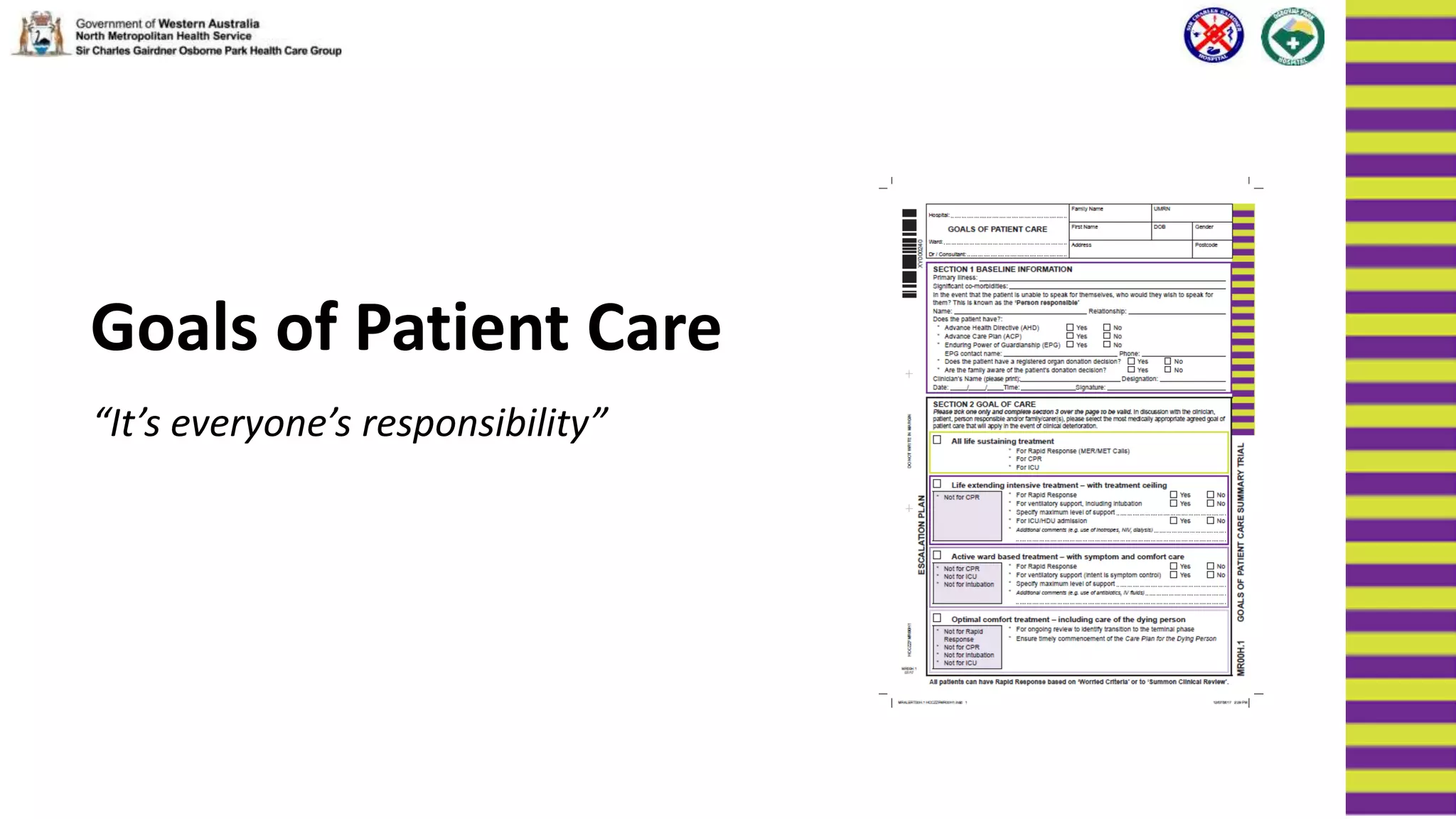
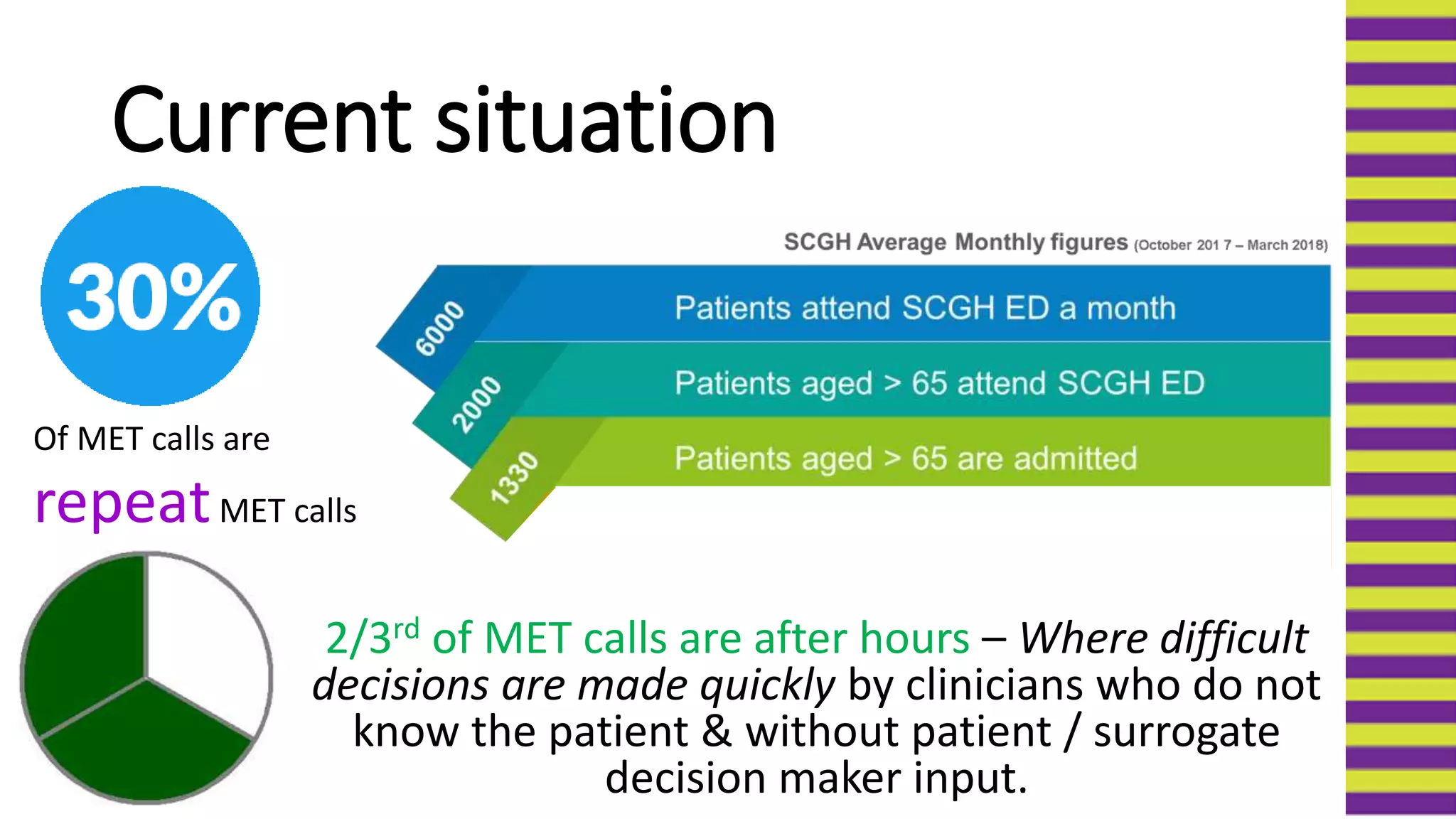
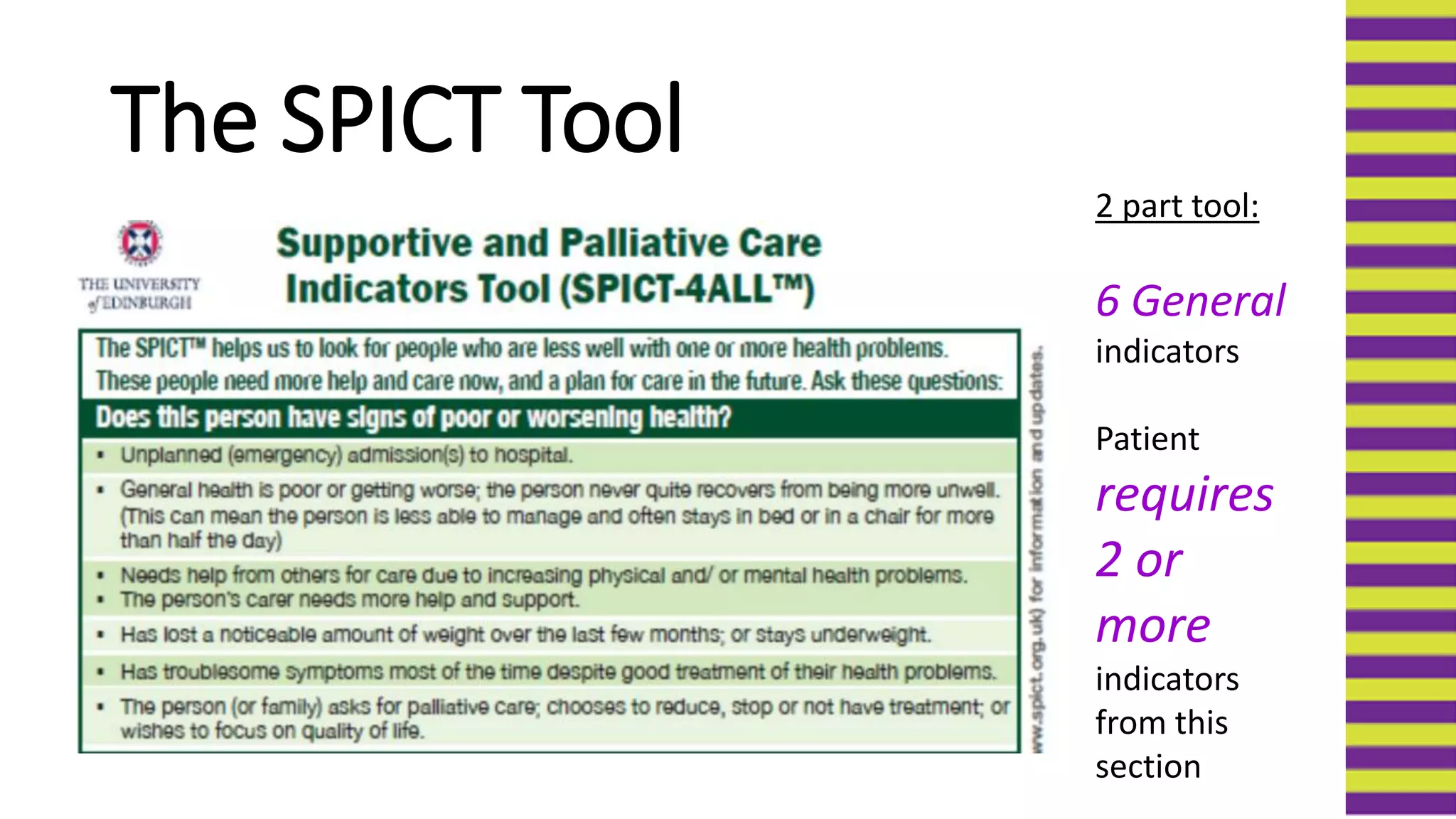
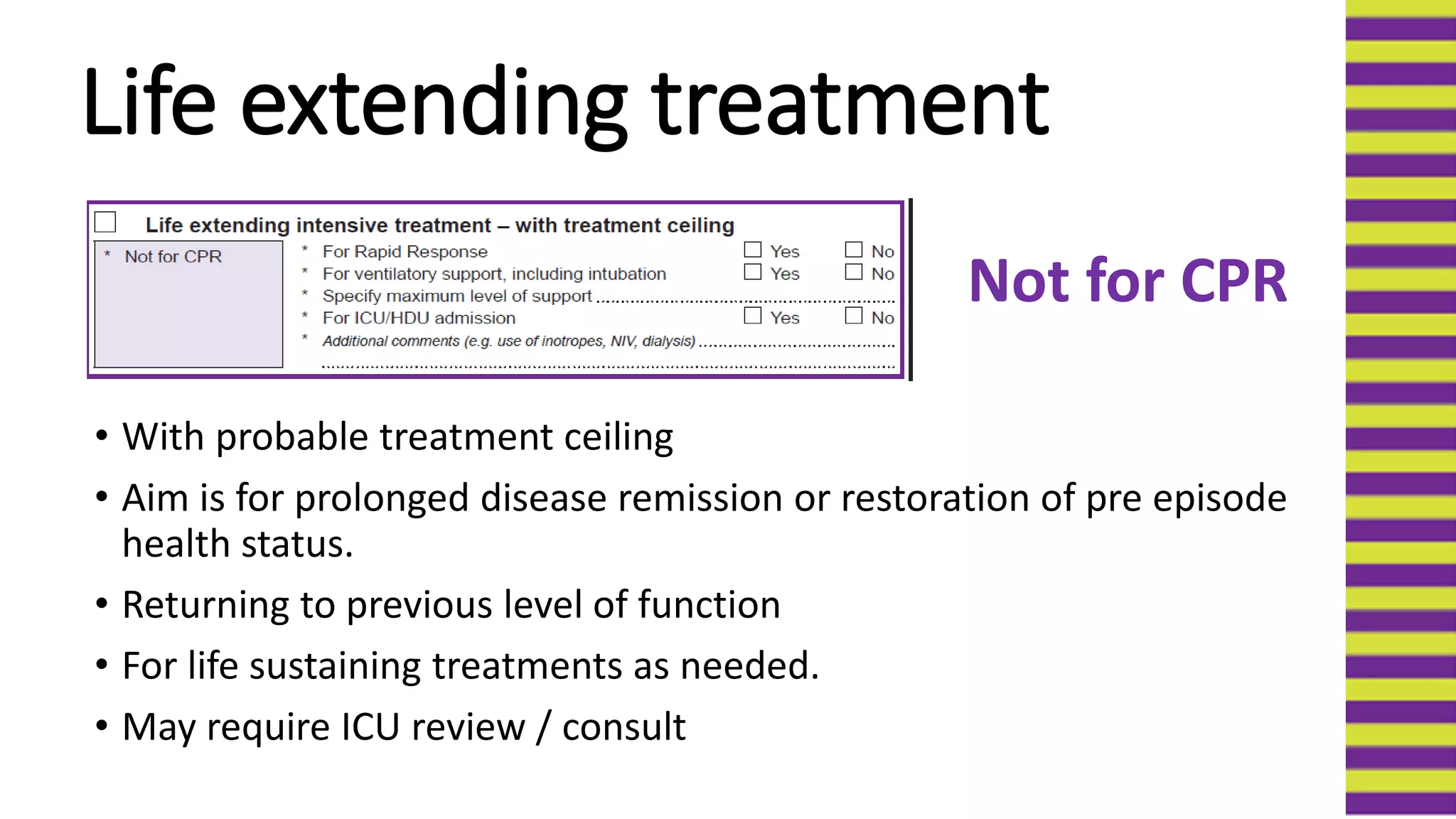
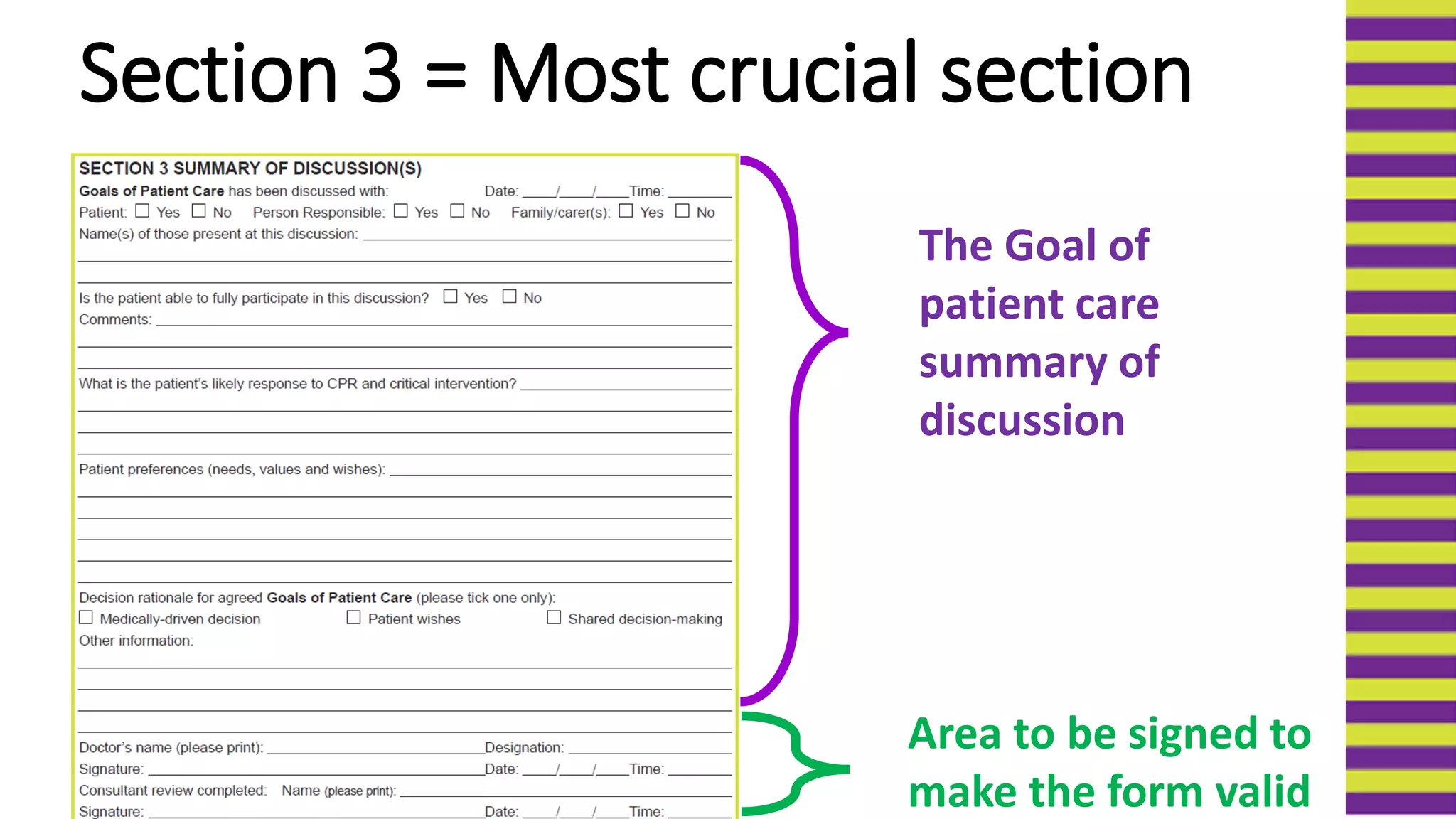
The document discusses the goals of implementing a new Goals of Patient Care (GOPC) form across hospitals in Western Australia to improve end-of-life care and decision making. It provides background on the form's trial implementation at various sites. The new form aims to have goals of care discussions with patients or their surrogates to determine appropriate treatment based on probable outcomes, not just resuscitation status. It outlines the form's structure with sections on baseline information, goal of care selection, discussion summary, and extended use. The document emphasizes improving communication around goals of care and ensuring treatment aligns with patients' values and preferences.