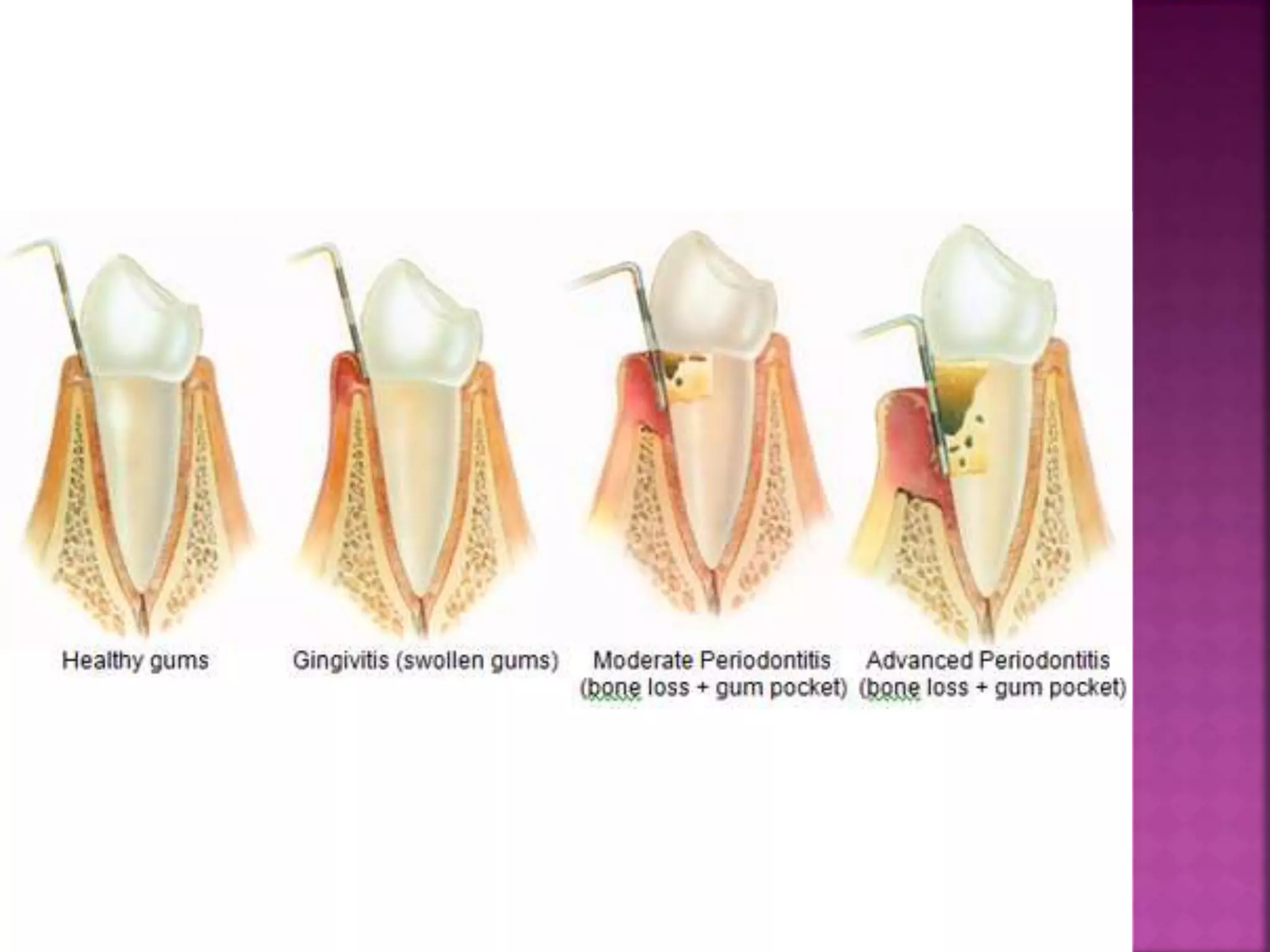
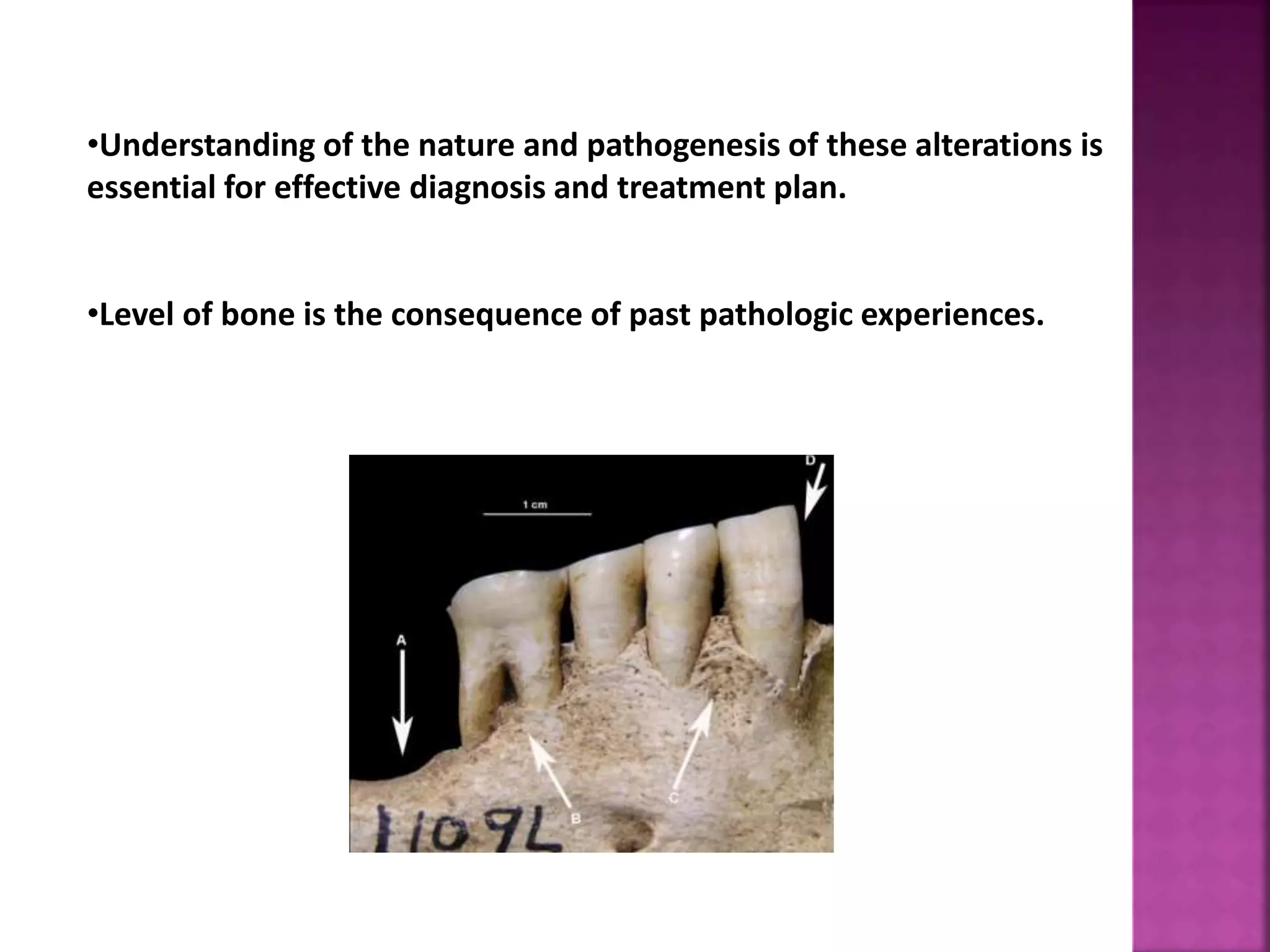
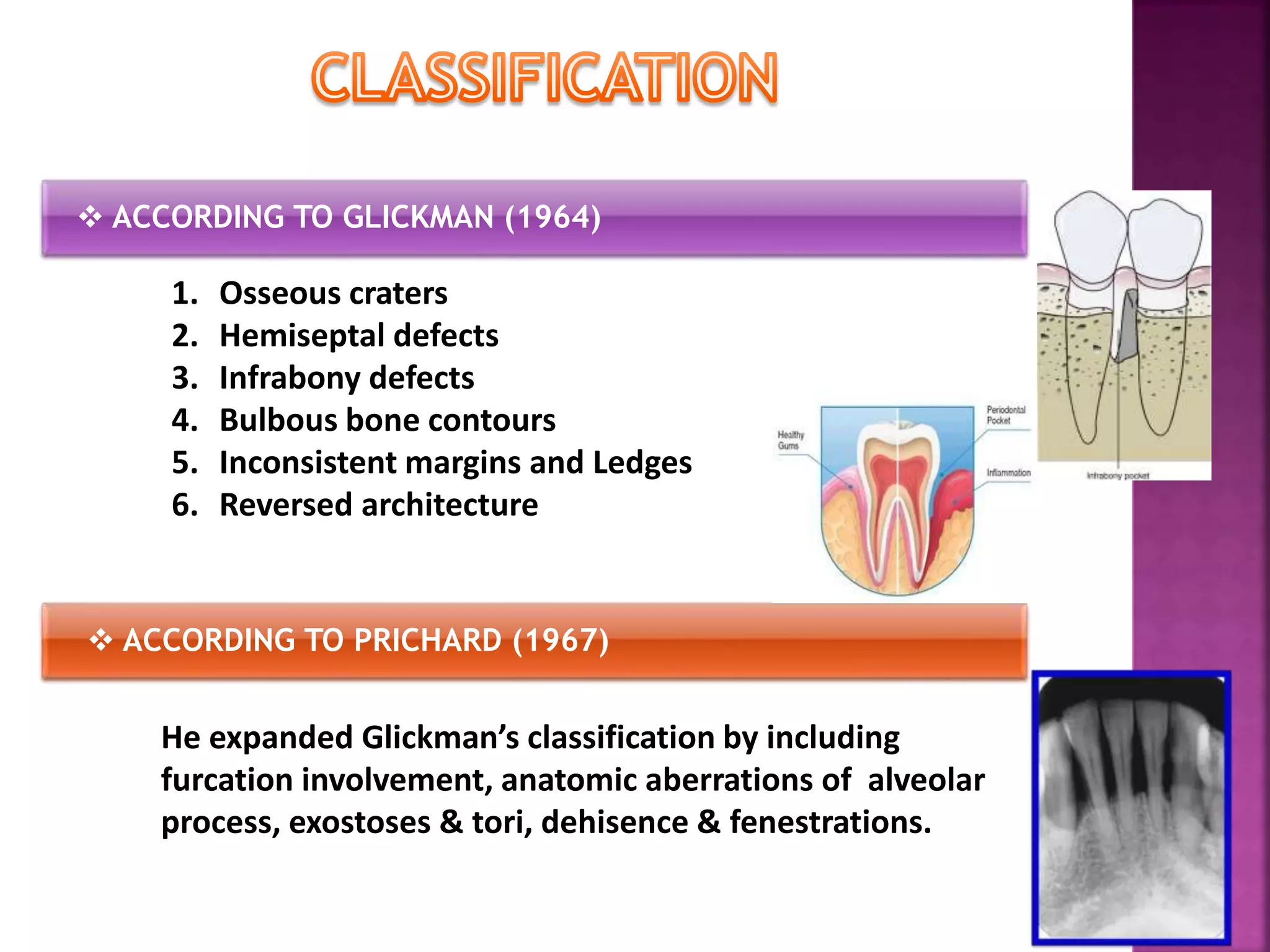
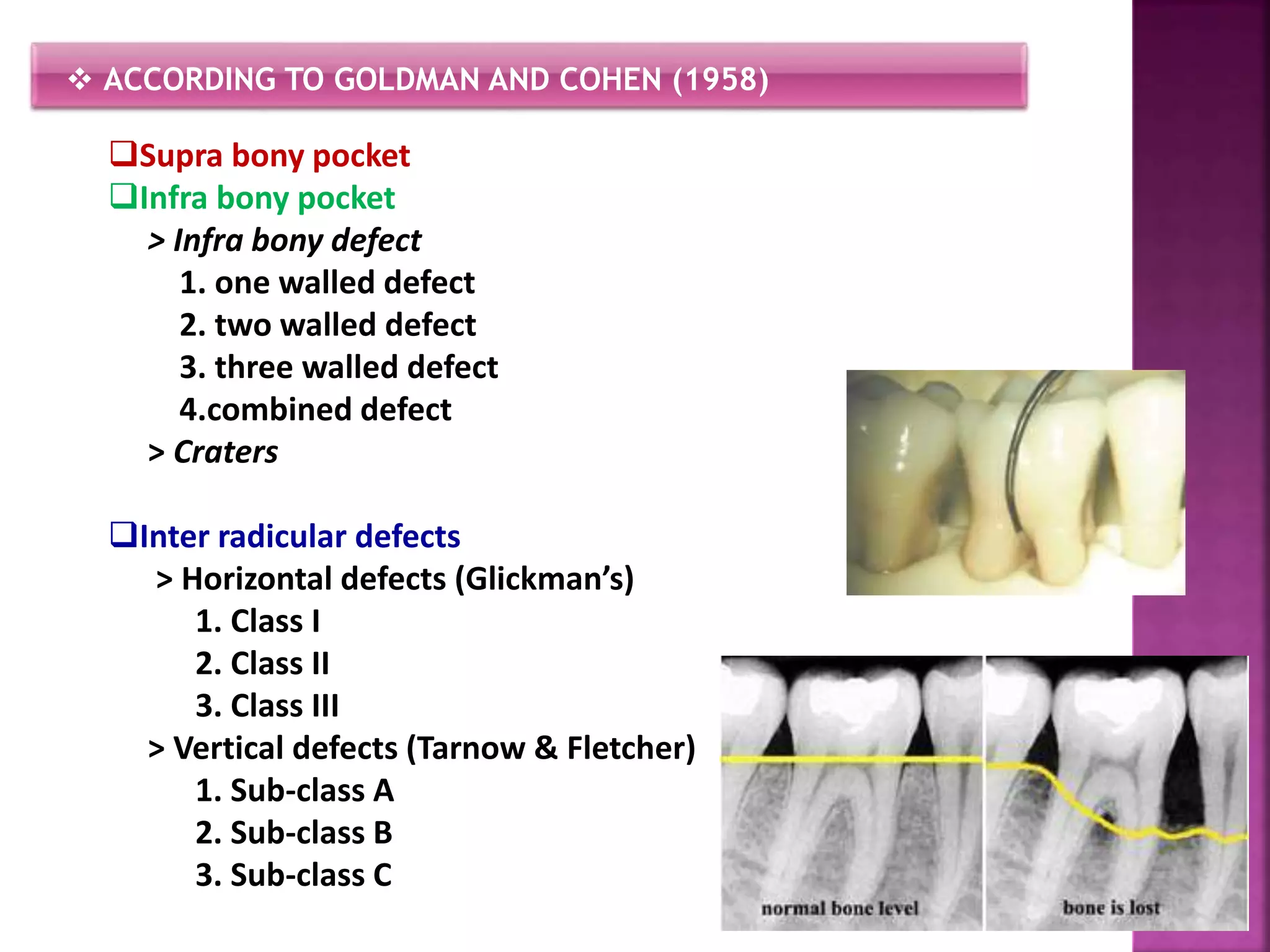
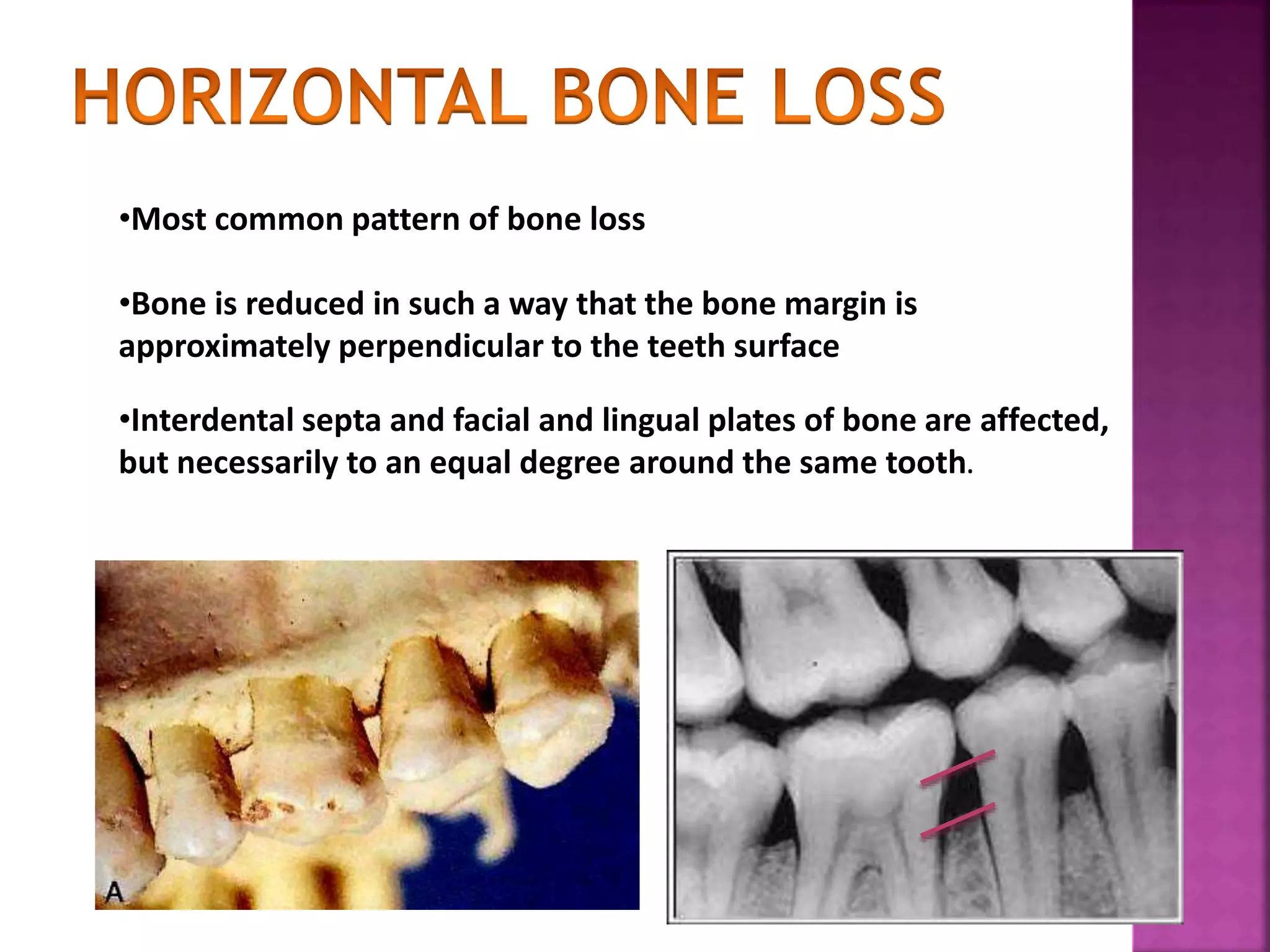
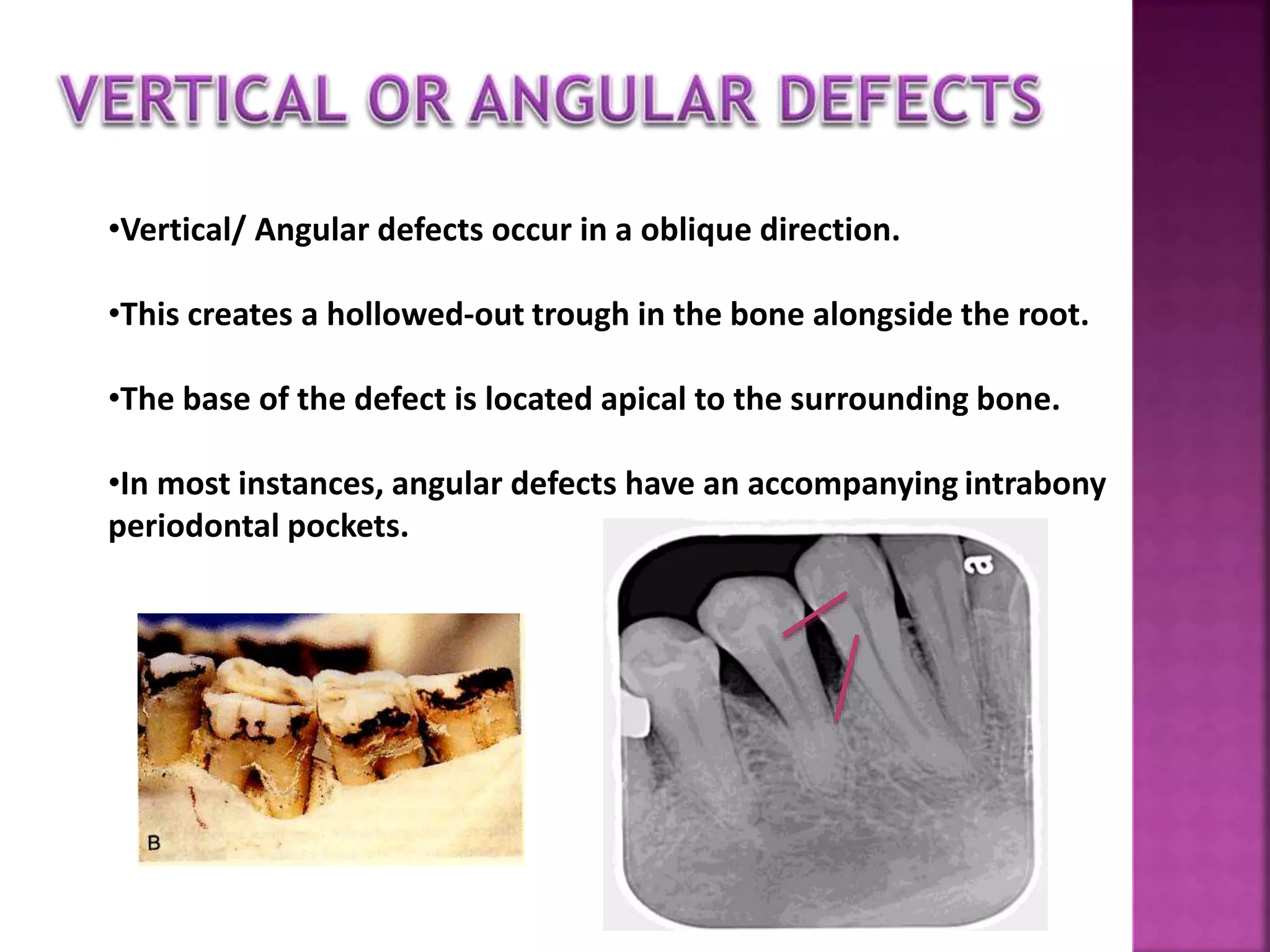
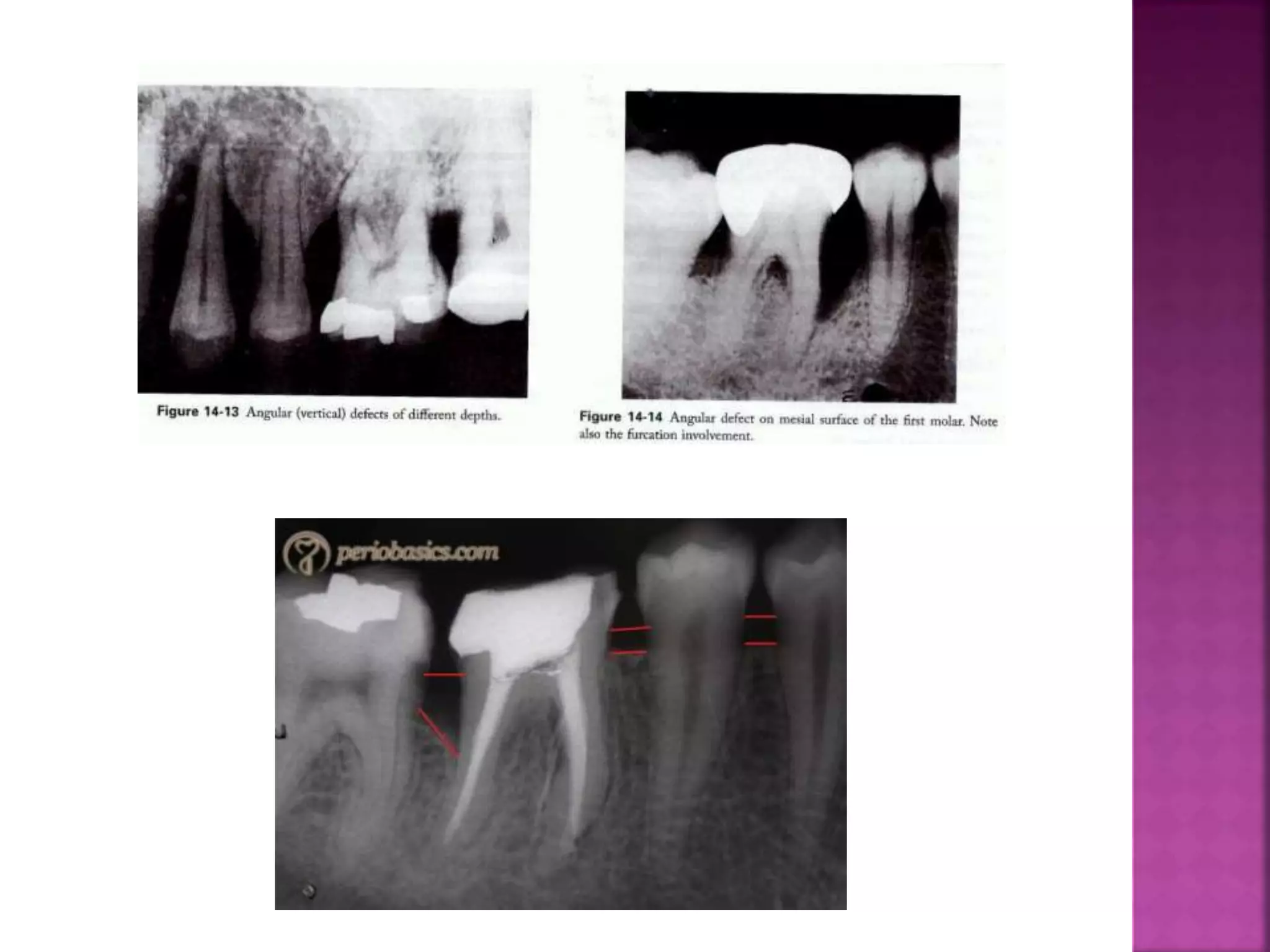
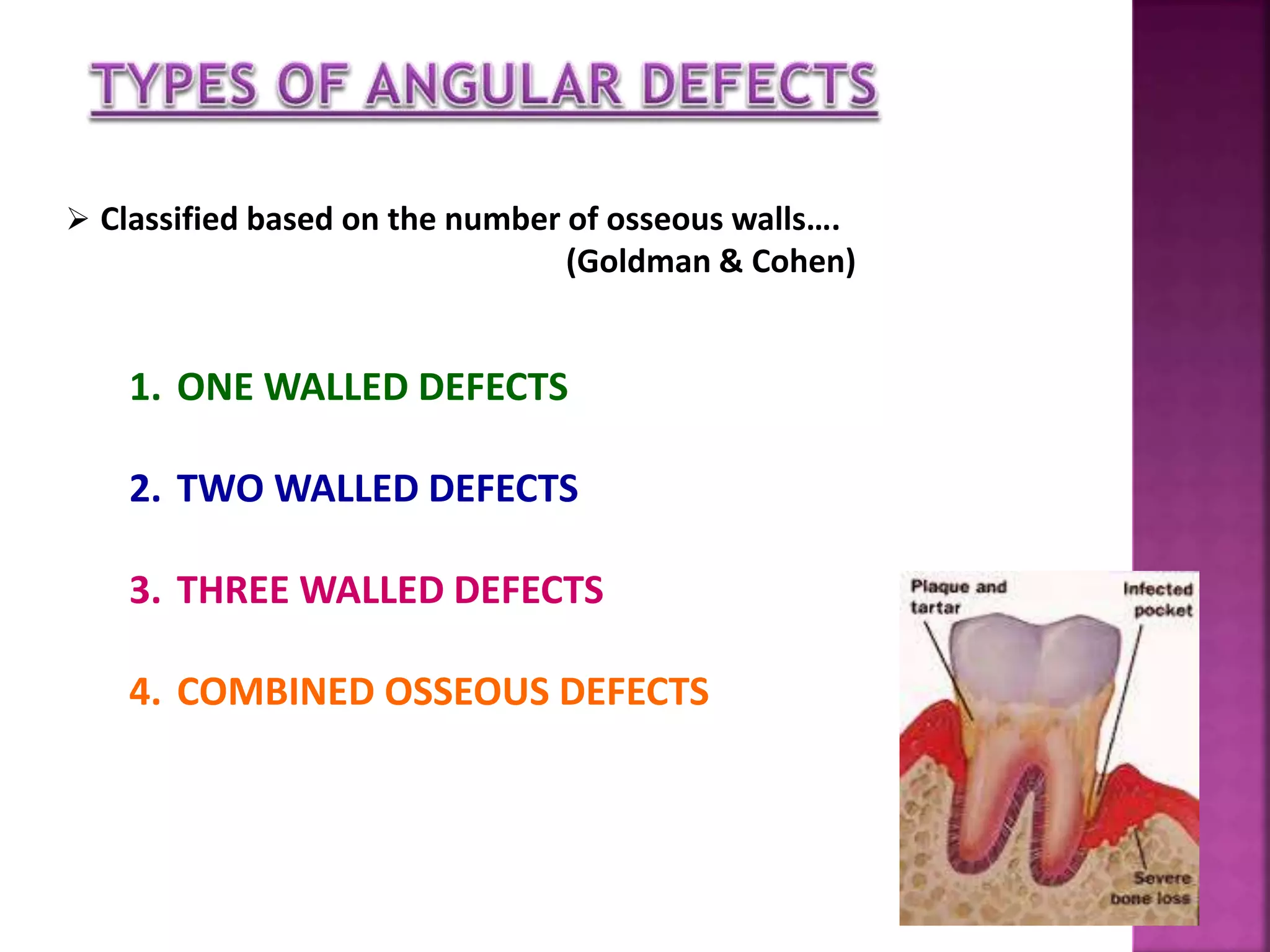
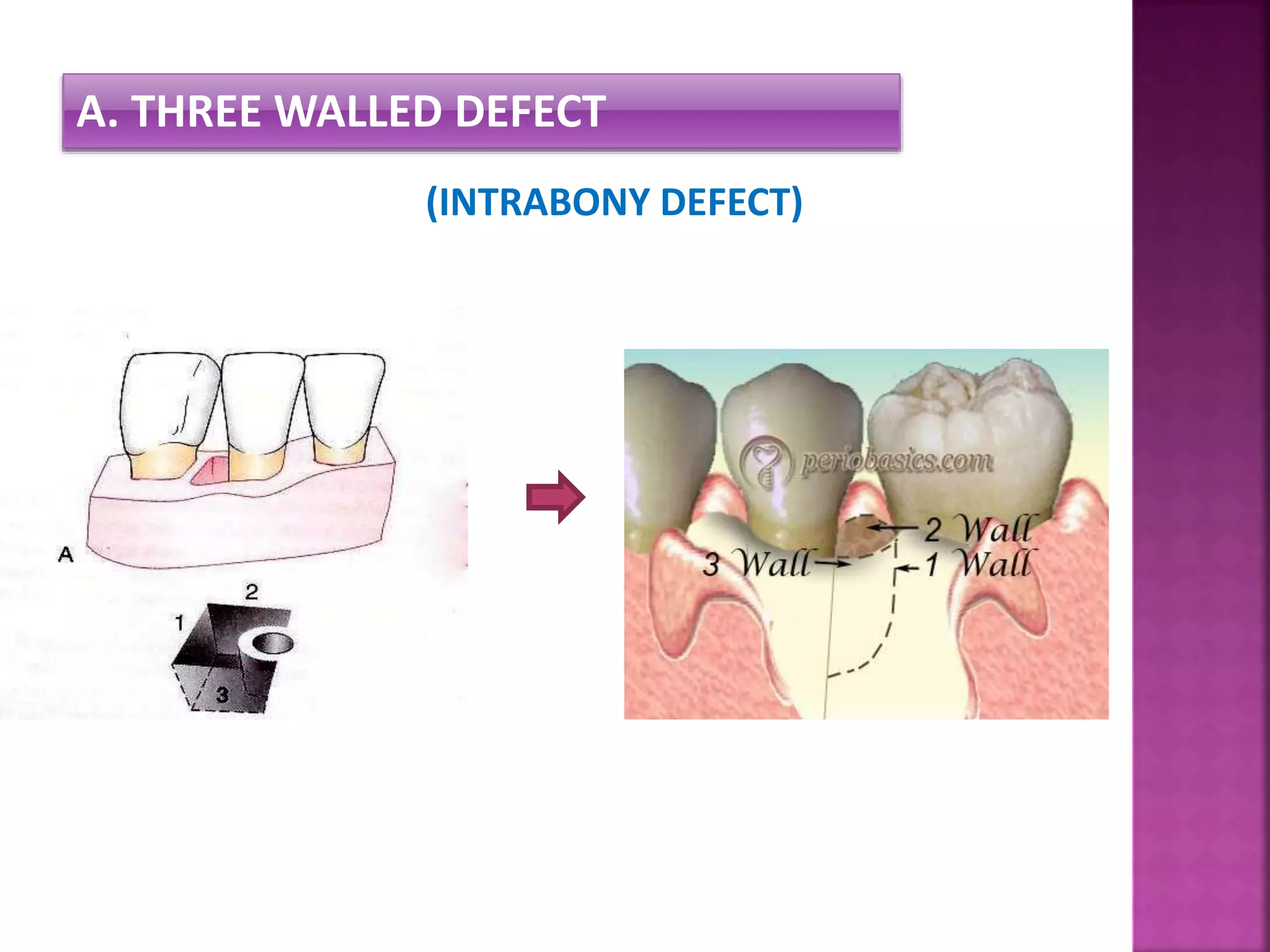
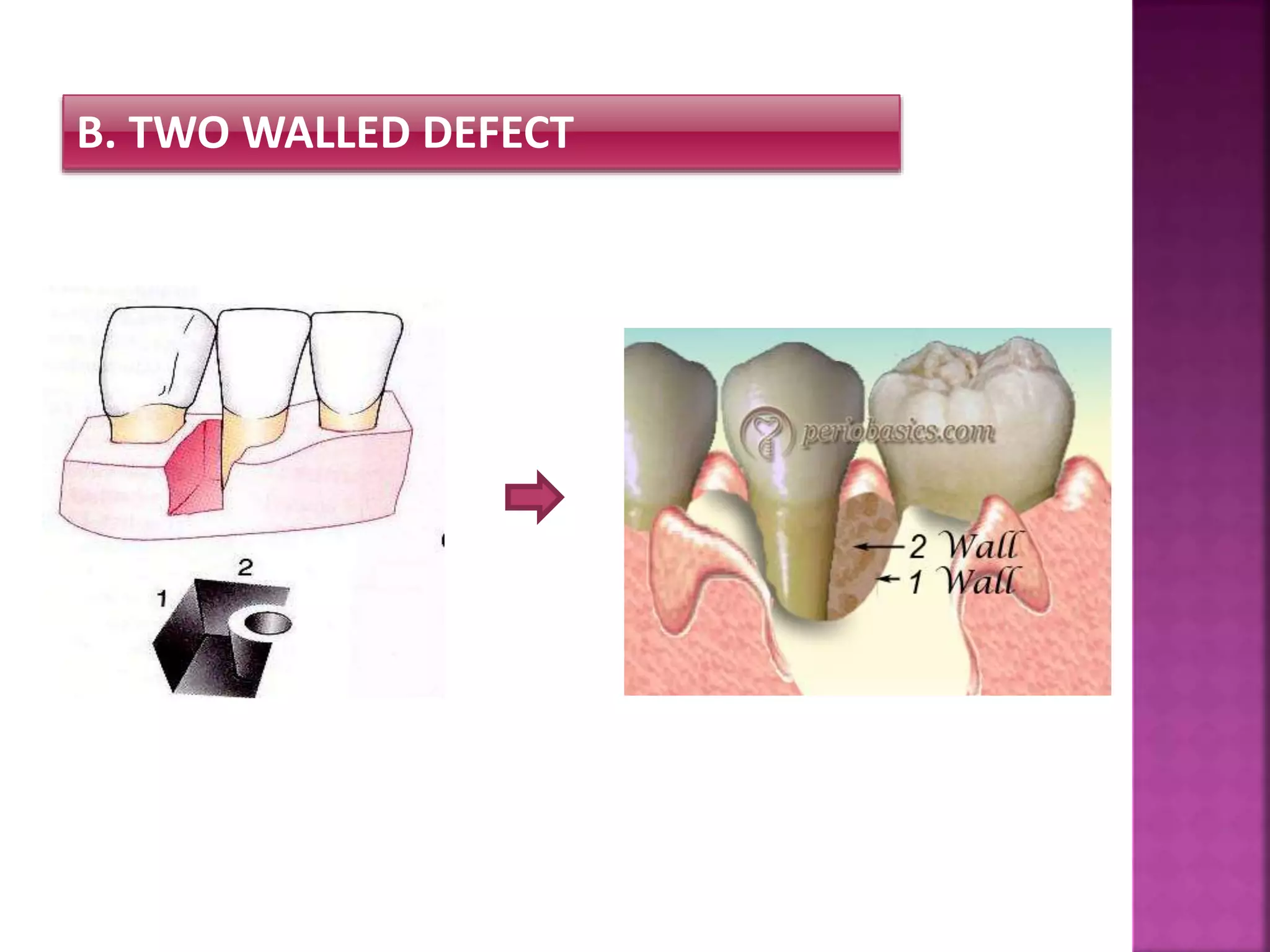
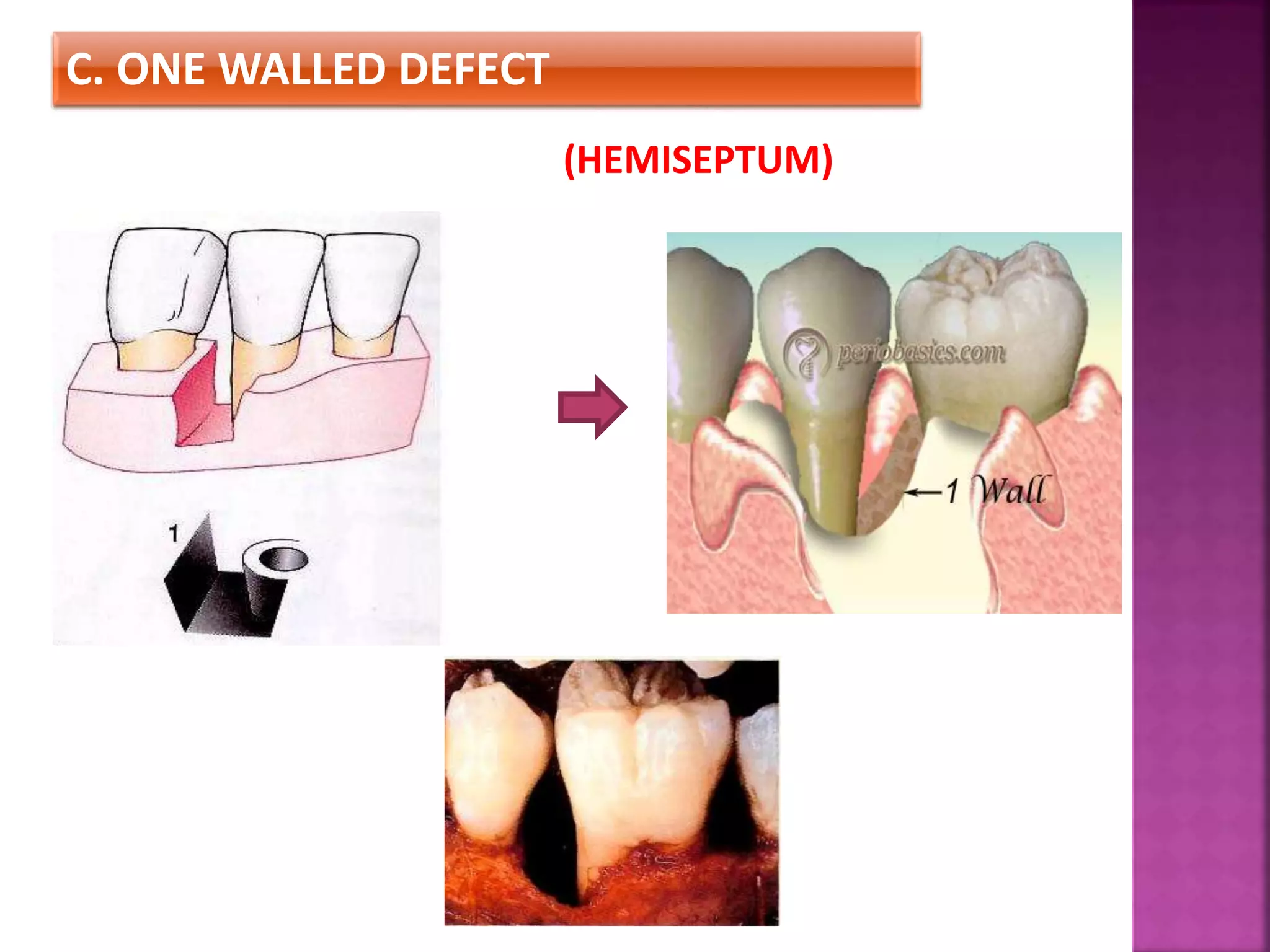
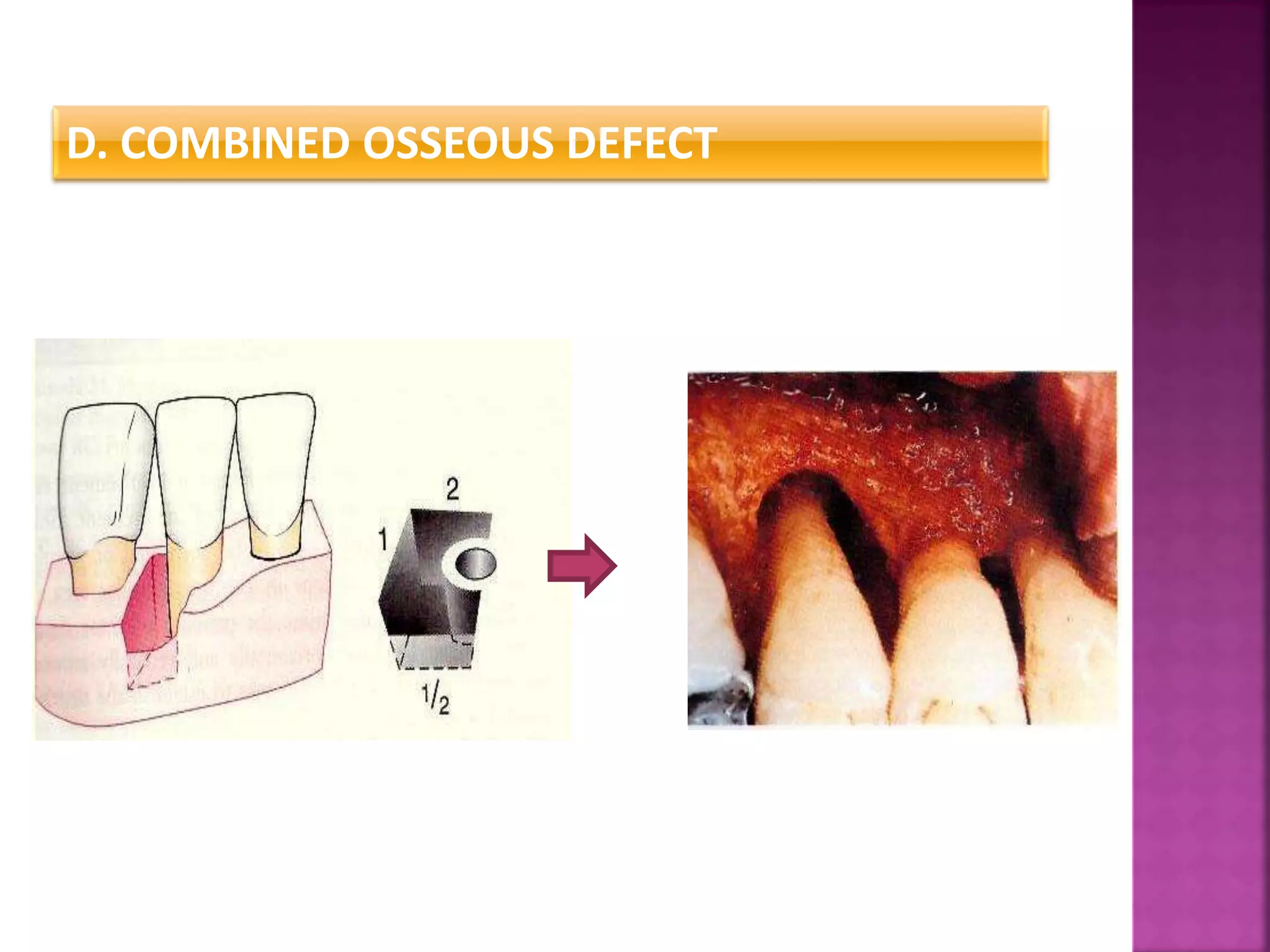
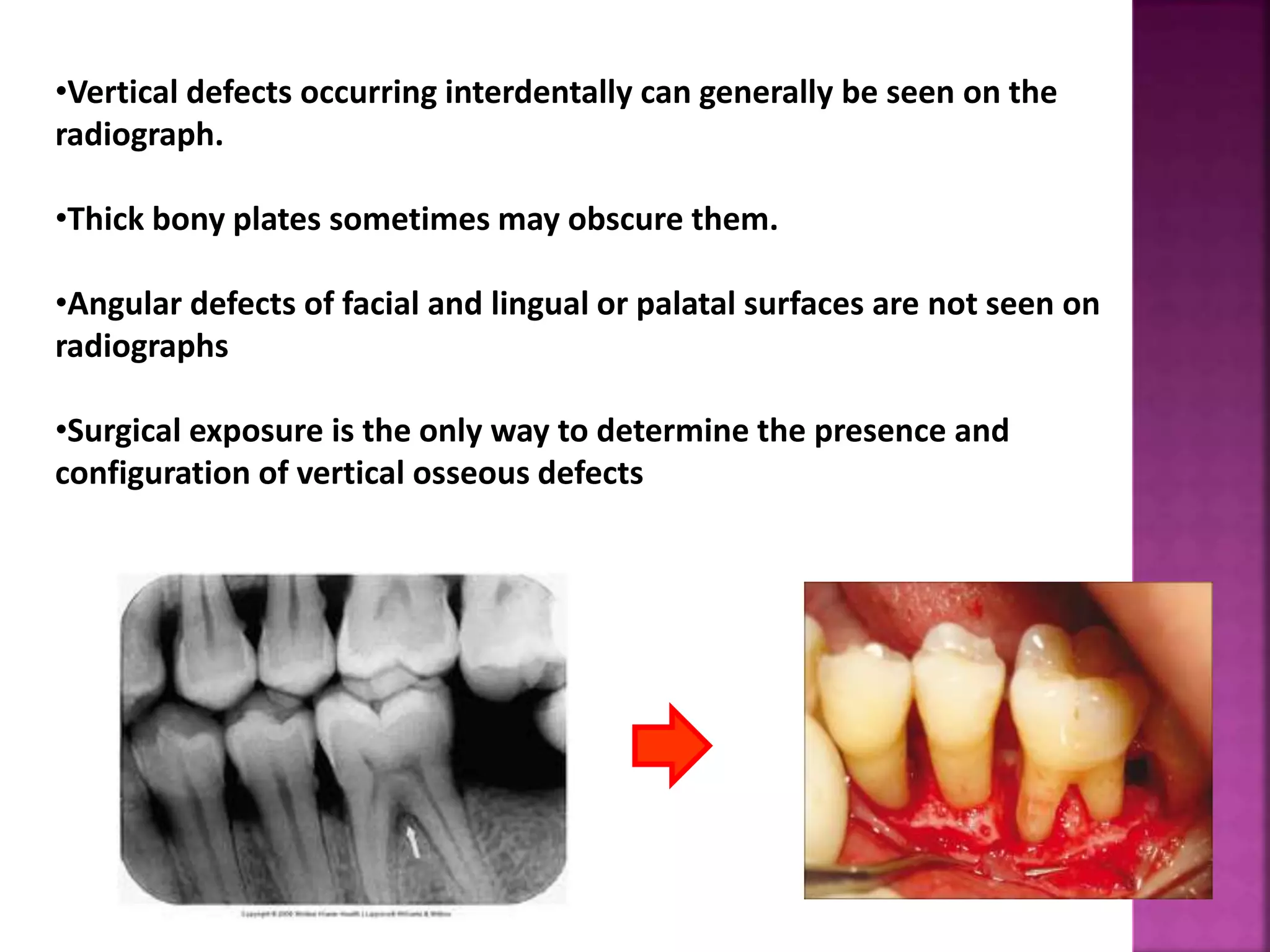
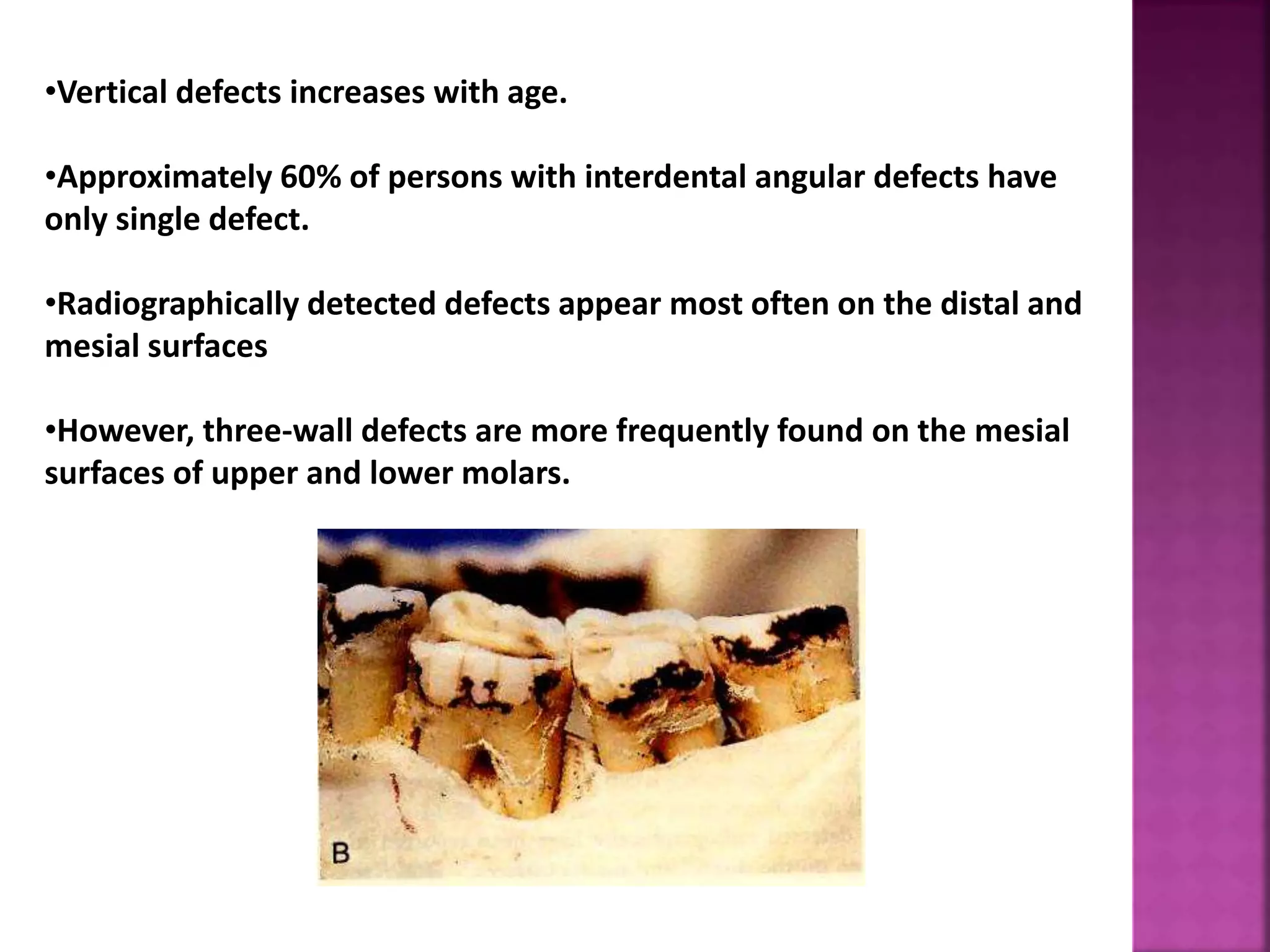
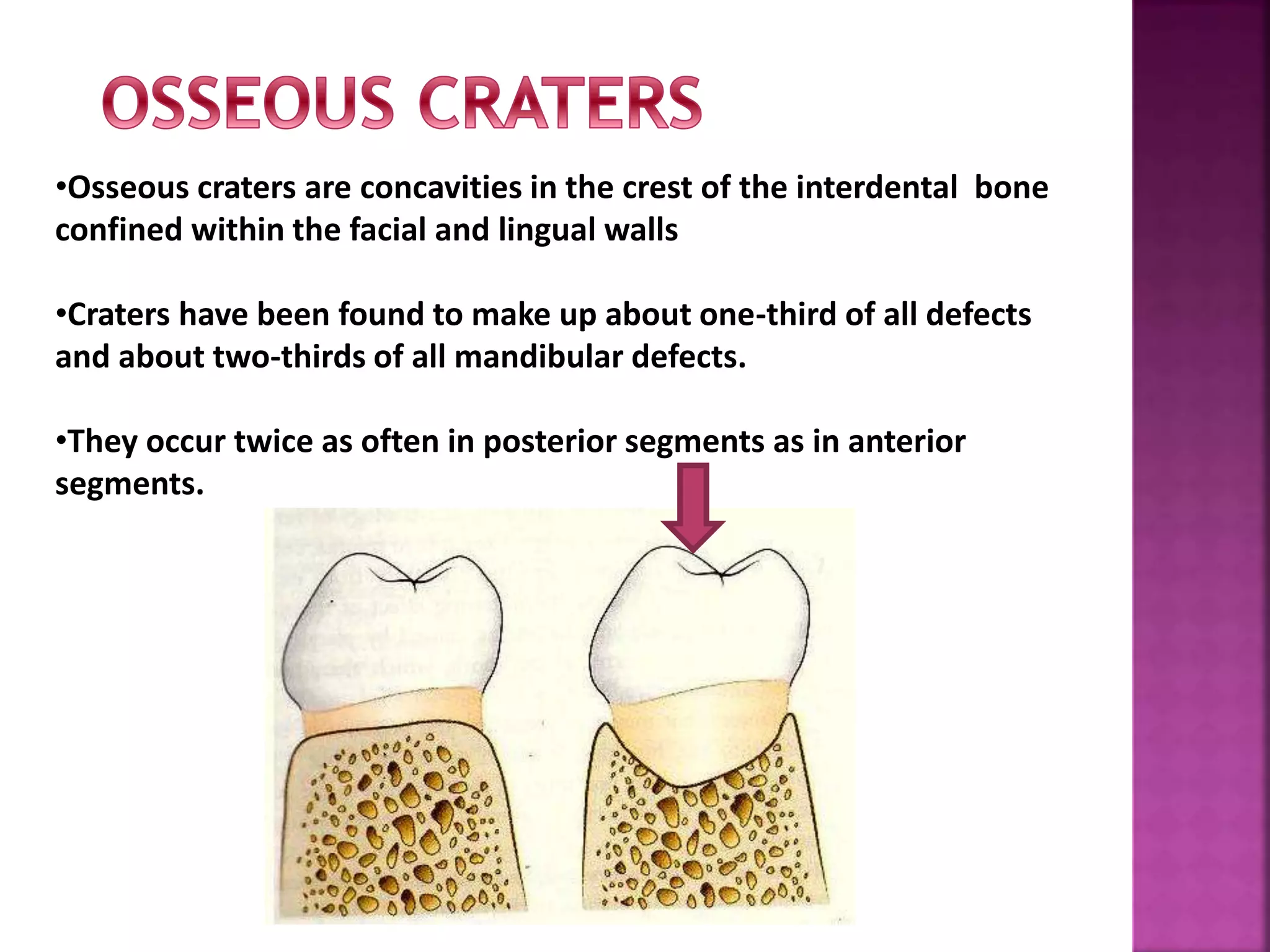
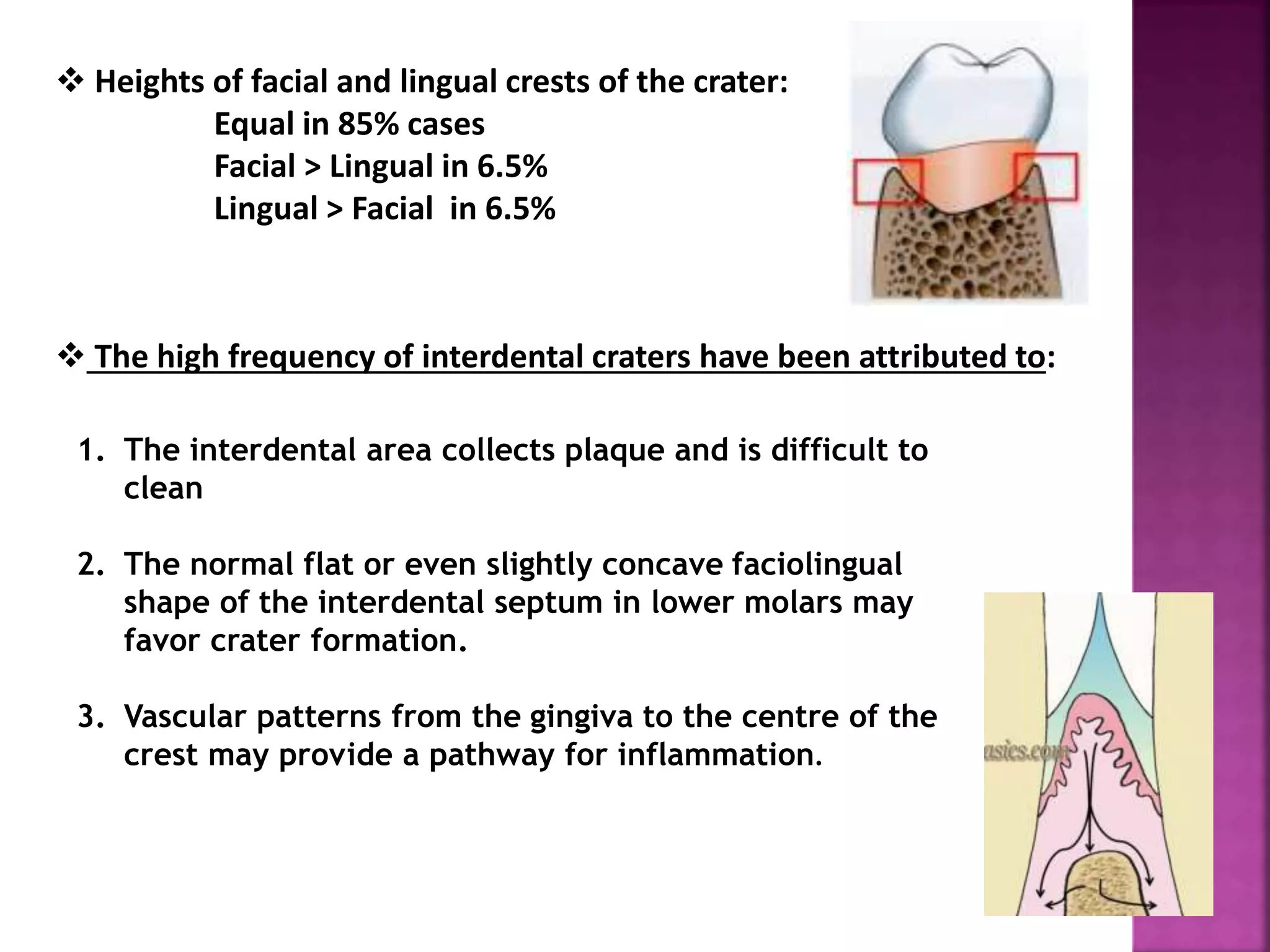
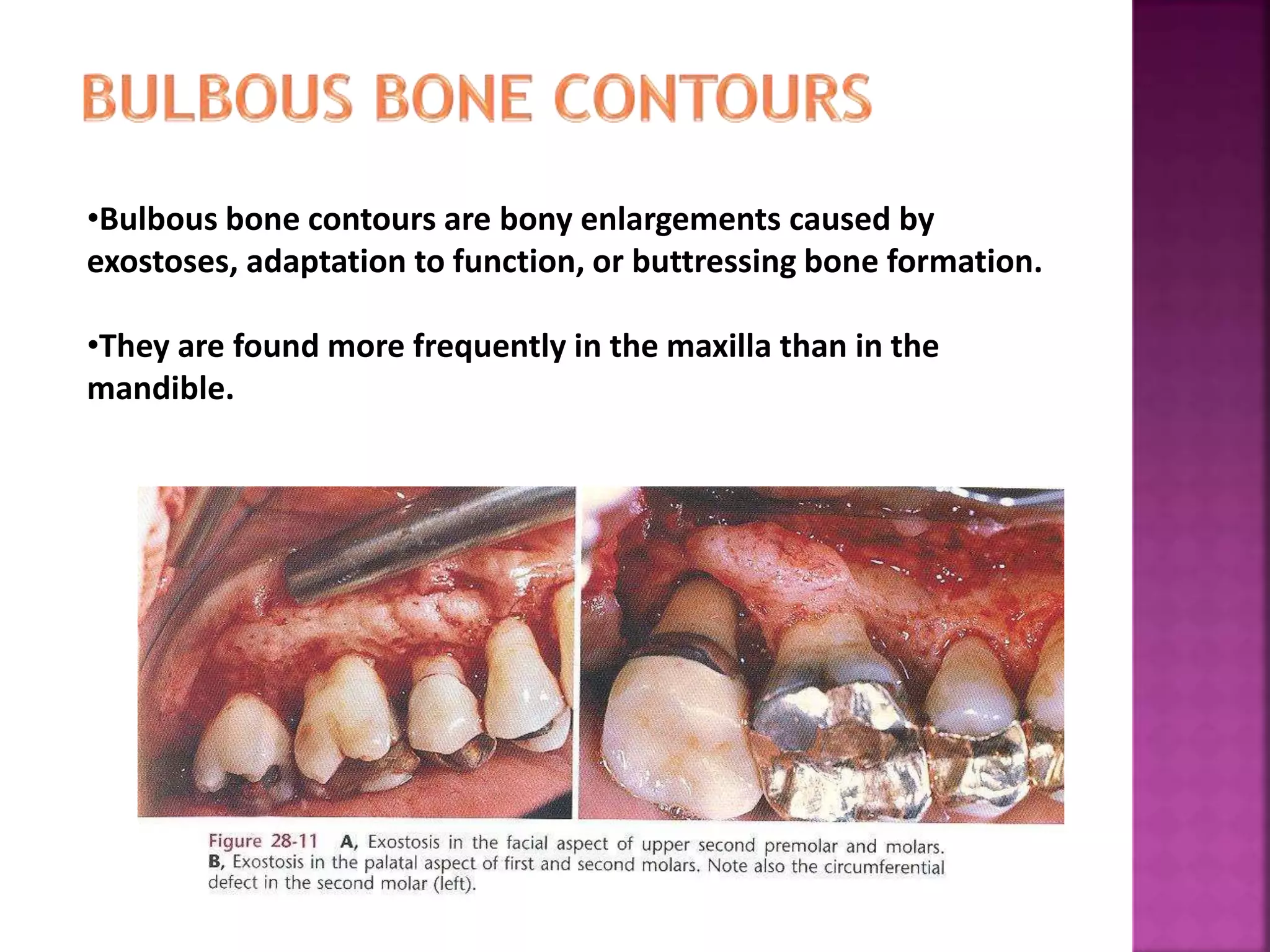
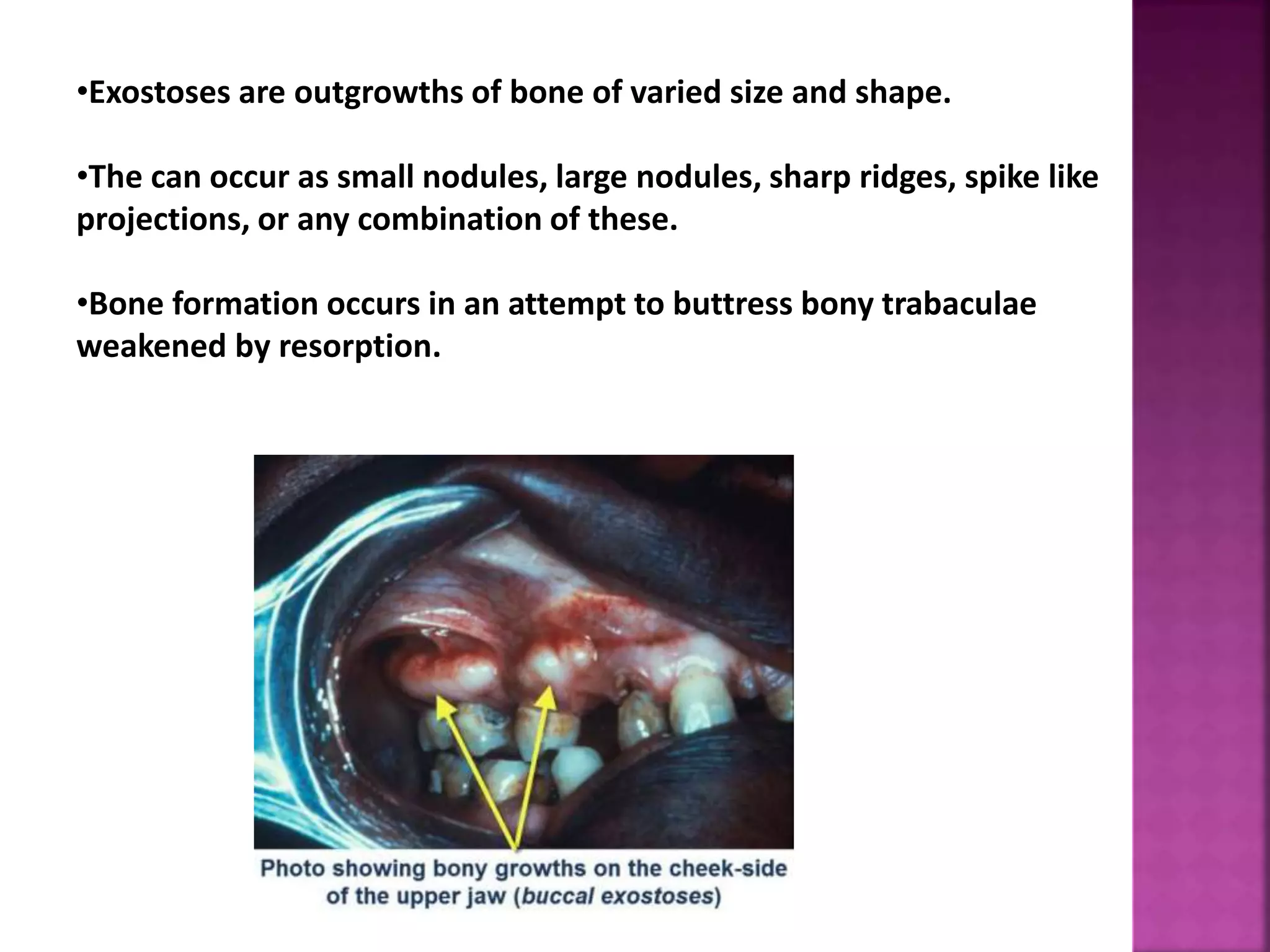
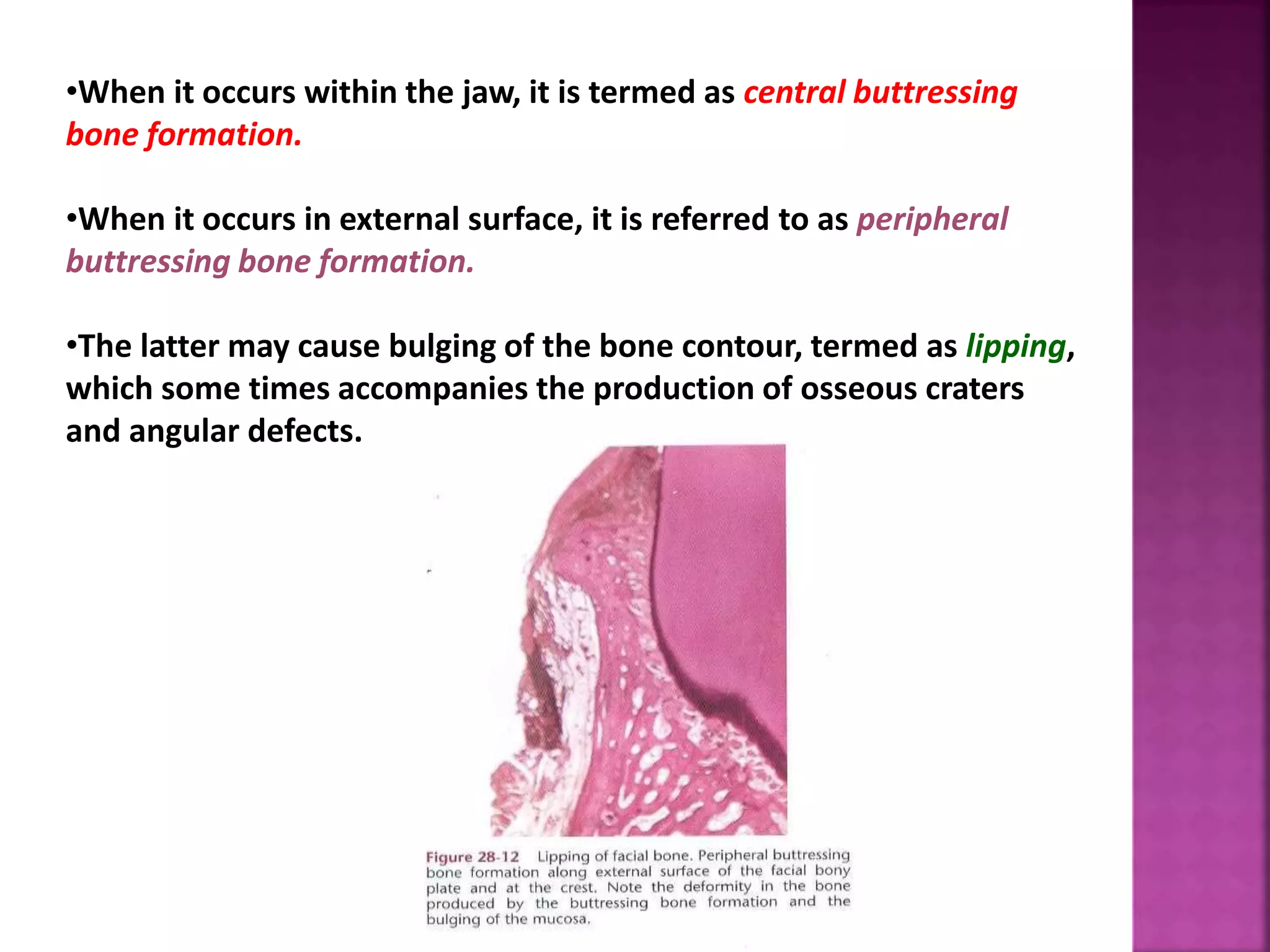
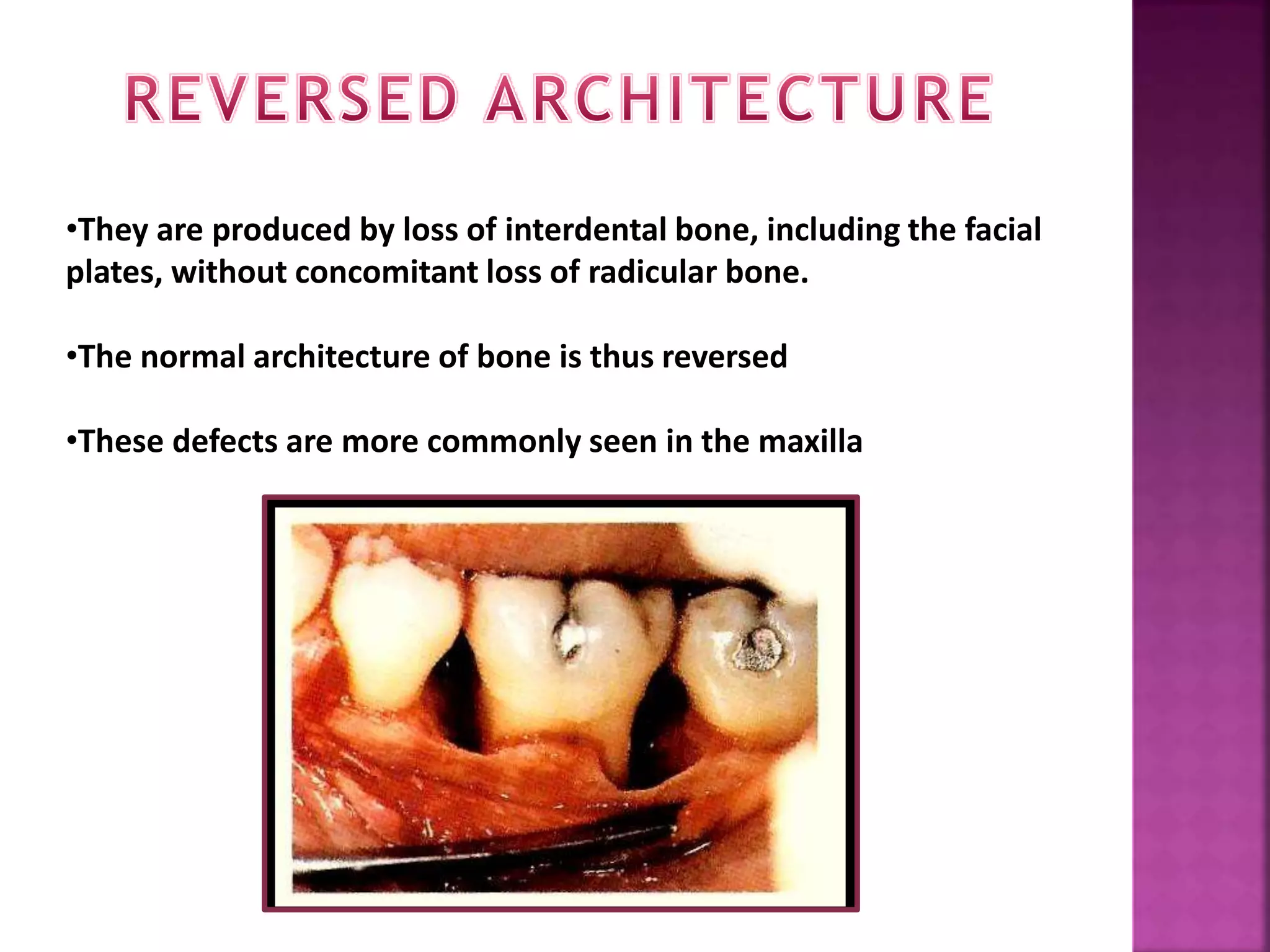
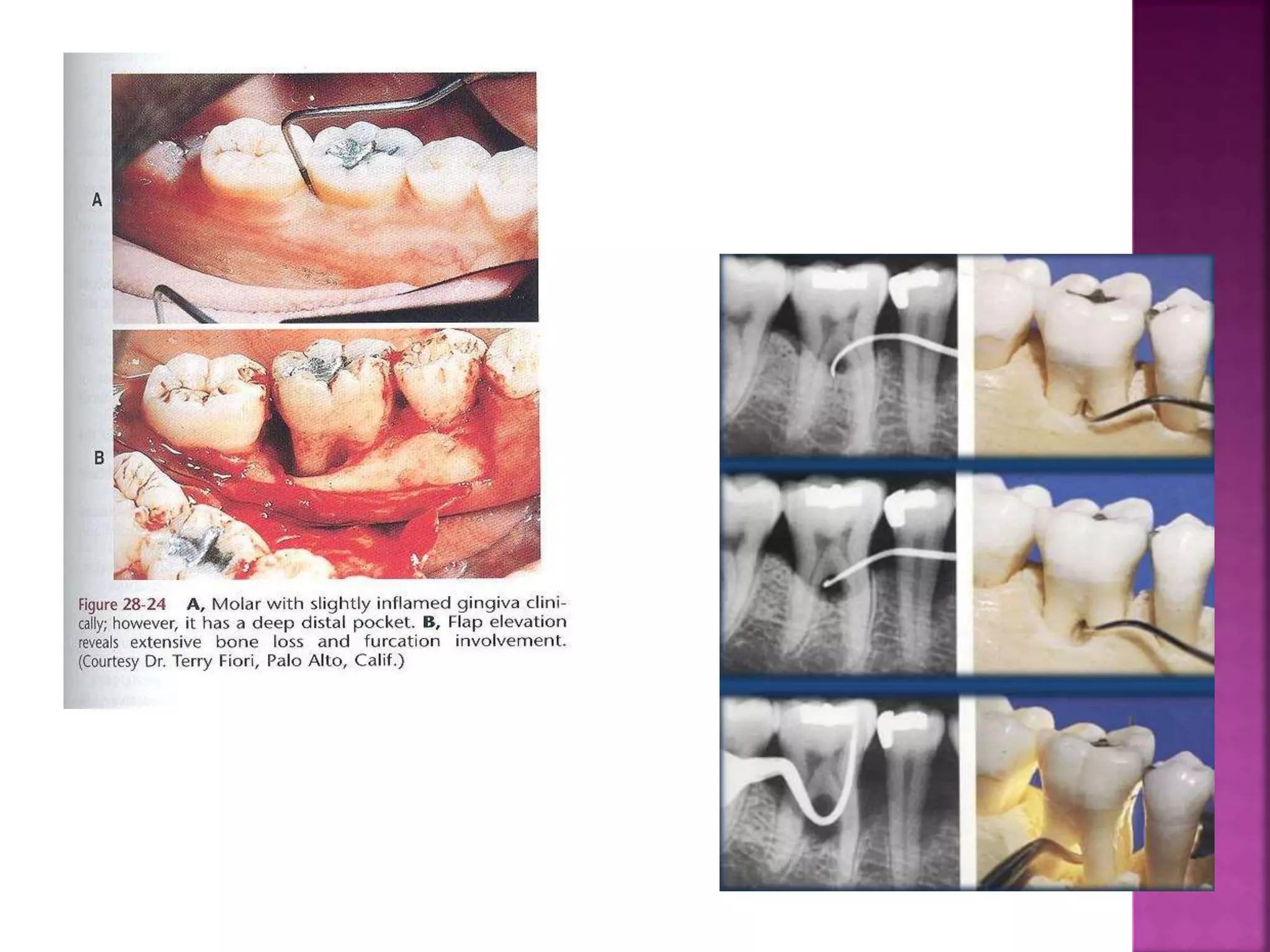
This document summarizes the classification of osseous defects caused by periodontal disease. It describes different types of horizontal bone loss including osseous craters and bulbous bony contours. It also discusses vertical/angular bone loss and classifications proposed by Glickman and Goldman/Cohen. Furcation involvement is classified using scales proposed by Glickman and Tarnow/Fletcher. Understanding the nature of these bone alterations is important for effective diagnosis and treatment planning.