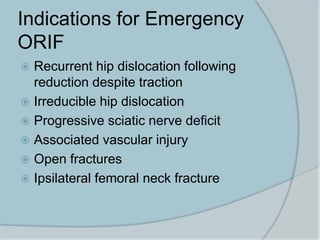
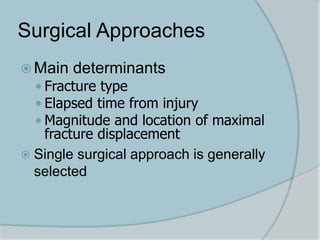
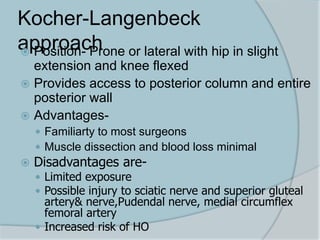
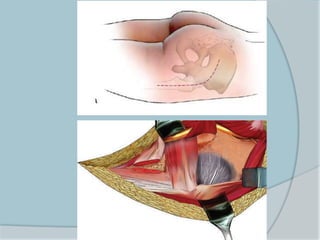
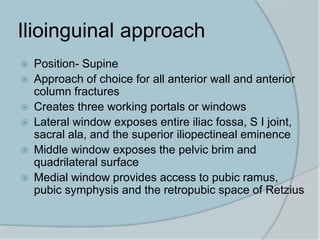
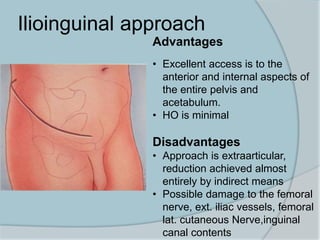
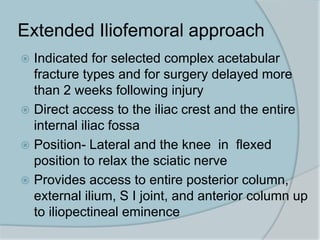
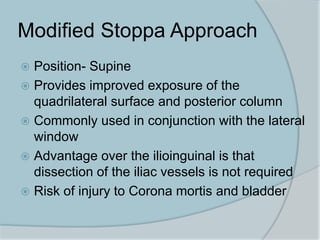
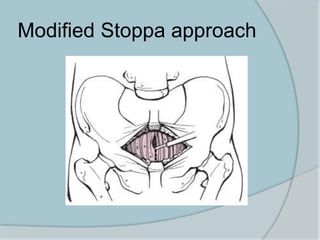
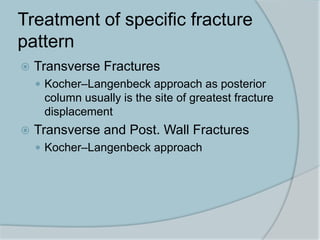
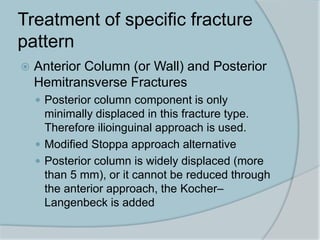
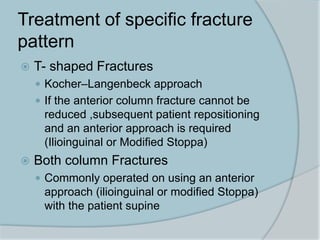
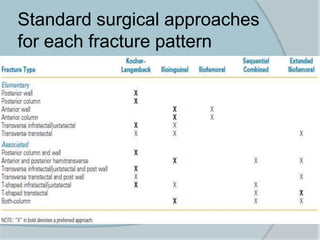
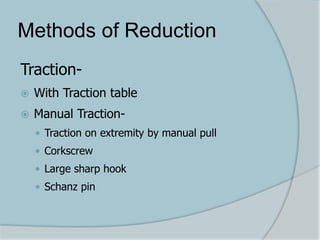
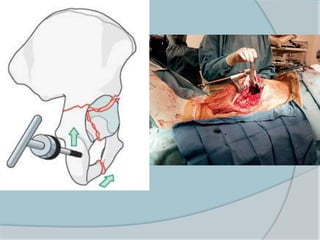
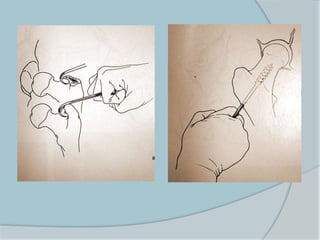
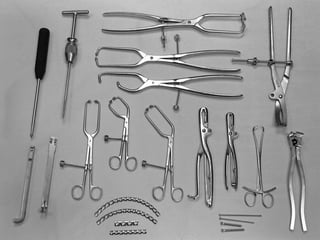
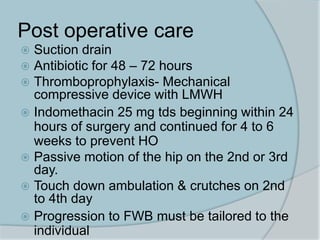
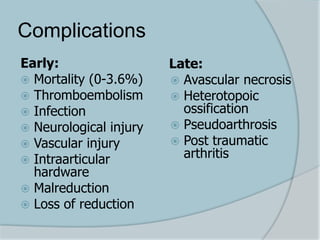
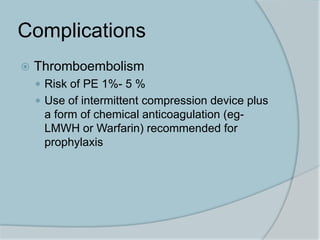
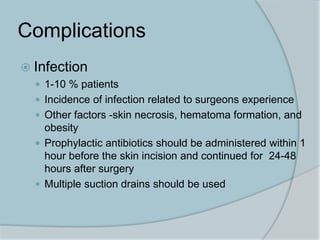
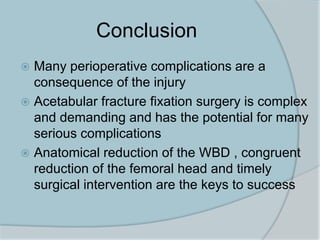
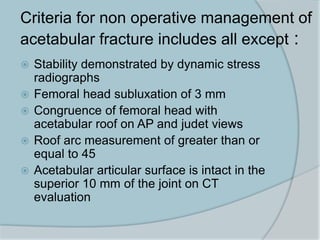
- Management considerations including operative vs non-operative treatment and various surgical approaches
- Specifics on fracture types, indications for surgery, timing of surgery, and surgical approaches for different fractures
The document contains detailed information on evaluating and treating acetabular fractures.